Tennessee Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
If you need to access, download, or print sanctioned document templates, utilize US Legal Forms, the most extensive collection of legal forms available online.
Employ the site’s straightforward and user-friendly search feature to find the documents you require.
Numerous templates for business and personal purposes are organized by categories and states or keywords.
Every legal document template you purchase is yours forever. You will have access to every form you acquired with your account.
Click the My documents section to select a form to print or download again. Get, download, and print the Tennessee Introductory COBRA Letter with US Legal Forms. There are thousands of professional and state-specific forms available for your business or personal needs.
- Use US Legal Forms to obtain the Tennessee Introductory COBRA Letter with just a few clicks.
- If you are already a US Legal Forms user, Log In to your account and click the Obtain button to get the Tennessee Introductory COBRA Letter.
- You can also access forms you previously acquired in the My documents tab of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1: Ensure you have selected the form for the correct city/region.
- Step 2: Use the Preview option to review the form’s content. Be sure to read the description.
- Step 3: If you are not satisfied with the form, use the Search field at the top of the screen to find other variations of legal form designs.
- Step 4: After locating the form you need, click the Purchase now button. Choose the pricing plan you prefer and provide your details to create an account.
- Step 5: Process the payment. You can use your Visa, Mastercard, or PayPal account to complete the transaction.
- Step 6: Choose the format of the legal form and download it to your device.
- Step 7: Complete, modify, and print or sign the Tennessee Introductory COBRA Letter.
Form popularity
FAQ
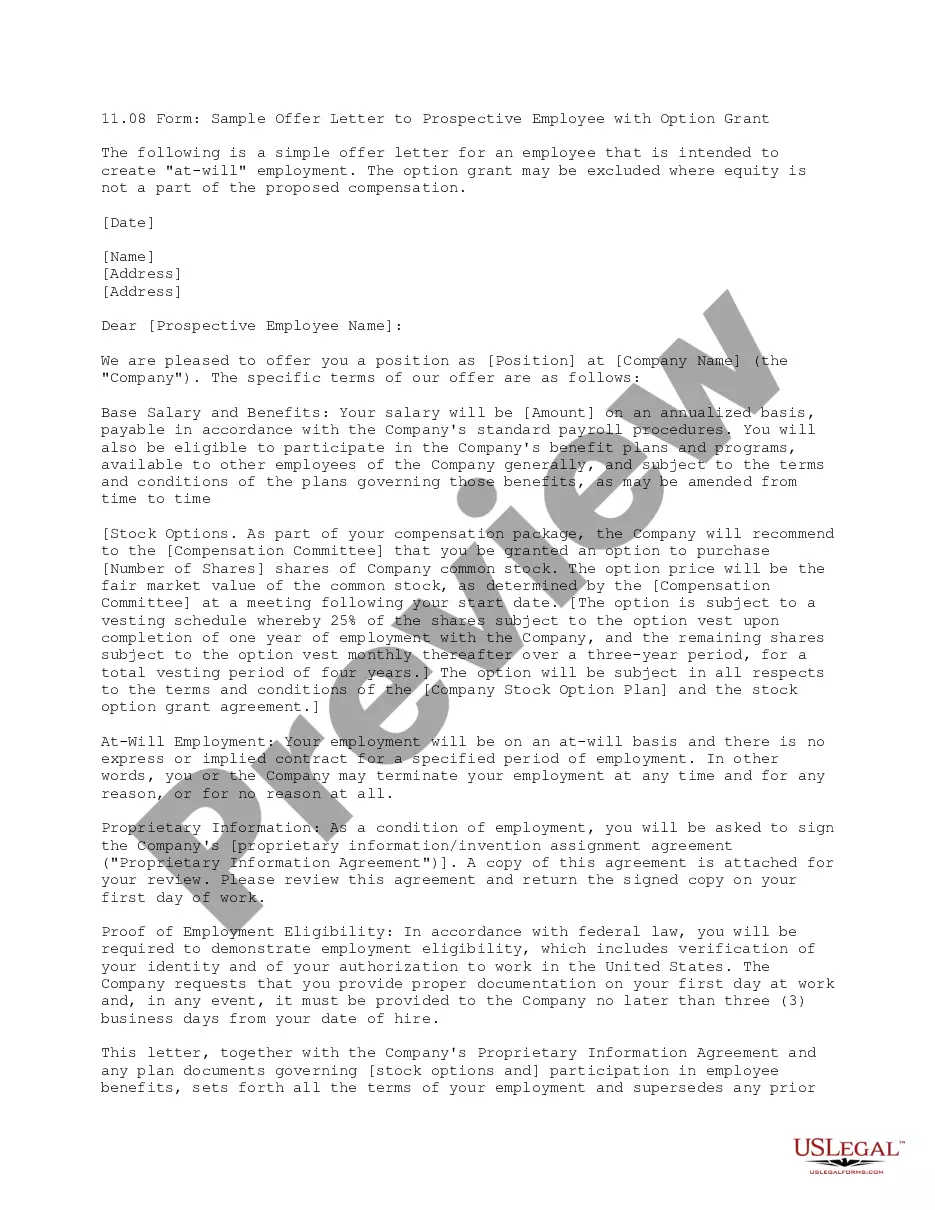
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Draft a letter stating facts why the COBRA benefits must be reinstated. The letter must provide your full legal name, address, Social Security number and COBRA policy number. The letter should be in proper business format and is best if free from all spelling and grammatical errors.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Once COBRA coverage is canceled, there is no option for reinstatement. Note that waiting until the end of the grace period to make payment may not allow enough time within the grace period to reconcile payment if your check is lost in the mail or is rejected by your bank.
If you feel the non-commencement or termination of your benefits under the Federal COBRA regulations was in error, you have the right to file an appeal by writing a letter which explains why you believe the coverage should be reinstated.
A COBRA letter is drafted by the plan administrator with a copy mailed to each qualified beneficiary before the coverage is terminated. The COBRA termination letter format must include the reason why the coverageis being terminated, the rights of the beneficiaries, and the specific date the coverage will end.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.