Tennessee COBRA Continuation Coverage Election Notice
Description
How to fill out COBRA Continuation Coverage Election Notice?
Selecting the appropriate legal document template can be quite a challenge.
Certainly, there is an abundance of templates accessible online, but how do you find the legal form you seek.
Utilize the US Legal Forms website. This service offers numerous templates, including the Tennessee COBRA Continuation Coverage Election Notice, suitable for both business and personal uses.
If the form does not meet your needs, use the Search feature to find the appropriate document. Once you are certain that the form works, click the Get now button to obtain it. Choose the pricing plan you want and enter the required information. Create your account and pay for the order using your PayPal account or credit card. Select the file format and download the legal document template to your device. Complete, modify, print, and sign the obtained Tennessee COBRA Continuation Coverage Election Notice. US Legal Forms is the largest collection of legal documents where you can find a variety of document templates. Utilize the service to download properly crafted documents that meet state requirements.
- All forms are reviewed by professionals and comply with federal and state regulations.
- If you are already registered, Log In to your account and click the Acquire button to locate the Tennessee COBRA Continuation Coverage Election Notice.
- Use your account to search through the legal documents you have previously purchased.
- Go to the My documents tab in your account and get another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple steps for you to follow.
- First, ensure you have selected the correct document for your city/state. You can review the form using the Preview button and read the form description to confirm it is indeed the right one for you.
Form popularity
FAQ
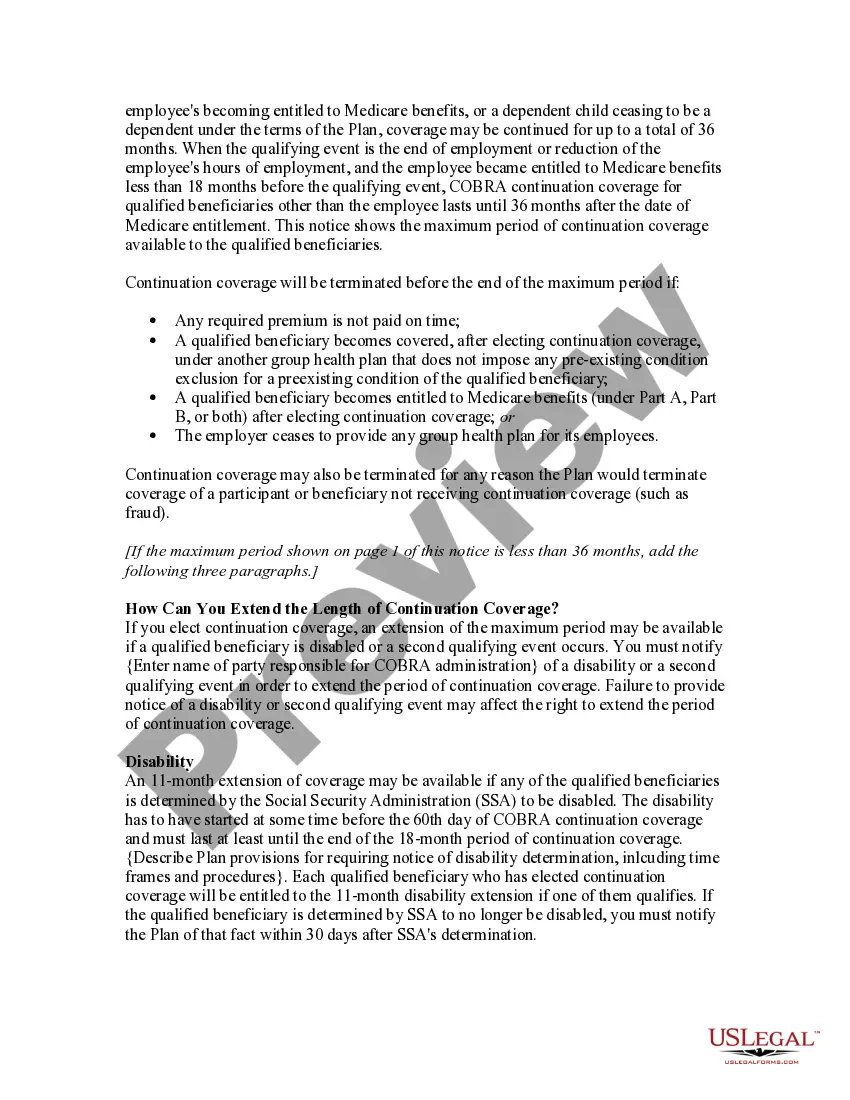
Tennessee - Coverage can be extended for the remainder of the month in which it would have terminated, plus up to three additional months. An individual who loses access to group coverage during pregnancy can continue their coverage for at least the duration of the pregnancy plus six months.
