Wyoming Qualifying Event Notice Information for Employer to Plan Administrator
Description
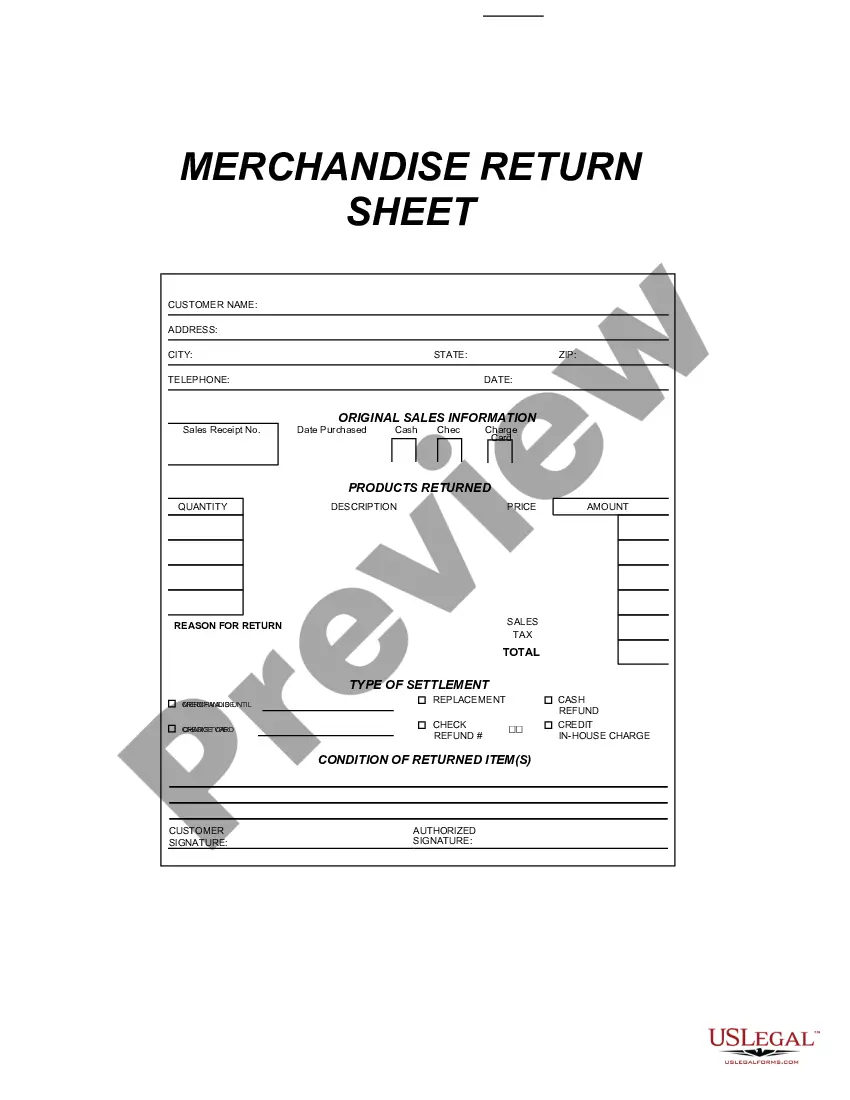
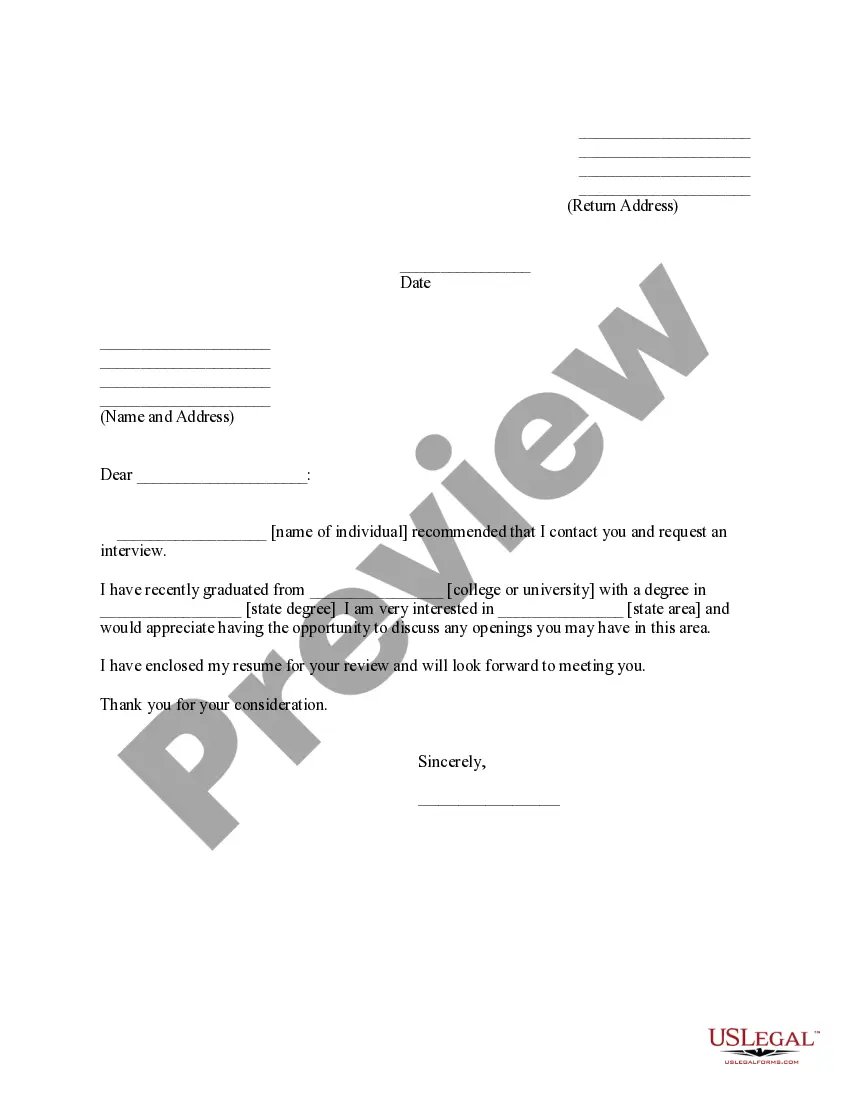
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
Are you in a situation where you must have documentation for potential professional or personal purposes nearly every time.
There is a multitude of legal document templates accessible online, yet finding reliable ones can be challenging.
US Legal Forms provides thousands of form templates, such as the Wyoming Qualifying Event Notice Information for Employer to Plan Administrator, which are designed to comply with federal and state requirements.
