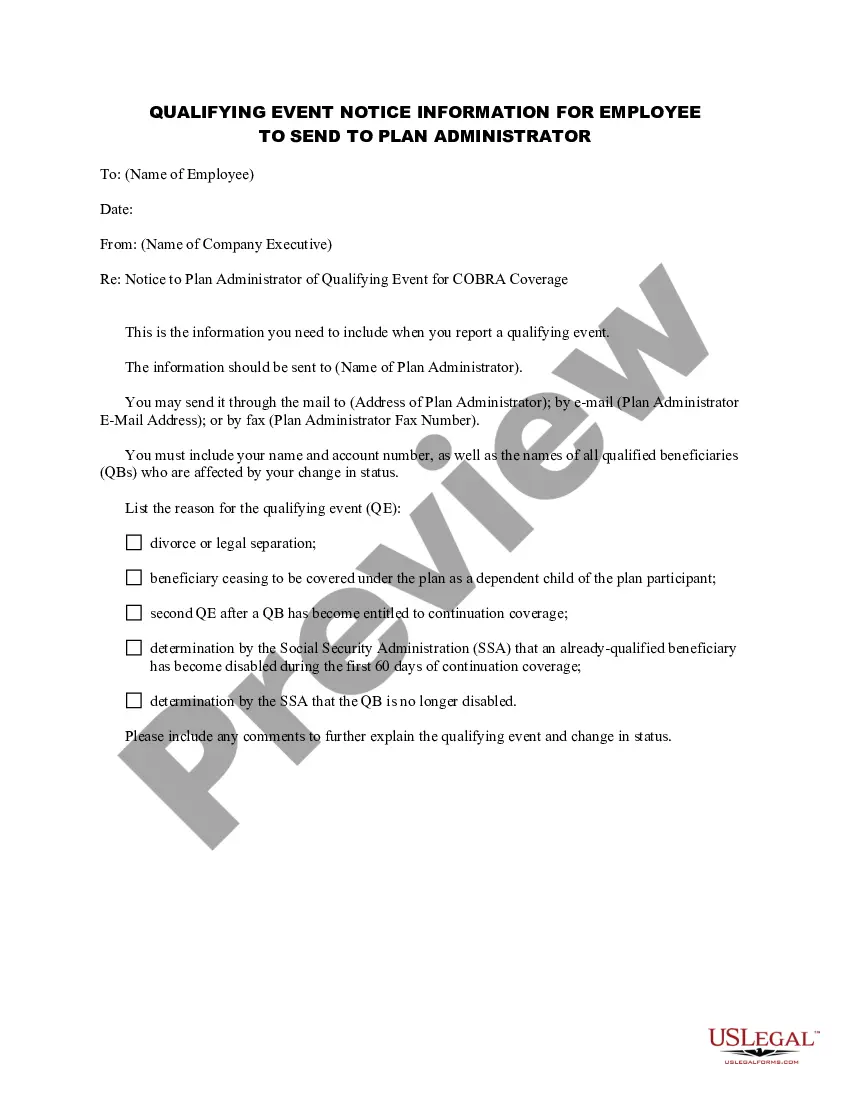
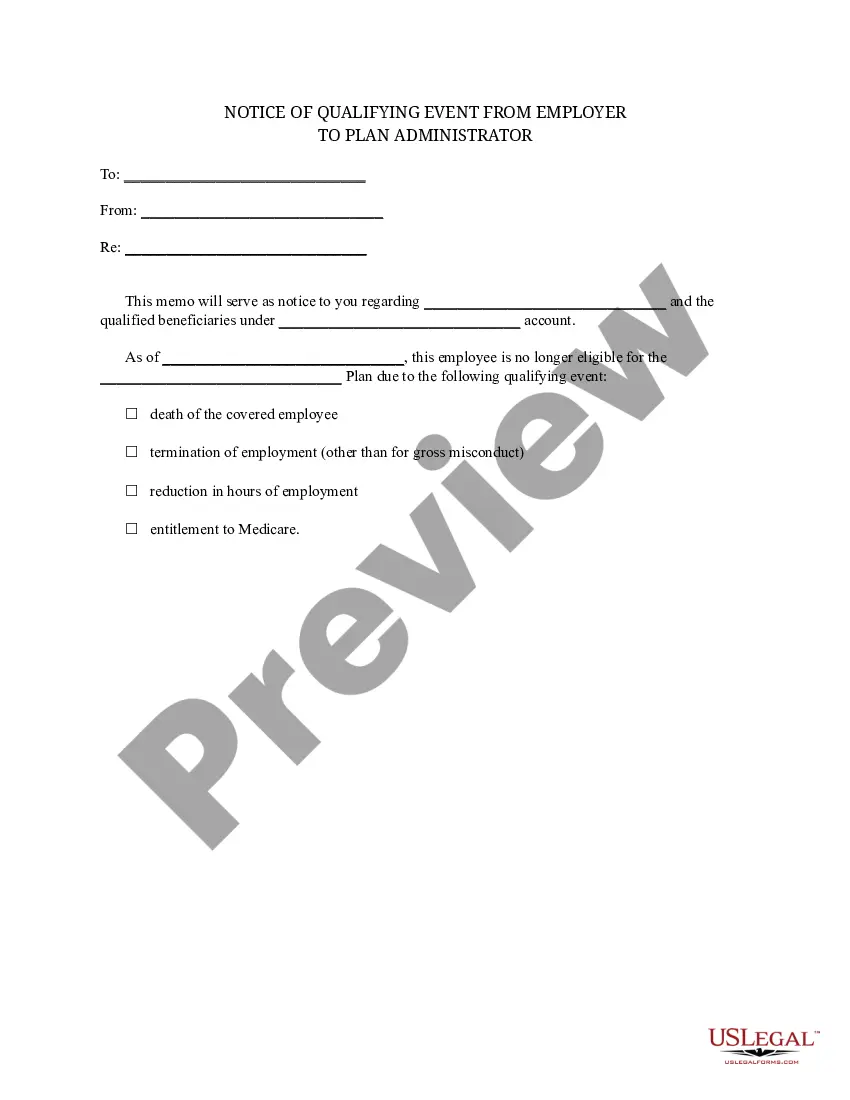
Wyoming Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
If you need to gather, obtain, or print authorized document templates, use US Legal Forms, the largest selection of legal forms available online.
Utilize the site’s simple and user-friendly search to find the documents you need.
Various templates for business and personal purposes are organized by categories and states or keywords.
Step 4. Once you have found the form you need, click the Buy now button. Choose your preferred payment plan and enter your information to register for an account.
Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the purchase.
- Use US Legal Forms to find the Wyoming Notice of Qualifying Event from Employer to Plan Administrator in just a few clicks.
- If you are already a US Legal Forms user, Log In to your account and click the Download button to obtain the Wyoming Notice of Qualifying Event from Employer to Plan Administrator.
- You can also access forms you have previously downloaded in the My documents tab of your account.
- If you are using US Legal Forms for the first time, follow these steps.
- Step 1. Ensure you have selected the form for your specific city/state.
- Step 2. Use the Preview option to review the form’s contents. Don’t forget to check the description.
- Step 3. If you are not satisfied with the document, use the Search area at the top of the screen to find other versions of the legal form template.
Form popularity
FAQ
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The qualifying event for COBRA purposes is the employee's loss of employment date. However, the election period does not end until 60 days from the sent date of the election form to the employee or until 60 days after the loss of coverage, whichever is later.
Losing your health care coverage because you lost or quit your job counts as a qualifying life event, says Scott Eckley, president of Apollo Insurance Group.
A plan, however, may provide longer periods of coverage beyond the maximum period required by law. When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
A change in your situation like getting married, having a baby, or losing health coverage that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Most employees lose their employer-sponsored health coverage either on their last day of work or at the end of the month during which they stop working. After leaving a job, you will likely have access to COBRAtemporary coverage lets you continue your health plan, although you'll pay the full cost of premiums.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
You'll have 60 days to enroll in COBRA or another health plan once your benefits end. But keep in mind that delaying enrollment won't save you money. COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.