Massachusetts Individual Notice of Preexisting Condition Exclusion
Description
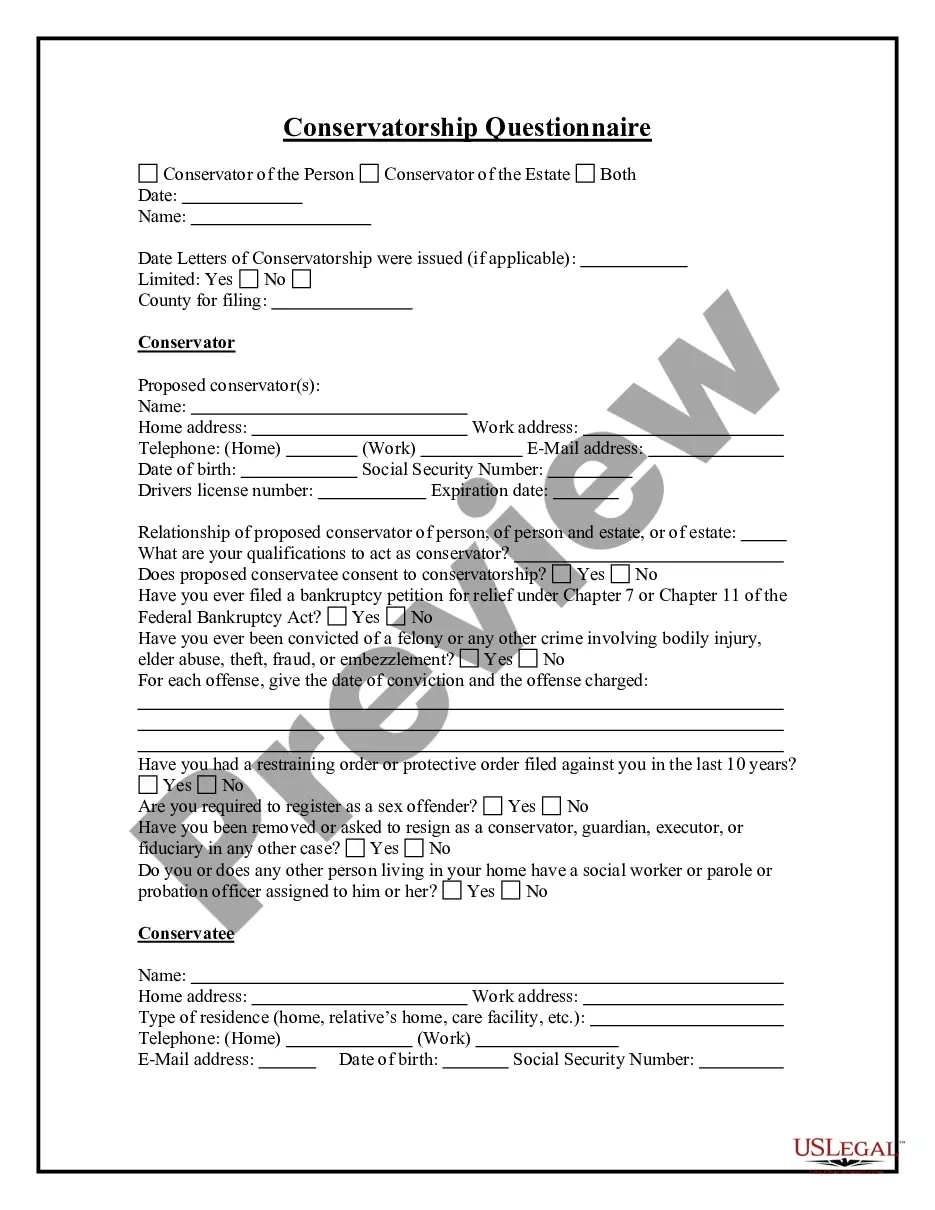
