Cobra Coverage For 2 Weeks
Description
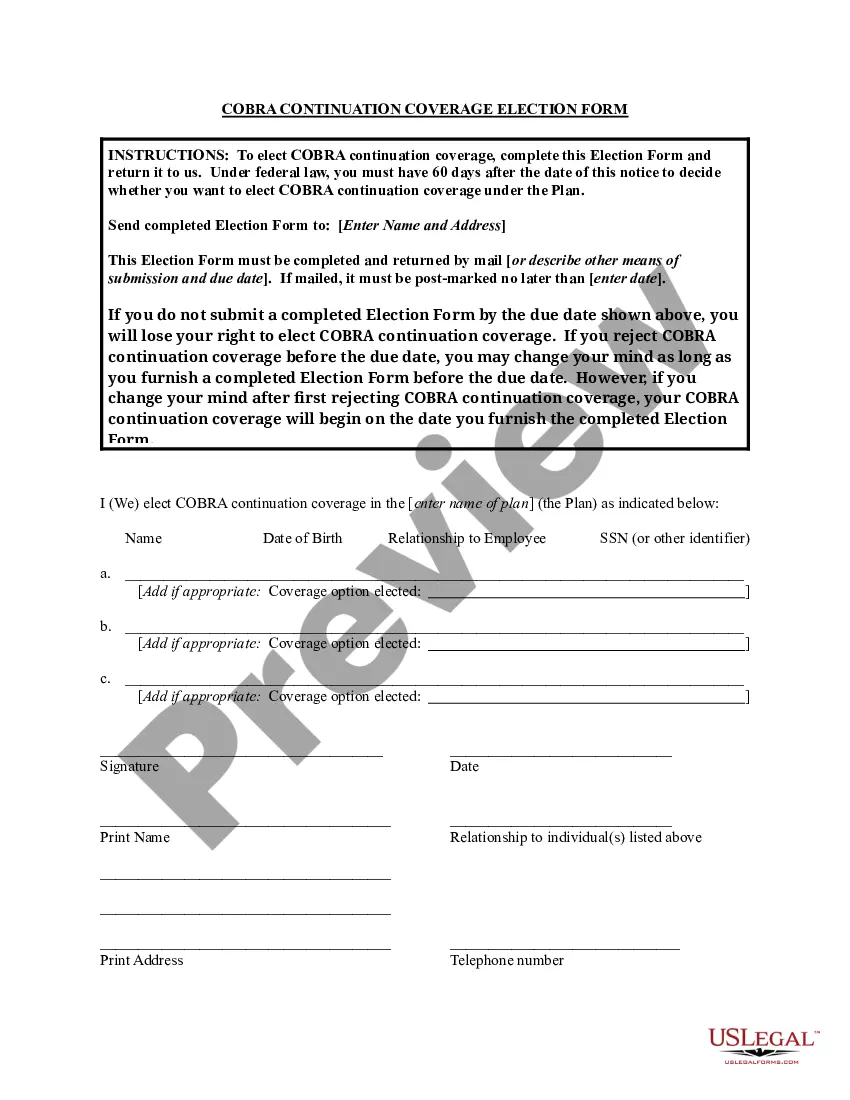
How to fill out Model COBRA Continuation Coverage Election Notice?
You no longer have to spend time searching for legal documents to fulfill your local state obligations. US Legal Forms has compiled all of them in one location and made them easier to access.
Our website features over 85,000 templates for various business and personal legal matters sorted by state and applicable area. All forms are properly created and verified for accuracy, ensuring you can confidently obtain an updated Cobra Coverage For 2 Weeks.
If you are already acquainted with our platform and possess an account, ensure that your subscription is active before accessing any templates. Log In to your account, select the document, and click Download. You can also revisit all downloaded documents as needed by accessing the My documents section in your profile.
Print your form to fill it out by hand or upload the document if you wish to complete it in an online editor. Creating legal documents according to federal and state regulations is quick and straightforward with our platform. Experience US Legal Forms today to keep your paperwork organized!
- If you've never used our platform before, the process will require a few additional steps to complete. Here's how new users can locate the Cobra Coverage For 2 Weeks in our catalog.
