Model COBRA Continuation Coverage Election Notice
What is this form?
The Model COBRA Continuation Coverage Election Notice is a legal document that provides essential information regarding an individual's right to continue their health care coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA). This form is specifically designed for use by single-employer group health plans, allowing qualified beneficiaries to elect continuation coverage after a qualifying event, such as job loss or a reduction in hours. It serves a critical purpose in ensuring that individuals maintain access to health care despite changes in their employment status.
Key parts of this document
- Date of the notice.
- Identification of qualified beneficiaries by name or status.
- Details on the health care plan, including coverage options and costs.
- Instructions for completing the Election Form and submission details.
- Explanation of rights under COBRA, including how long the coverage will last.
- Reasons for termination of coverage and procedures for notifying about changes.
Common use cases
This form should be used when a qualified beneficiary has experienced a qualifying event such as termination of employment, a reduction in hours, divorce, legal separation, or death of the covered employee. It is essential for notifying the individual of their right to elect COBRA continuation coverage, which is crucial to safeguard their access to health care benefits during times of change.
Who should use this form
- Employees or former employees who have experienced a qualifying event.
- Spouses or former spouses of employees affected by a qualifying event.
- Dependent children covered under the health plan who may lose coverage.
Instructions for completing this form
- Enter the date of the notice at the top of the form.
- Identify each qualified beneficiary by name or status.
- Specify the date when COBRA coverage will begin and the duration of coverage.
- Select the relevant reasons for the qualifying event from the provided options.
- Complete the Election Form and submit it by the specified due date, ensuring proper contact information is included.
Does this form need to be notarized?
This form usually doesn’t need to be notarized. However, local laws or specific transactions may require it. Our online notarization service, powered by Notarize, lets you complete it remotely through a secure video session, available 24/7.
Get your form ready online
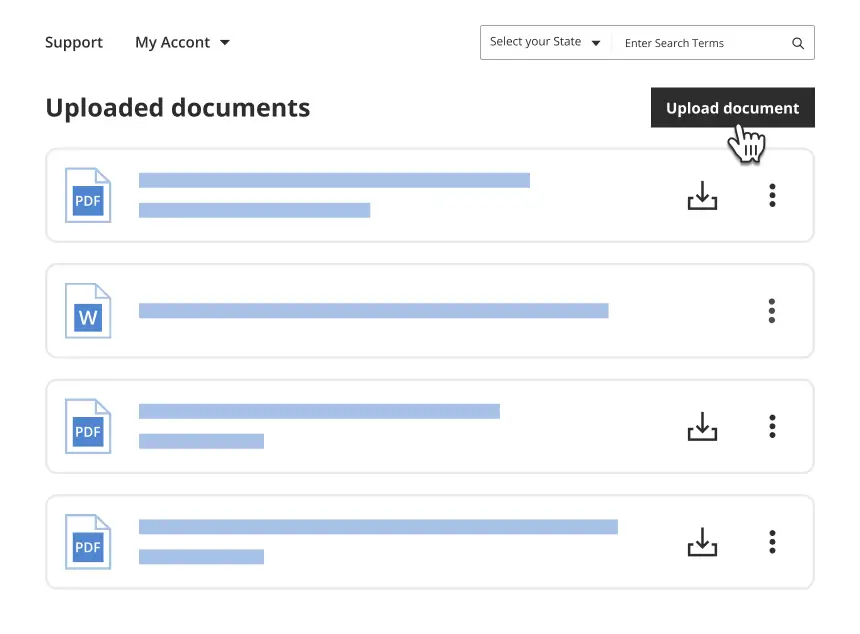
Our built-in tools help you complete, sign, share, and store your documents in one place.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Common mistakes to avoid
- Failing to submit the Election Form by the due date.
- Leaving out essential information such as names or dates.
- Not including the correct payment amount for COBRA coverage.
- Overlooking the requirement to notify the plan of any changes in status or dependent eligibility.
Advantages of online completion
- Convenience of downloading and completing the form at your own pace.
- Easy access to legal updates and applicable requirements.
- Ability to save time with an efficient, user-friendly format.
- Reliability of forms drafted by licensed attorneys to ensure compliance with legal standards.
Looking for another form?
Form popularity
FAQ
You may be eligible to apply for individual coverage through Covered California, the State's Health Benefit Exchange. You can reach Covered California at (800) 300-1506 or online at www.coveredca.com. You can apply for individual coverage directly through some health plans off the exchange.
Leave a company with 20 or more employees, or have your hours reduced. Private sector and state or local government employers with 20 or more employees offer COBRA continuation coverage. Wait for a letter in the mail. Elect health coverage within 60 days. Make a payment within 45 days.
If you enroll in COBRA before the 60 days are up, your coverage is then retroactive, as long as you pay the retroactive premiums. This means that if you incur medical bills during your "election period," you can retroactively and legally elect COBRA and have those bills covered.
You must meet three basic requirements to be entitled to elect COBRA continuation coverage: Your group health plan must be covered by COBRA; 2022 A qualifying event must occur; and 2022 You must be a qualified beneficiary for that event.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Q8: How long do I have to elect COBRA coverage? If you are entitled to elect COBRA coverage, you must be given an election period of at least 60 days (starting on the later of the date you are furnished the election notice or the date you would lose coverage) to choose whether or not to elect continuation coverage.
Assuming one pays all required premiums, COBRA coverage starts on the date of the qualifying event, and the length of the period of COBRA coverage will depend on the type of qualifying event which caused the qualified beneficiary to lose group health plan coverage.
The insurance company. COBRA Election Notice. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. The election notice describes their rights to continuation coverage and how to make an election.