Wisconsin Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
It is feasible to spend hours online seeking the proper legal document template that meets the federal and state specifications you need. US Legal Forms provides a vast array of legal forms that are reviewed by experts.
You can download or print the Wisconsin Qualifying Event Notice Information for Employer to Plan Administrator from my service.
If you have a US Legal Forms account, you can sign in and then click the Download button. Afterwards, you can complete, modify, print, or sign the Wisconsin Qualifying Event Notice Information for Employer to Plan Administrator. Every legal document template you purchase is yours indefinitely.
Choose the pricing plan you want, enter your details, and create a free account on US Legal Forms. Complete the transaction. You can use your credit card or PayPal account to pay for the legal form. Select the format of your document and download it to your system. Make changes to your document if necessary. You can fill out, amend, and sign and print the Wisconsin Qualifying Event Notice Information for Employer to Plan Administrator. Download and print numerous document layouts using the US Legal Forms website, which offers the largest collection of legal forms. Utilize professional and state-specific templates for your business or personal needs.
- To obtain another copy of the purchased form, navigate to the My documents tab and click the corresponding button.
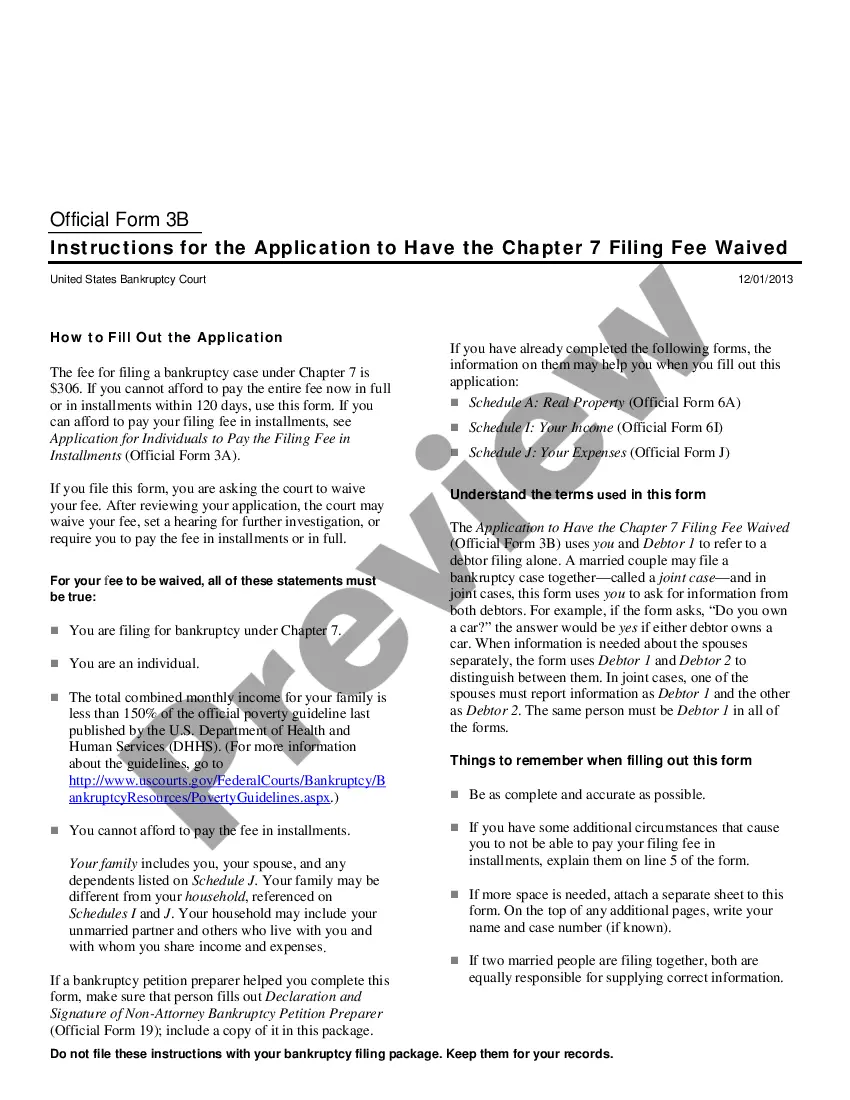
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document template for the area/region of your choice.
- Read the form description to confirm you have selected the appropriate form.
- If available, utilize the Preview button to review the document template as well.
- To acquire another version of your form, use the Search field to find the template that fits your needs and requirements.
- Once you have found the template you need, click Buy now to proceed.
