Wisconsin Notice of Qualifying Event from Employer to Plan Administrator
Description
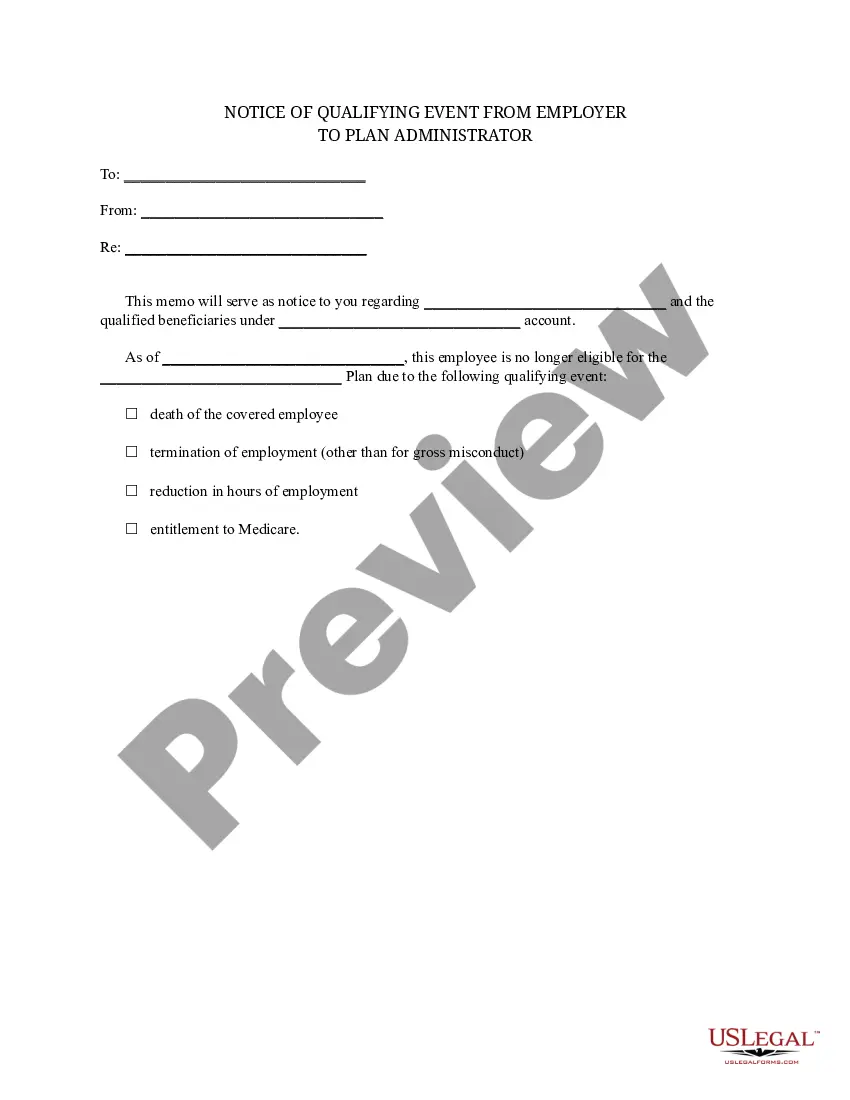
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
You can spend hours online attempting to locate the valid document template that meets the federal and state requirements you will need.
US Legal Forms offers thousands of valid templates that have been examined by experts.
It is easy to download or print the Wisconsin Notice of Qualifying Event from Employer to Plan Administrator from the service.
