Election Form for Continuation of Benefits - COBRA
Description
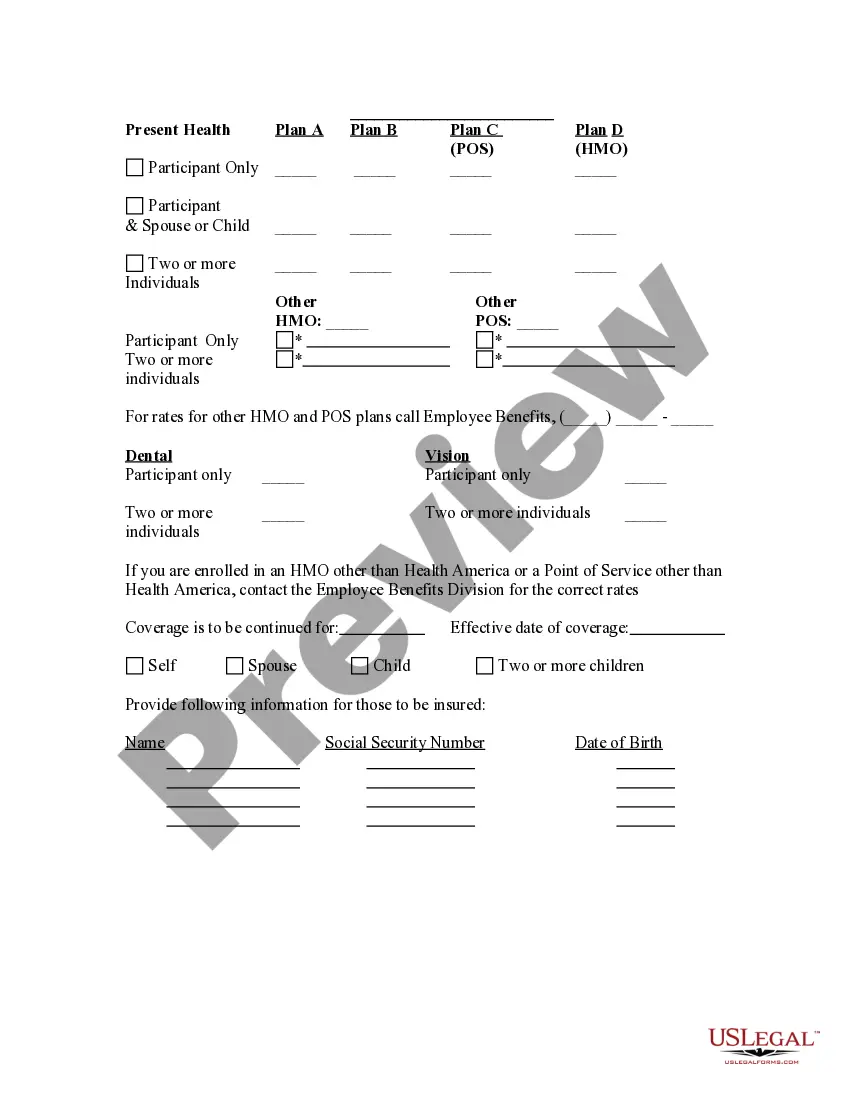
How to fill out Election Form For Continuation Of Benefits - COBRA?
Among numerous paid and free examples that you’re able to get on the net, you can't be certain about their accuracy and reliability. For example, who made them or if they are skilled enough to deal with what you require these people to. Always keep relaxed and utilize US Legal Forms! Discover Election Form for Continuation of Benefits - COBRA samples developed by skilled legal representatives and get away from the expensive and time-consuming process of looking for an attorney and then paying them to draft a document for you that you can find on your own.
If you already have a subscription, log in to your account and find the Download button near the file you’re looking for. You'll also be able to access all your earlier saved samples in the My Forms menu.
If you’re making use of our platform the first time, follow the tips listed below to get your Election Form for Continuation of Benefits - COBRA easily:
- Make certain that the file you see applies in the state where you live.
