Cobra Coverage Complete With Contacts
Description
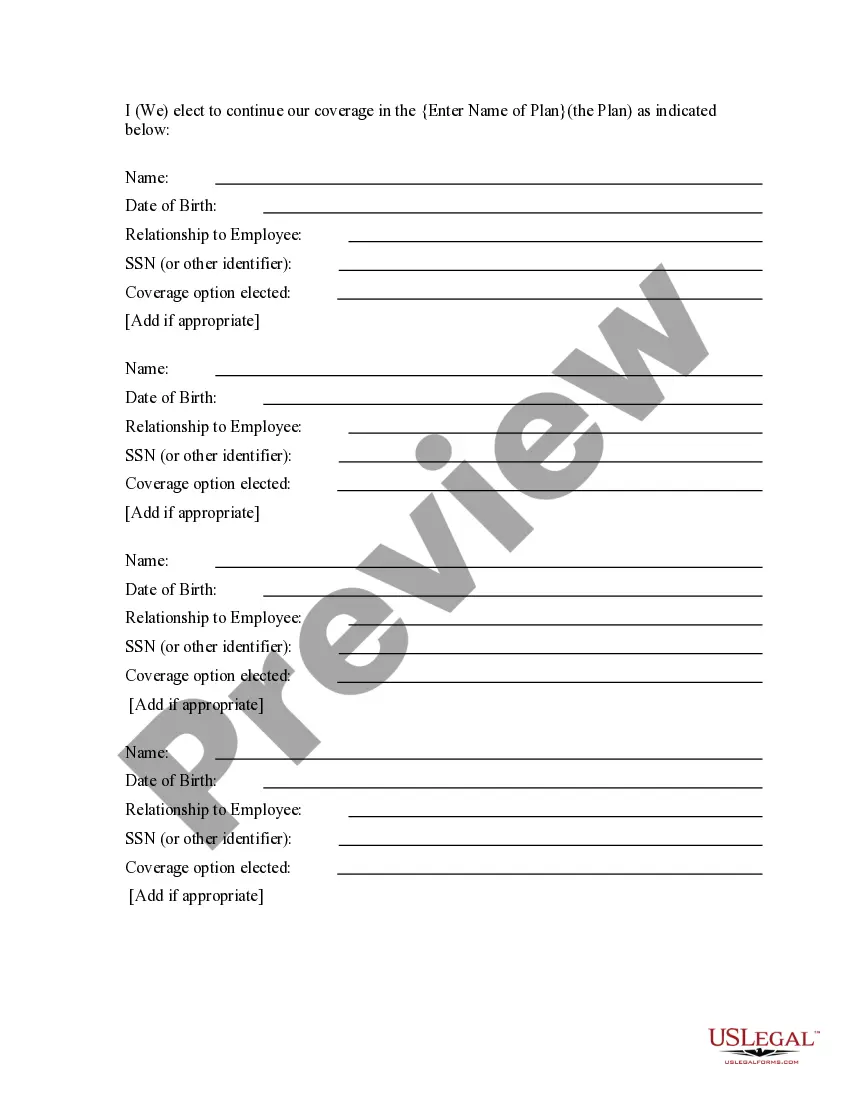
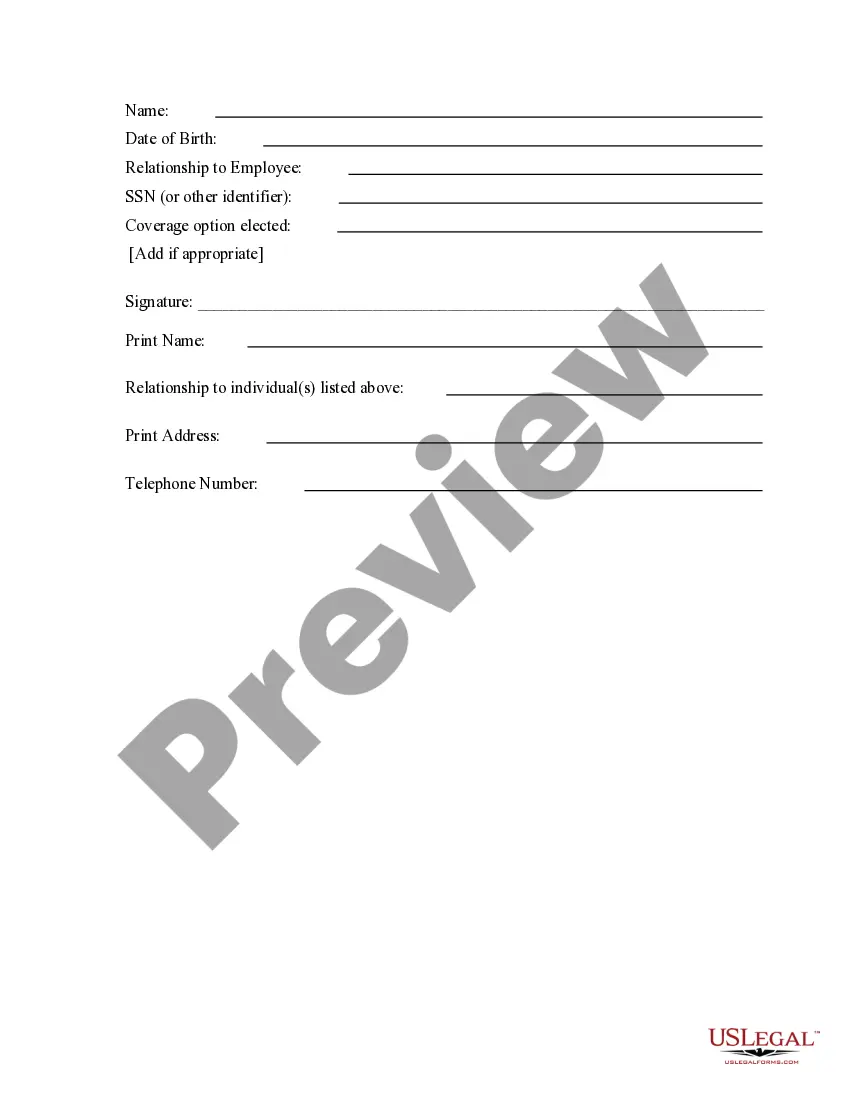
How to fill out COBRA Continuation Coverage Election Form?
It’s well-known that you cannot transform into a legal specialist instantly, nor can you quickly learn to effectively draft Cobra Coverage Complete With Contacts without a specialized education.
Assembling legal documents is a lengthy undertaking that necessitates specific training and expertise. Therefore, why not allow the professionals to handle the creation of the Cobra Coverage Complete With Contacts.
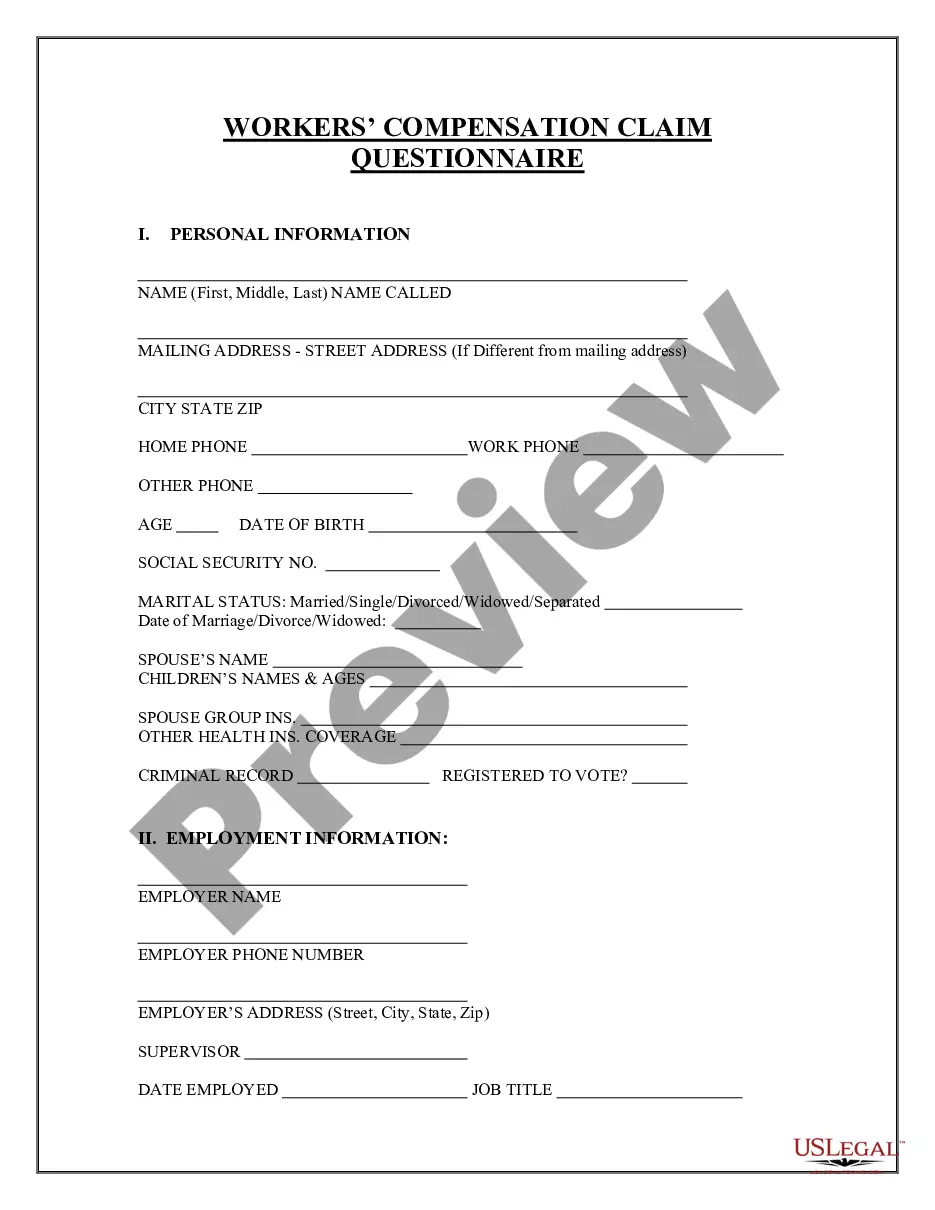
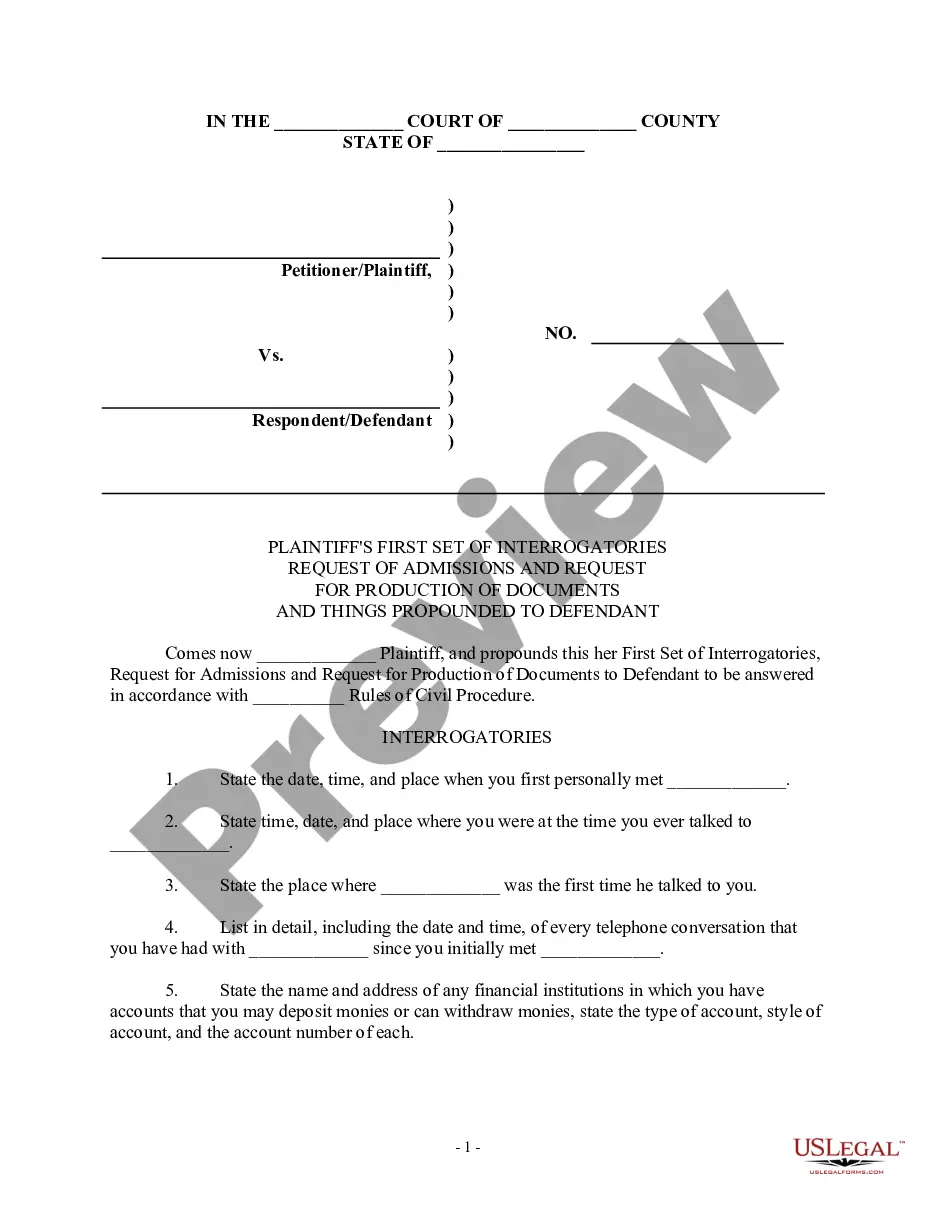
With US Legal Forms, one of the most extensive legal document repositories, you can access anything from court forms to templates for internal corporate communications.