Form popularity
FAQ
You can cancel your COBRA coverage at any time, but obtaining a refund can be a bit trickier. Typically, once you make a payment for COBRA coverage, it is non-refundable. However, if you canceled your coverage before the start date or within the grace period, you may be eligible for a refund. To navigate these nuances effectively, consider seeking Wisconsin Qualifying Event Notice Information for Employer to Plan Administrator through our platform, US Legal Forms, to ensure compliance and clarity in your processes.
The 60-day loophole for COBRA allows employees and beneficiaries to delay their decision about continuing health coverage for up to 60 days after receiving the initial notice. This period provides critical time to consider options without immediate pressure. It is important for employers to properly communicate this timeline, ensuring compliance with Wisconsin Qualifying Event Notice Information for Employer to Plan Administrator. Clarity in the communication helps employees make empowered decisions regarding their health benefits.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
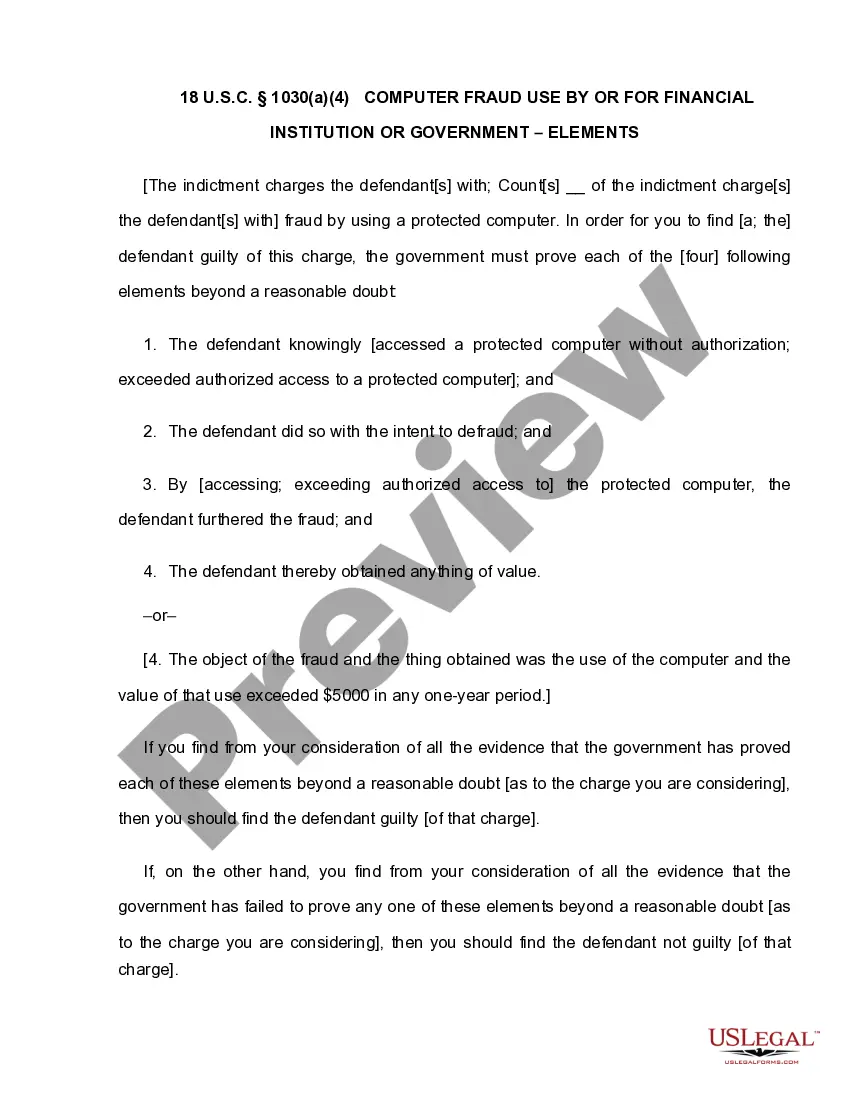
1. Plan Coverage Group health plans for employers with 20 or more employees on more than 50 percent of its typical business days in the previous calendar year are subject to COBRA. Both full and part-time employees are counted to determine whether a plan is subject to COBRA.
Federal Law (COBRA) Under federal law, employees who have a reduction in work hours or terminate employment for any reason other than gross misconduct may continue their group coverage for up to 18 months. (A spouse and dependents are also covered.)
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Federal Law (COBRA) Under federal law, employees who have a reduction in work hours or terminate employment for any reason other than gross misconduct may continue their group coverage for up to 18 months. (A spouse and dependents are also covered.)
To be eligible for COBRA coverage, you must have been enrolled in your employer's health plan when you worked and the health plan must continue to be in effect for active employees.