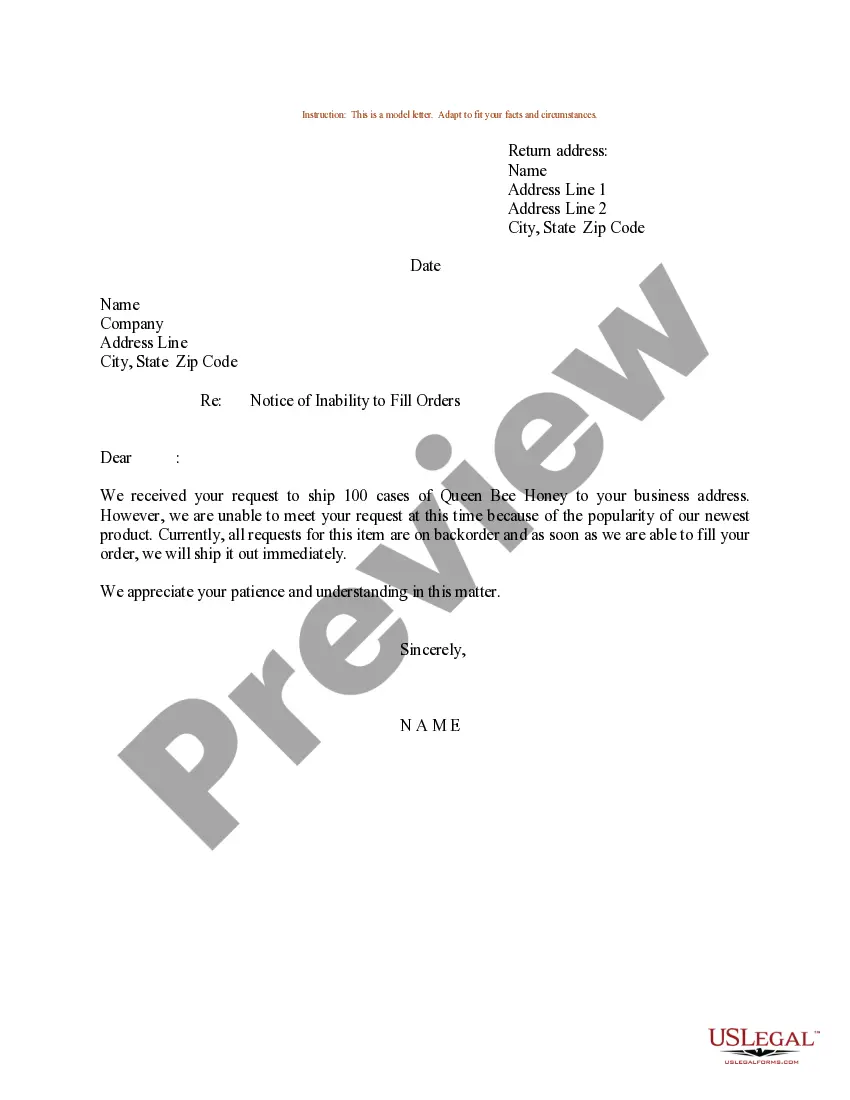
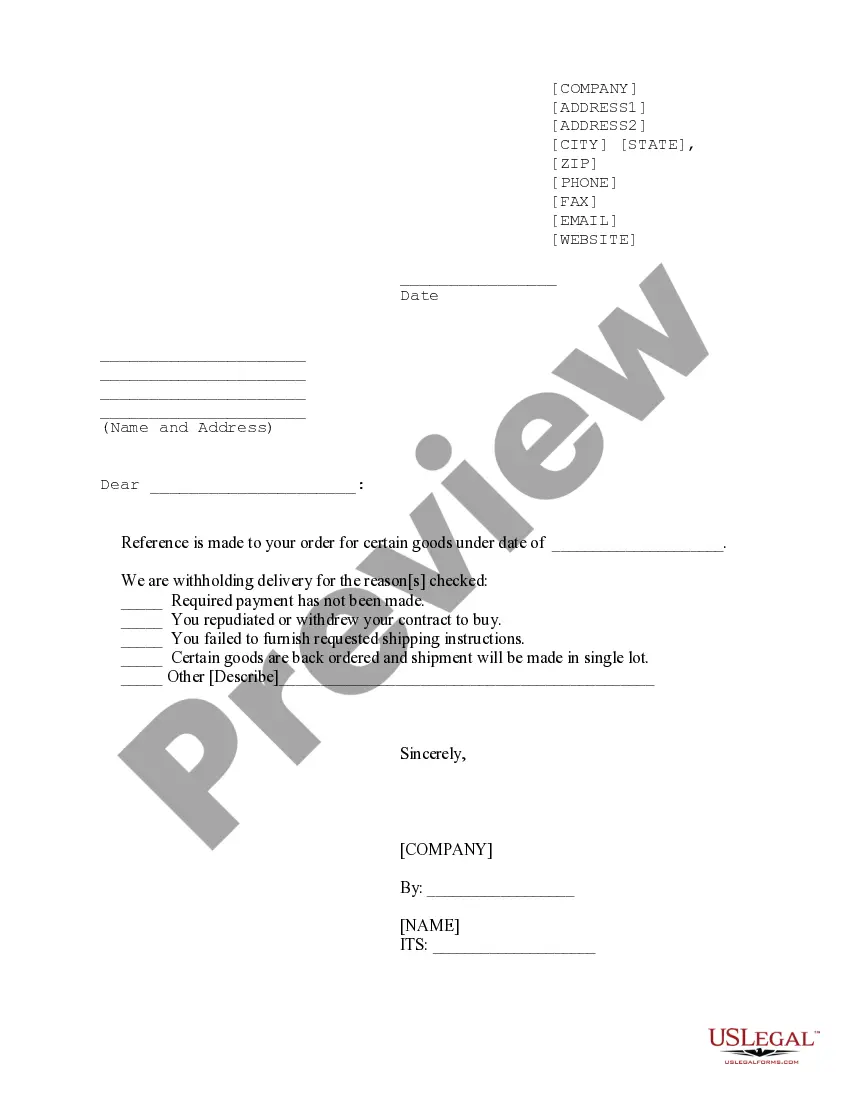
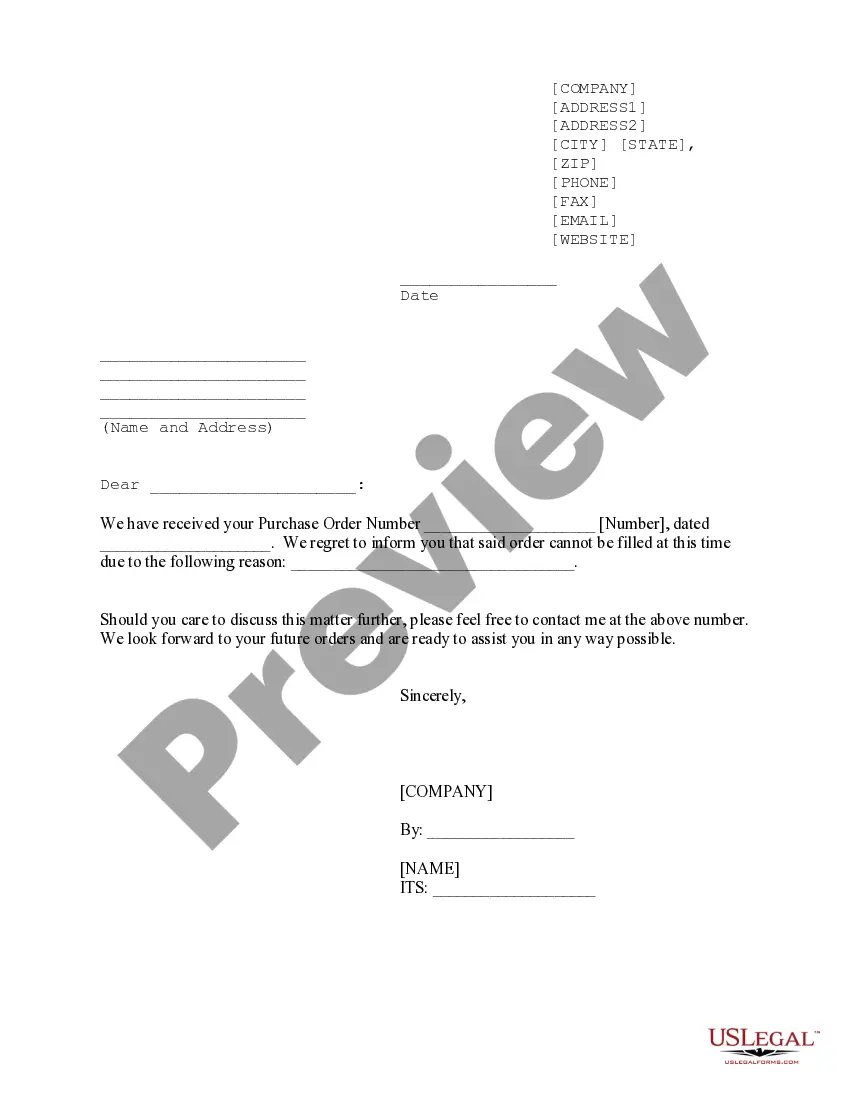
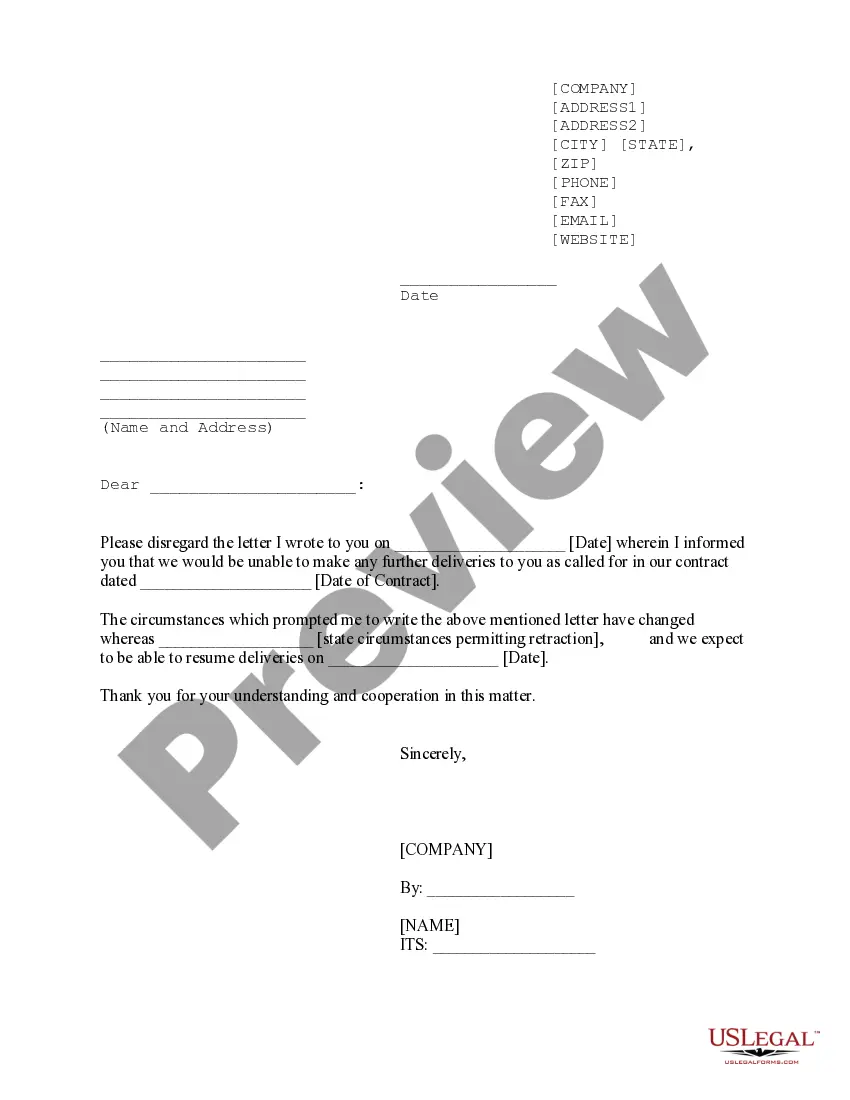
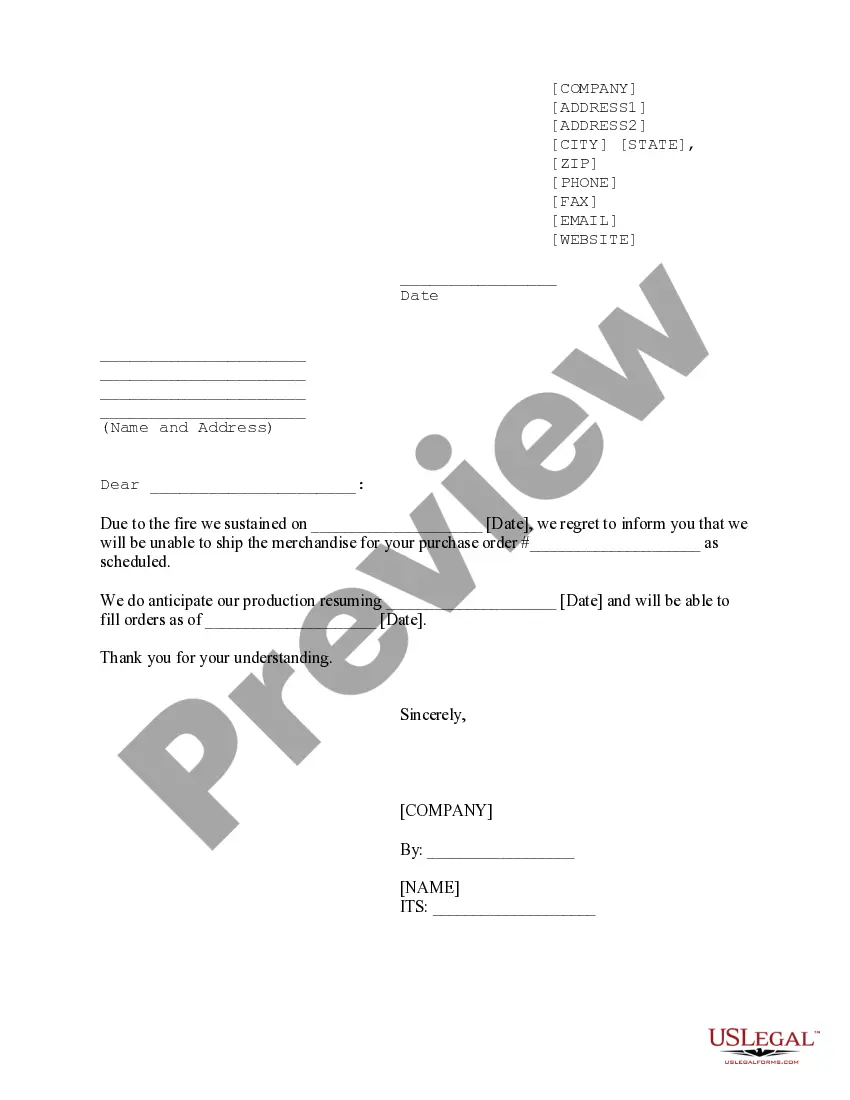
A Notice of Inability to Ship (also known as Non-Delivery Notice) is a document issued by a shipping carrier or freight forwarder to a customer when they are unable to ship goods for any reason. This notice may be sent via email, mail, or fax and includes the following information: • Details of the shipment: carrier, origin and destination, date of shipment, and shipment reference number. • Reason for the inability to ship, such as lack of shipping space, delay in customs clearance, or other unforeseen issues. • Suggested plan of action, such as alternate delivery options or a new estimated delivery date. There are two types of Notice of Inability to Ship: Non-Delivery Notice and Reschedule Notice. A Non-Delivery Notice is issued when a shipment cannot be delivered due to an unforeseen issue, such as lack of shipping space or delay in customs clearance. A Rescheduling Notice is issued when a shipment is delayed due to an unforeseen event, such as weather or mechanical issues.