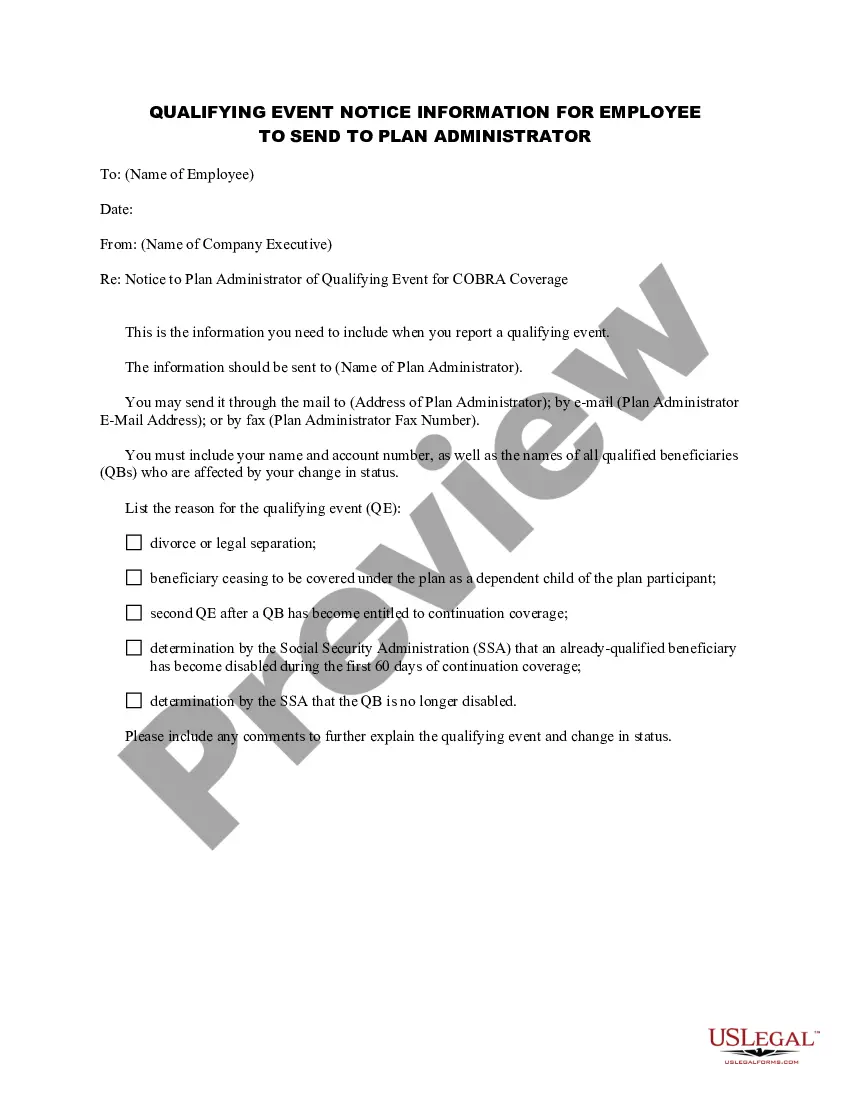
If available, use the Preview button to browse through the document template as well.
- If you already possess a US Legal Forms account, you may Log In and click on the Download button.
- Then you may complete, modify, print, or sign the Wisconsin Notice of Qualifying Event from Employer to Plan Administrator.
- Every valid document template you acquire is yours permanently.
- To obtain an additional copy of any acquired form, navigate to the My documents tab and click on the respective button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document template for your region/area of selection.
- Read the template description to confirm that you have chosen the right one.
Form popularity
FAQ
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Employees are eligible for 18 months of continued coverage under COBRA if the qualifying event stems from reduction of hours or termination of employment for reasons other than gross misconduct. Note that termination can be voluntary or involuntary, including retirement.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months. The length of time depends on the type of qualifying event that gave rise to Page 6 6 the COBRA rights.
Both Wisconsin law and the federal Consolidated Omnibus Budget Reconciliation Act (COBRA) permit employees to continue their group health coverage if they leave the group for certain specified reasons. According to federal law, employees may utilize the law that is most favorable to their situation.
If you are entitled to an 18 month maximum period of continuation coverage, you may become eligible for an extension of the maximum time period in two circumstances. The first is when a qualified beneficiary is disabled; the second is when a second qualifying event occurs.
If within the first 60 days of COBRA coverage an individual or dependent is determined by Social Security to be disabled, the disabled individual and other covered family members may continue coverage for up to 29 months.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under