COBRA Continuation Coverage Election Notice
Description
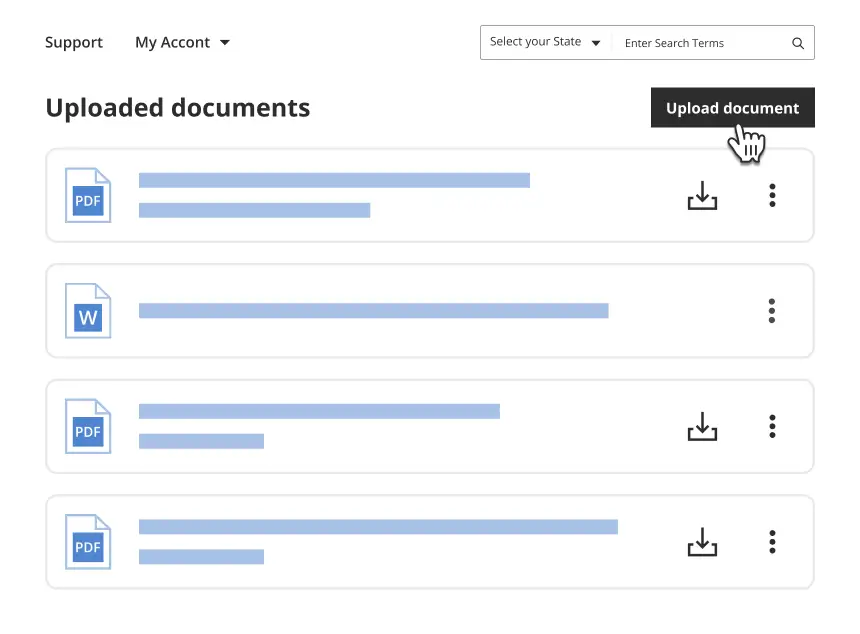
Get your form ready online
Our built-in tools help you complete, sign, share, and store your documents in one place.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
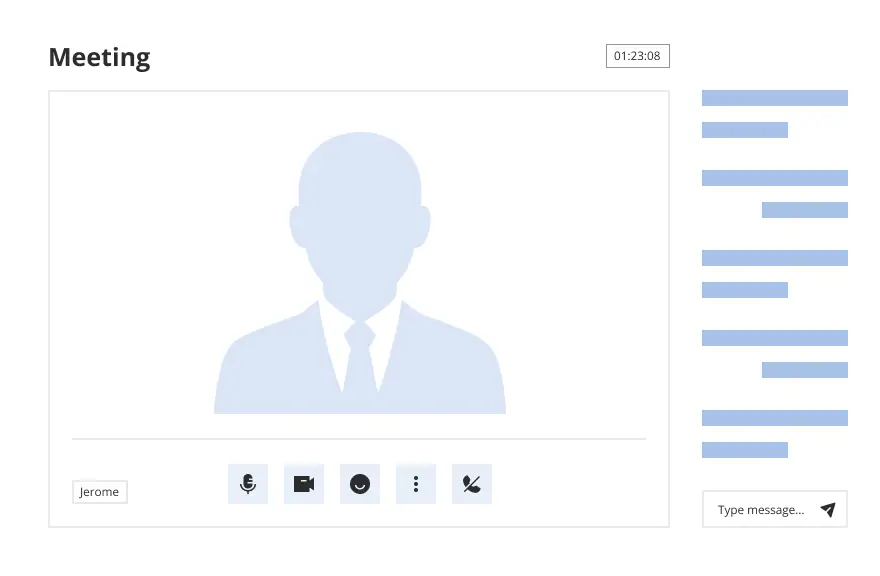
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Looking for another form?
- COBRA Continuation Coverage: A federal provision allowing for the temporary extension of group health coverage that would otherwise be terminated.
- Election Notice: A document that must be sent to a qualified beneficiary explaining their rights to elect COBRA continuation coverage within 60 days following a qualifying event.
- Qualified Beneficiary: An individual covered under a group health plan on the day before a qualifying event who is an employee, the employee's spouse, or the employee's dependent child.