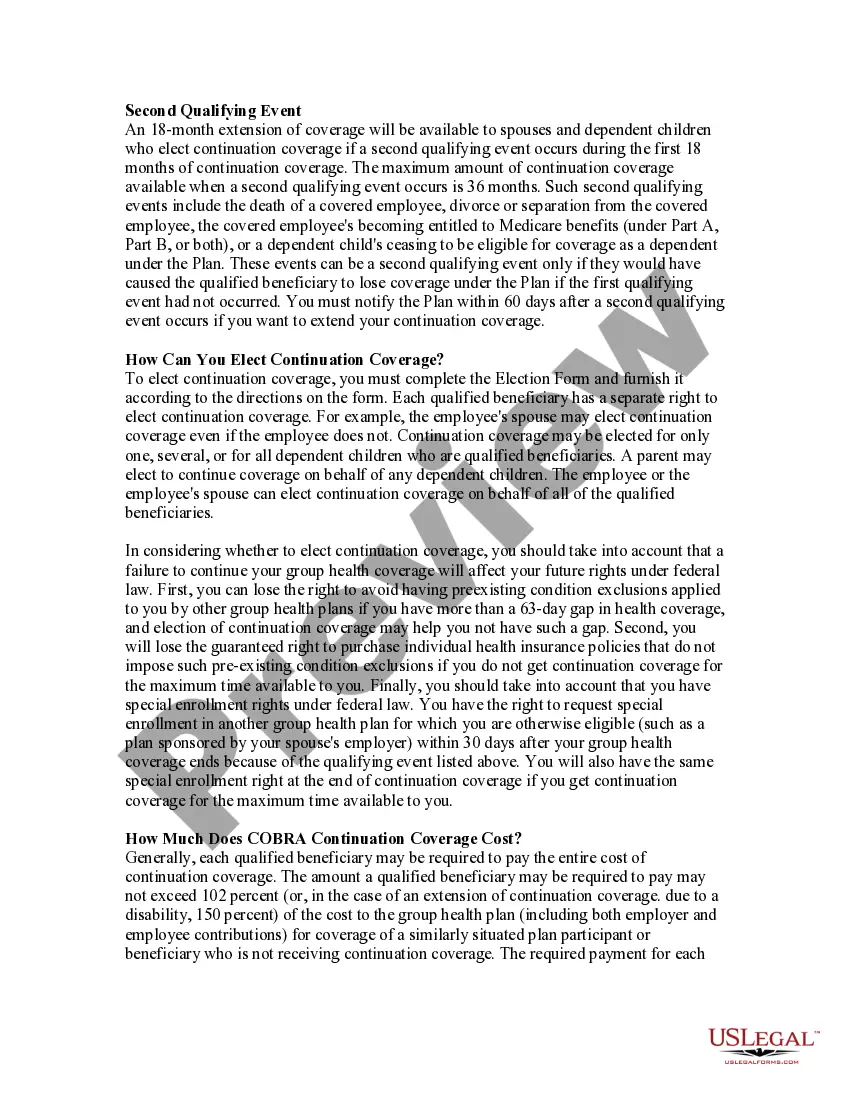
State continuation coverage refers to state laws that enable employees to extend their employer-sponsored group health insurance even if they are not eligible for an extension through COBRA. While COBRA law applies throughout the U.S., it is only applicable to employers with 20 or more employees.
The term continuation coverage refers to the extended coverage provided under the group benefit plan in which an eligible employee or eligible dependent is currently enrolled.
Through COBRA, individuals pay the entire monthly premium plus a two percent administrative fee, and may be able to remain insured with their health plan for up to 18, 29, or 36 months.