You can revisit your forms from the My documents tab at any time. If you’re a returning customer, you can simply Log In, and locate and download the template from the same tab.
Regardless of the purpose of your forms—whether they are financial, legal, or personal—our platform has you covered. Give US Legal Forms a try today!
- Find the document you require using the search bar located at the top of the page.
- Preview it (if this feature is available) and review the accompanying description to determine if Cobra Coverage Complete With Contacts meets your needs.
- Initiate your search again if you need any other form.
- Create a free account and select a subscription option to purchase the form.
- Click Buy now. Once the payment is processed, you can obtain the Cobra Coverage Complete With Contacts, complete it, print it, and send or mail it to the specified individuals or organizations.
Form popularity
FAQ
With COBRA, you can use your health insurance plan like you did when employed. However, you'll pay all the costs without help from your former employer. You can keep COBRA for at least 18 months. Sometimes, you can have a COBRA plan for up to 36 months, depending on the qualifying event.
Applying for COBRA begins with the employer who provided the health plan to notify you of your right to continuation. The employer has 30 days to notify the group health plan of the qualifying event. After that, the employer has 14 days to notify you of your COBRA right to keep your work health insurance.
COBRA is Retroactive. When you receive your COBRA letter, you have 60 days to submit the paperwork with your insurance company. However, no matter when you submit the paperwork during this time, you are covered retroactively from day 1. The catch: you will also be responsible for all premiums from day 1.
When Federal COBRA ends, eligible employees can buy 18 months additional health coverage under Cal-COBRA. All qualified beneficiaries are generally eligible for continuation coverage for 36 months after the date the qualified beneficiary's benefits would otherwise have terminated.
In that case, COBRA lasts for eighteen months. If the qualifying event is the death of the covered employee, divorce or legal separation of the covered employee from the covered employee's spouse, or the covered employee becoming entitled to Medicare, COBRA for the spouse or dependent child lasts for 36 months.