- Qualifying Event: An event that causes a covered employee, or a qualified beneficiary, to lose their health insurance coverage, including job loss, reduction in hours, or other life events such as divorce or death.
- Group Health Plan: A health plan offered by an employer or employee organization that provides health care to employees and their families.
- Understand Your Notification: Ensure you receive the election notice post a qualifying event and read it thoroughly.
- Evaluate Continuation Coverage: Consider your health insurance needs and how the continuation of your group health plan could benefit you.
- Decide to Elect COBRA Coverage: Choose whether to continue with the COBRA coverage. Remember, the election period typically lasts for 60 days from the date of the qualifying event or the date the notice is provided.
- Complete Necessary Forms: Fill out and return the election form to the plan administrator by the deadline stated in the notice.
- Make Payment: Be aware of the initial premium payment deadline to prevent loss of coverage.
- Lack of Coverage: Failing to elect COBRA coverage could leave you without health insurance, potentially leading to high medical costs due to unexpected illness or accidents.
- Condition Exclusions: Delay in obtaining alternative coverage may result in pre-existing condition exclusions.
- Financial Implications: Absence of health plan could mean significant personal financial liability in the face of health issues.
- What is the cost of COBRA continuation coverage? COBRA coverage typically costs 102% of the plan cost, which includes an administration fee. Generally, it is more expensive than coverage for active employees.
- Can I switch to another health plan under COBRA? No, when electing COBRA, you must continue with the same level of health benefits that were available before the qualifying event.
- How long can I maintain COBRA continuation coverage? COBRA continuation coverage can last up to 18 months after the qualifying event, which can be extended to 36 months under certain circumstances.
How to fill out COBRA Continuation Coverage Election Notice?
Among lots of free and paid samples that you’re able to get online, you can't be certain about their accuracy. For example, who created them or if they are qualified enough to take care of the thing you need them to. Always keep calm and utilize US Legal Forms! Discover COBRA Continuation Coverage Election Notice samples created by skilled legal representatives and get away from the expensive and time-consuming procedure of looking for an lawyer or attorney and then having to pay them to draft a papers for you that you can easily find yourself.
If you have a subscription, log in to your account and find the Download button next to the form you’re trying to find. You'll also be able to access all your earlier saved files in the My Forms menu.
If you’re making use of our platform the very first time, follow the instructions below to get your COBRA Continuation Coverage Election Notice fast:
- Make certain that the document you find is valid where you live.
- Review the file by reading the description for using the Preview function.
- Click Buy Now to start the ordering process or find another example using the Search field in the header.
- Choose a pricing plan and create an account.
- Pay for the subscription using your credit/debit/debit/credit card or Paypal.
- Download the form in the needed file format.
Once you have signed up and purchased your subscription, you can use your COBRA Continuation Coverage Election Notice as many times as you need or for as long as it remains valid where you live. Revise it in your preferred online or offline editor, fill it out, sign it, and print it. Do much more for less with US Legal Forms!
Form popularity
FAQ
The insurance company. COBRA Election Notice. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. The election notice describes their rights to continuation coverage and how to make an election.
Notices properly mailed are generally considered provided on the date sent, regardless of whether they're actually received. 1. COBRA Initial Notice must be provided. Within 30 days after the employee first becomes enrolled in the group health plan.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
1. You never received your COBRA enrollment packet. Contact your former employer or your health plan administrator.Your former employer must notify your health plan administrator within 30 days after your "qualifying event" death, job termination, reduced hours of employment or eligibility for Medicare.
An employer that is subject to COBRA requirements is required to notify its group health plan administrator within 30 days after an employee's employment is terminated, or employment hours are reduced.
Plan Administrator has 14 days to provide a COBRA election notice to the former employee/qualified beneficiary. Qualified beneficiary has 60 days from the date of the notification to make an election to continue enrollment in the plan(s). Qualified beneficiary has 45 days to pay the first premium.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The employer must notify the plan within 30 days of the event. You (the covered employee or one of the qualified beneficiaries) must notify the plan if the qualifying event is divorce, legal separation, or a child's loss of dependent status under the plan.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.