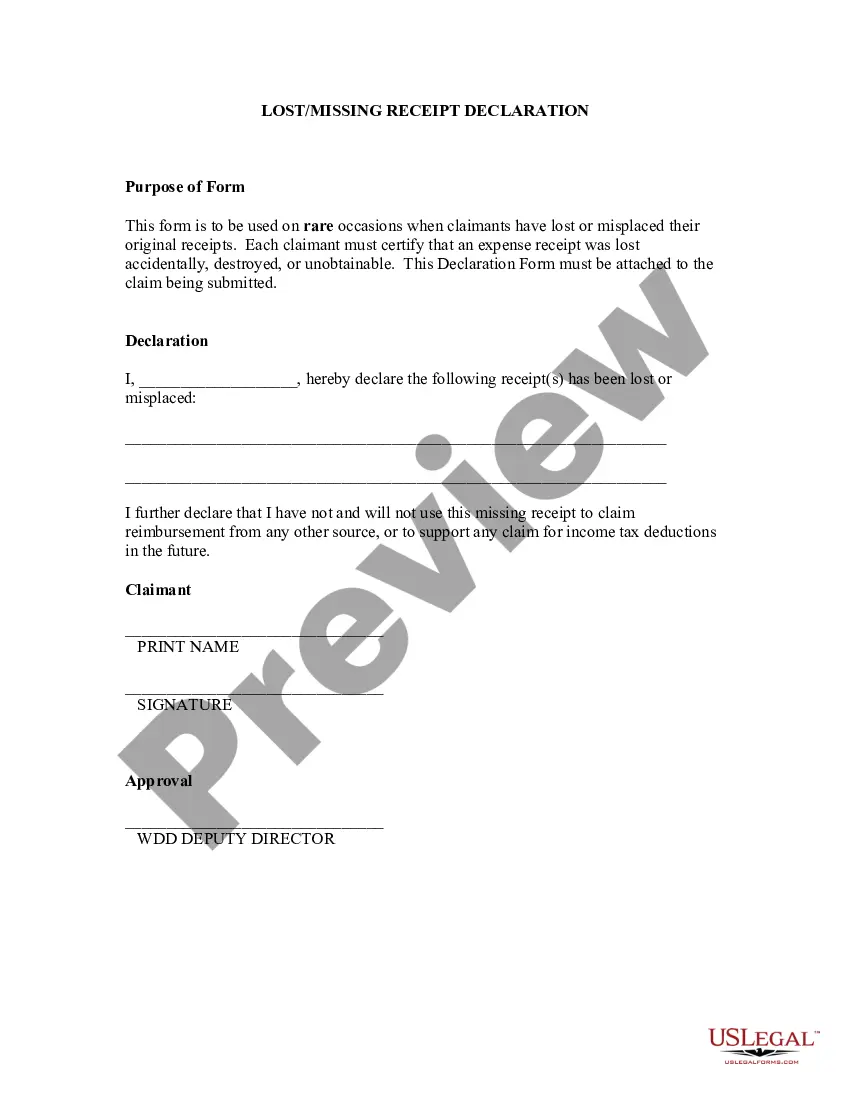
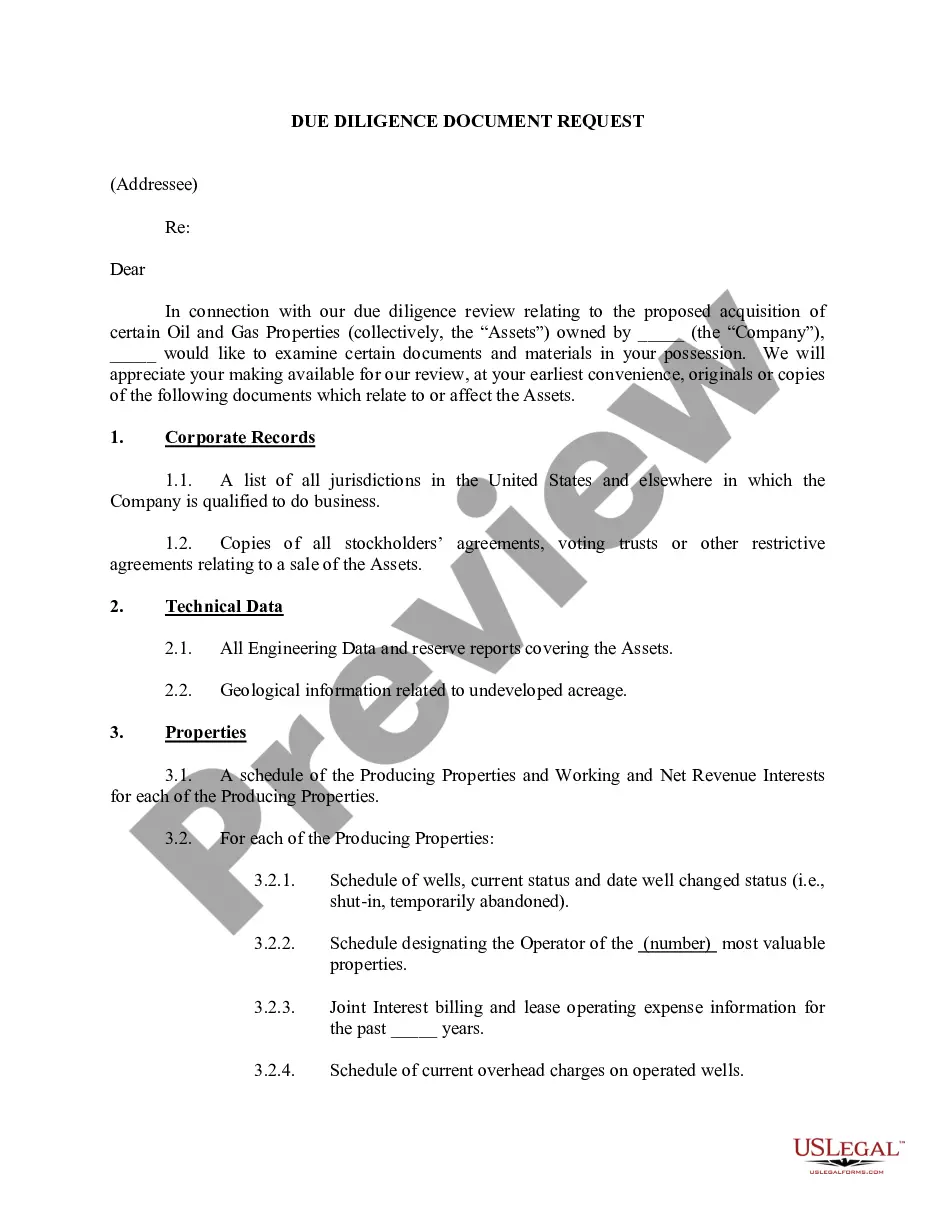
- Review the page content thoroughly to ensure it contains the sample you need.