Notice of Inability to Ship
Description
How to fill out Notice Of Inability To Ship?
Preparing official paperwork can be a real stress if you don’t have ready-to-use fillable templates. With the US Legal Forms online library of formal documentation, you can be certain in the blanks you find, as all of them correspond with federal and state regulations and are checked by our specialists. So if you need to prepare Notice of Inability to Ship, our service is the perfect place to download it.
Obtaining your Notice of Inability to Ship from our catalog is as simple as ABC. Previously registered users with a valid subscription need only log in and click the Download button after they find the correct template. Afterwards, if they need to, users can pick the same document from the My Forms tab of their profile. However, even if you are new to our service, registering with a valid subscription will take only a few moments. Here’s a brief guide for you:
- Document compliance verification. You should carefully examine the content of the form you want and make sure whether it suits your needs and complies with your state law requirements. Previewing your document and reviewing its general description will help you do just that.
- Alternative search (optional). Should there be any inconsistencies, browse the library using the Search tab on the top of the page until you find an appropriate template, and click Buy Now when you see the one you need.
- Account creation and form purchase. Sign up for an account with US Legal Forms. After account verification, log in and choose your most suitable subscription plan. Make a payment to proceed (PayPal and credit card options are available).
- Template download and further usage. Select the file format for your Notice of Inability to Ship and click Download to save it on your device. Print it to complete your paperwork manually, or use a multi-featured online editor to prepare an electronic version faster and more efficiently.
Haven’t you tried US Legal Forms yet? Subscribe to our service now to obtain any formal document quickly and easily any time you need to, and keep your paperwork in order!
Form popularity
FAQ
A Medicare provider or health plan (Medicare Advantage plans and cost plans , collectively referred to as ?plans?) must deliver a completed copy of the Notice of Medicare Non-Coverage (NOMNC) to beneficiaries/enrollees receiving covered skilled nursing, home health (including psychiatric home health), comprehensive
The NOMNC notifies a Medicare member, in writing, that the member's Medicare health plan and/or provider have decided to terminate the member's covered Home Health Agency (HHA), Skilled Nursing Facility (SNF), or Comprehensive Outpatient Rehabilitation Facility (CORF) care and, as a result of the termination of
The NOMNC informs beneficiaries on how to request an expedited determination from their Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) and gives beneficiaries the opportunity to request an expedited determination from a BFCC-QIO.
To complete a DE 2501 Form you will need to provide the following information: Health Insurance Portability and Accountability Act (HIPAA) Authorization. Social security number. Name.Claimant's Statement. Social security number. EDD customer account number.Physician/Practitioner's Certificate. Patient's SSN.
"Hospital Issued Notice of Noncoverage" (HINN): Hospitals use a HINN when Medicare may not cover all or part of your Part A inpatient hospital care. This notice will tell you why the hospital thinks Medicare won't pay, and what you may have to pay if you keep getting these services.
Beneficiaries who are receiving covered skilled nursing (including. physical therapy), home health, outpatient rehabilitation, or. hospice services. ? The NOMNC must be given when the last skilled service is to be. discontinued.Medicare-covered services end (Effective Date) or the second to.
Hospices are required to provide a Notice of Medicare Non-Coverage (NOMNC) expedited determination notices are given to beneficiaries when all Medicare covered services are being terminated when no longer terminally ill Hospice must provide the Notice of Medicare Provider Non-Coverage (Generic Notice) to Medicare
The NOMNC must be delivered at least two calendar days before Medicare covered services end or the second to last day of service if care is not being provided daily.