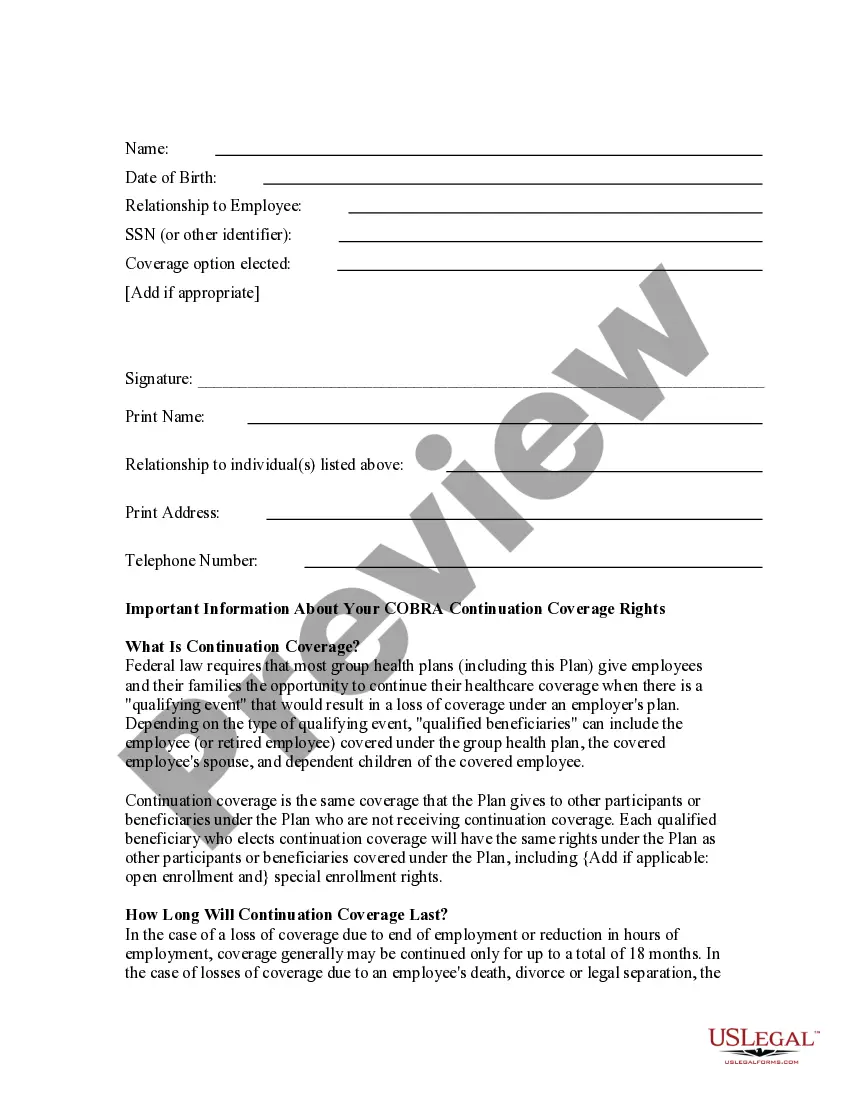
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
What is state continuation? State law allows employees of smaller employers (fewer than 20 employees) to keep the same group health insurance coverage for up to nine months after loss of a job or loss of coverage because of a reduction in work hours. This is called state continuation.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
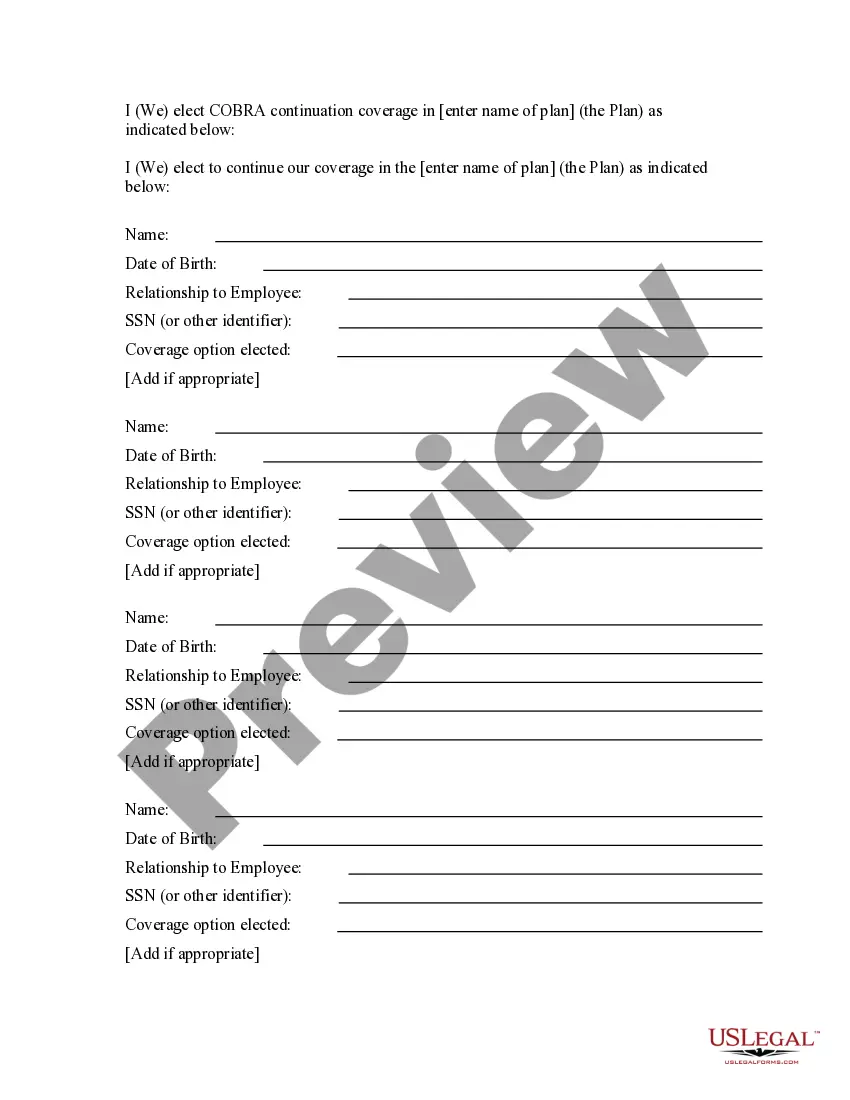
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.