- To assist, use the form description and preview options if available.
- Employ the Search bar above to look for another template if the current one doesn't meet your needs.
- Click Buy Now next to the template title when you identify the correct one.
- Select the preferred pricing plan and either register for an account or sign in.
- Complete your payment for the subscription via credit card or PayPal to proceed.
- Select the file format for your Cobra Coverage For 2 Weeks and download it to your device.
Form popularity
FAQ
Yes, you can elect COBRA coverage for 2 weeks if that fits your needs, but it’s essential to follow the specific election timeline outlined by your employer. It's not uncommon to want short-term coverage during transitions, and COBRA is designed to offer flexibility in such situations. If you need help navigating the process, consider using the US Legal Forms platform to simplify managing your COBRA coverage options.
The benefits of COBRA can begin almost immediately upon election and first premium payment, assuming you act quickly. Once you formally elect COBRA coverage for 2 weeks and make the necessary payments, your coverage should start almost right away. This allows you to quickly secure healthcare during a time of transition.
While COBRA coverage does not start immediately, you can elect coverage within a specified period after receiving the notice from your employer. After you elect coverage, your health insurance benefits can go back as far as your last day of work, ensuring you have the protection you need. This is especially relevant for those looking for COBRA coverage for 2 weeks while transitioning.
COBRA coverage does not automatically begin the day you quit your job. Instead, it starts when your employer notifies you about your COBRA rights after your employment ends. This process ensures you receive the right information to understand your options for COBRA coverage for 2 weeks and potentially longer.
The COBRA loophole for 60 days allows you to delay your election of coverage for a limited period. You can choose to enroll in Cobra coverage for 2 weeks anytime within these 60 days. This means you can review your options and even explore other health insurance plans before making a decision. However, keep in mind that failing to elect coverage within this timeframe may result in losing your right to COBRA.
After a qualifying event, an employer has up to 14 days to provide you with a COBRA election notice. This notice will explain your coverage options and the process for obtaining Cobra coverage for 2 weeks. If you do not receive this notice within the 14-day window, it is advisable to reach out directly to your plan administrator for assistance. Timely access to your information is key to ensuring your coverage.
To initiate Cobra coverage for 2 weeks, you need to notify your employer or your plan administrator within the required time frame. Typically, you will receive a COBRA election notice after your employment ends. Following that, carefully fill out the election form and return it by the deadline specified in the notice. If you have questions, uslegalforms can guide you through the process to ensure you don’t miss any important steps.
Yes, you can do COBRA for 2 weeks, making it a viable option for short-term health coverage. This approach is particularly useful if you need temporary insurance while transitioning between jobs or waiting for new coverage to begin. By ensuring that you complete the necessary steps promptly, you can successfully secure COBRA coverage for 2 weeks and bridge any immediate healthcare needs.
The 14 day rule for COBRA refers to the time period an employer has to provide coverage after receiving your election form. Once you submit the COBRA election form, your employer must act within 14 days to ensure your coverage begins. This rule is crucial for those needing immediate access to healthcare; it reassures you that you can plan for COBRA coverage for 2 weeks without delays.
The maximum duration for COBRA coverage typically ranges from 18 to 36 months, depending on the qualifying event. For instance, if you've lost your job or had your hours reduced, you may qualify for the shorter term. This period allows you to maintain necessary health coverage while seeking new employment or making other arrangements. Understanding this timeframe ensures you can effectively utilize COBRA coverage for 2 weeks or longer.