Once you find the correct form, click Get now.
Choose the pricing plan you desire, fill in the required information to create your account, and pay for your order using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Then, you can download the Wyoming Qualifying Event Notice Information for Employer to Plan Administrator template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Obtain the form you need and ensure it is for the correct city/region.
- Utilize the Review option to examine the document.
- Check the description to confirm that you have selected the accurate form.
- If the form is not what you're searching for, use the Research field to find the form that suits your requirements.
Form popularity
FAQ
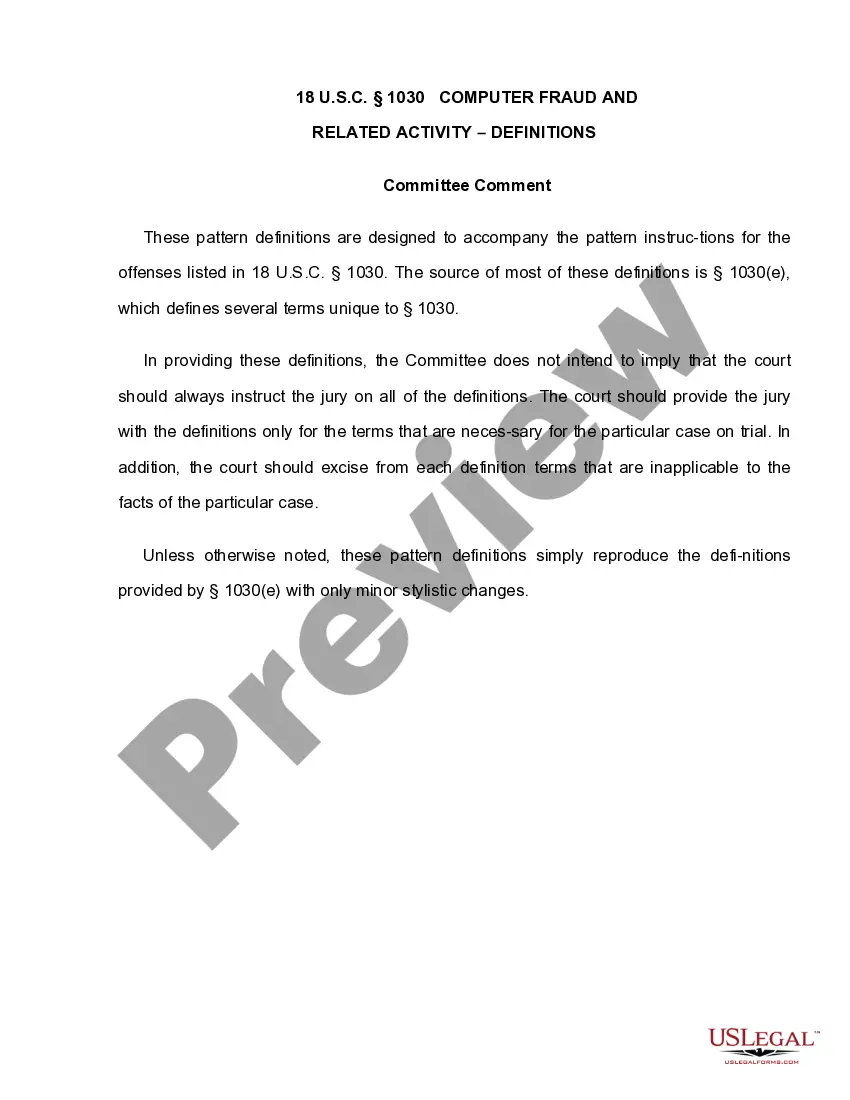
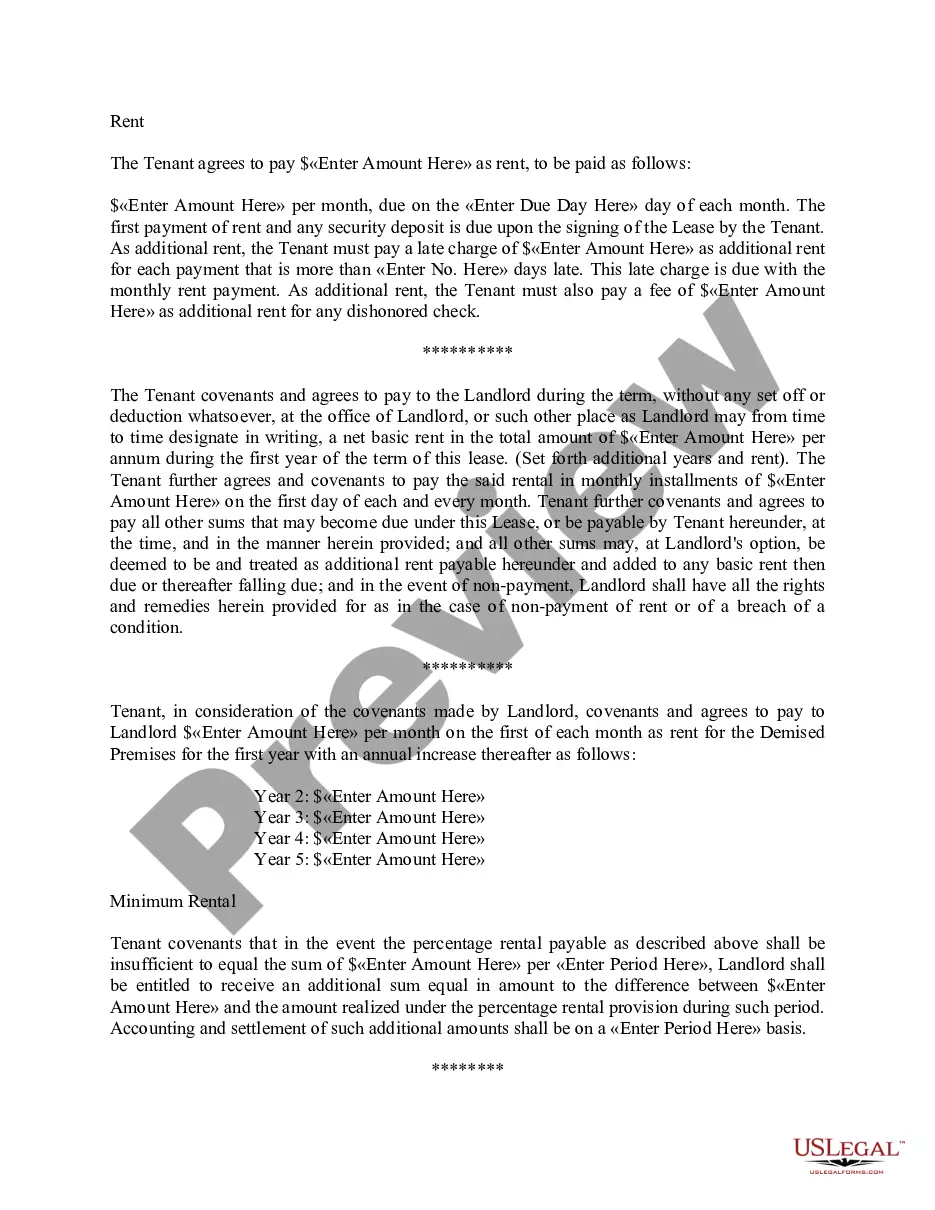
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Cobra is a discontinued general-purpose, object-oriented programming language. Cobra is designed by Charles Esterbrook, and runs on the Microsoft . NET and Mono platforms. It is strongly influenced by Python, C#, Eiffel, Objective-C, and other programming languages. It supports both static and dynamic typing.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.