- Look at the template by reading the information for using the Preview function.
- Click Buy Now to begin the purchasing procedure or look for another example using the Search field in the header.
- Select a pricing plan sign up for an account.
- Pay for the subscription with your credit/debit/debit/credit card or Paypal.
- Download the form in the required format.
As soon as you’ve signed up and paid for your subscription, you can utilize your Election Form for Continuation of Benefits - COBRA as often as you need or for as long as it continues to be active in your state. Revise it in your favorite online or offline editor, fill it out, sign it, and create a hard copy of it. Do more for less with US Legal Forms!
Form popularity
FAQ
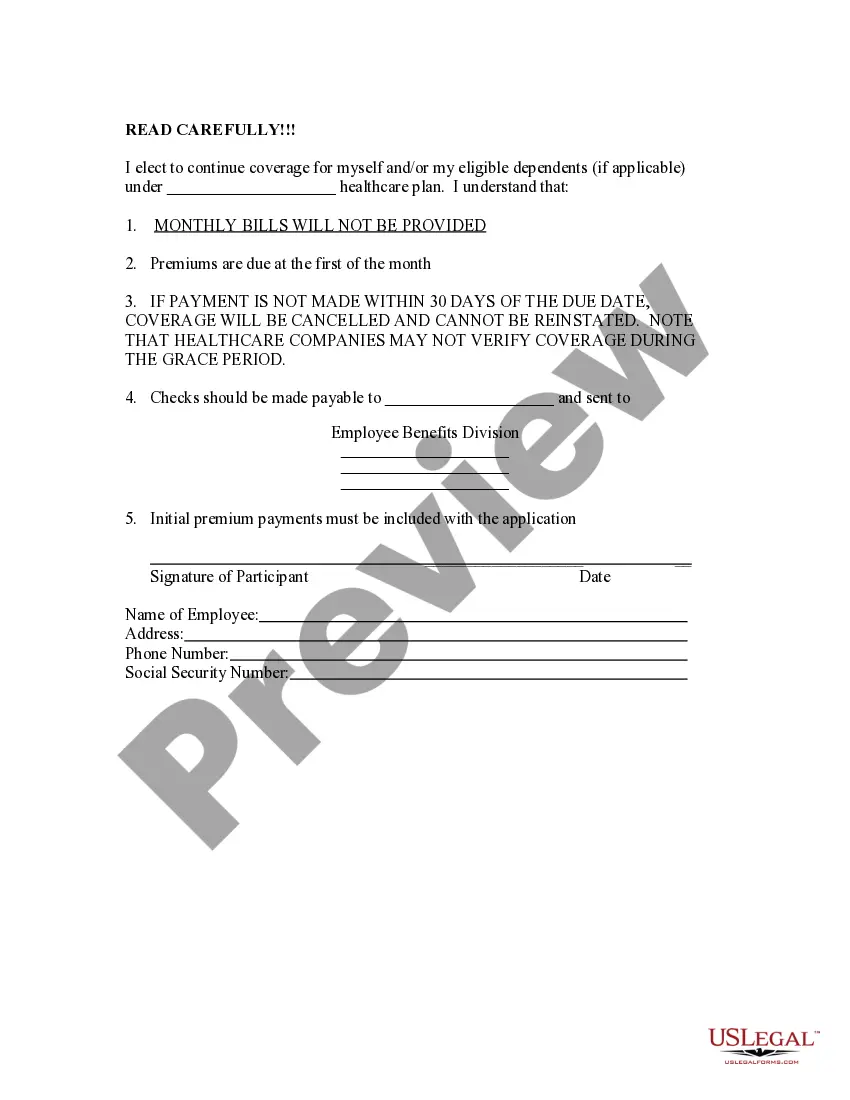
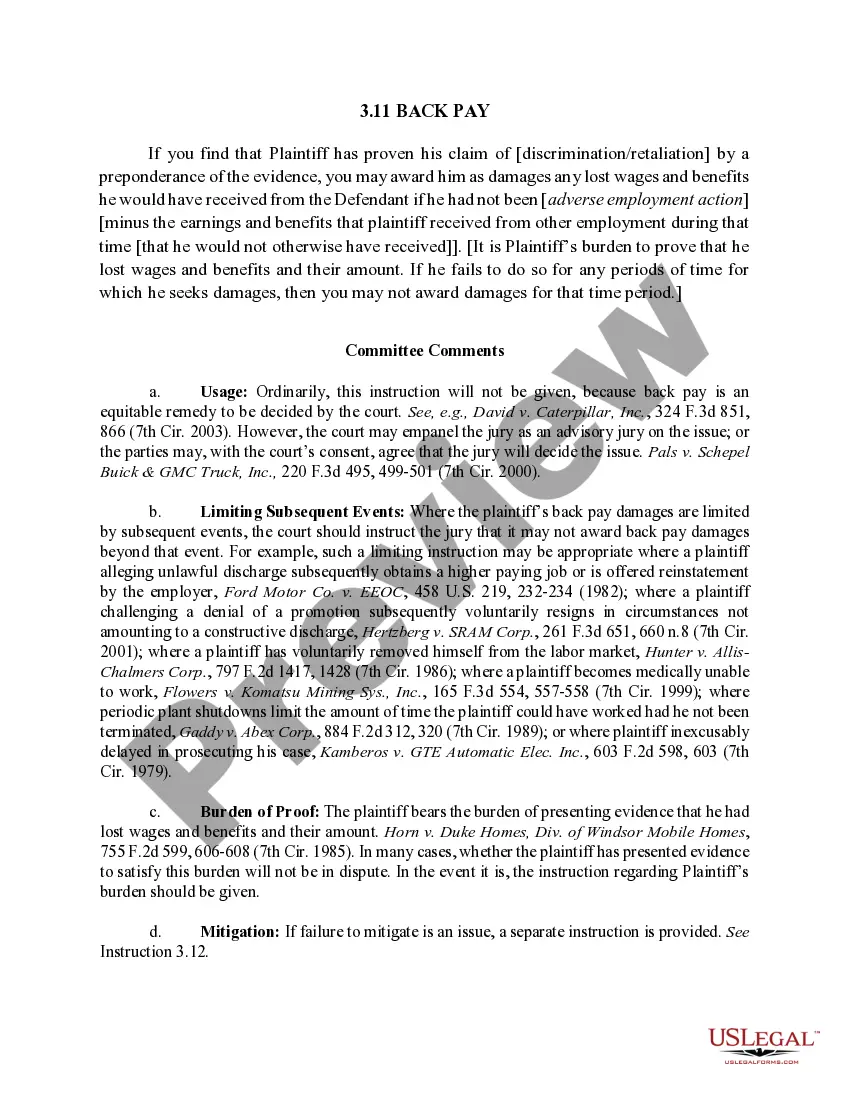
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Leave a company with 20 or more employees, or have your hours reduced. Private sector and state or local government employers with 20 or more employees offer COBRA continuation coverage. Wait for a letter in the mail. Elect health coverage within 60 days. Make a payment within 45 days.
The insurance company. COBRA Election Notice. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. The election notice describes their rights to continuation coverage and how to make an election.
You may be eligible to apply for individual coverage through Covered California, the State's Health Benefit Exchange. You can reach Covered California at (800) 300-1506 or online at www.coveredca.com. You can apply for individual coverage directly through some health plans off the exchange.
You may be eligible to apply for individual coverage through Covered California, the State's Health Benefit Exchange. You can reach Covered California at (800) 300-1506 or online at www.coveredca.com. You can apply for individual coverage directly through some health plans off the exchange.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
With COBRA insurance, you're on the hook for the whole thing. That means you could be paying average monthly premiums of $569 to continue your individual coverage or $1,595 for family coveragemaybe more!
Assuming one pays all required premiums, COBRA coverage starts on the date of the qualifying event, and the length of the period of COBRA coverage will depend on the type of qualifying event which caused the qualified beneficiary to lose group health plan coverage.