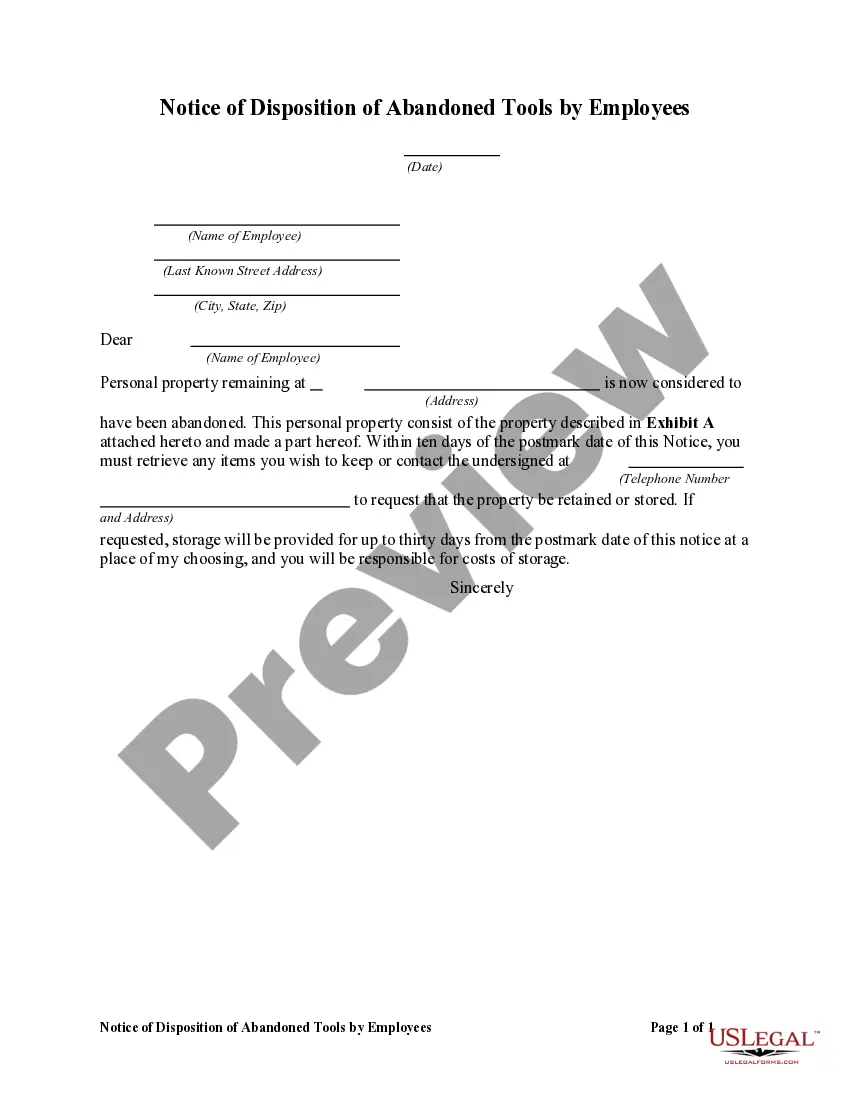
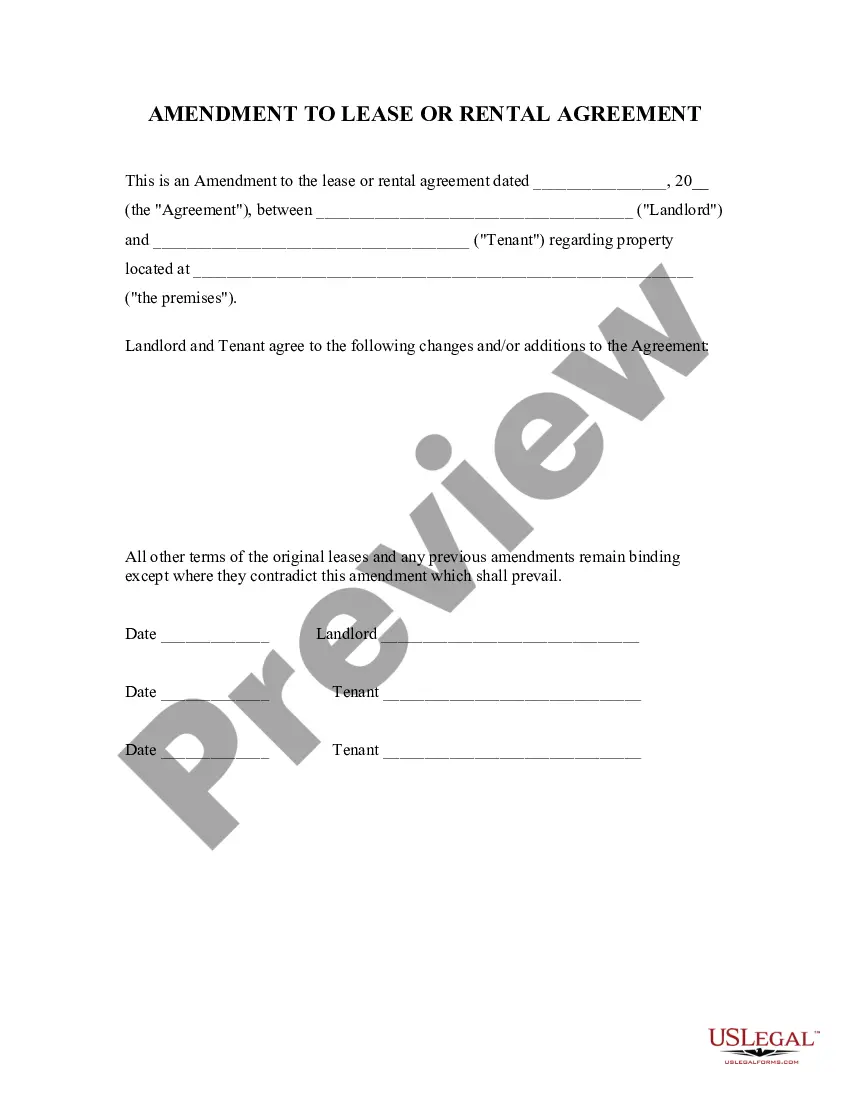
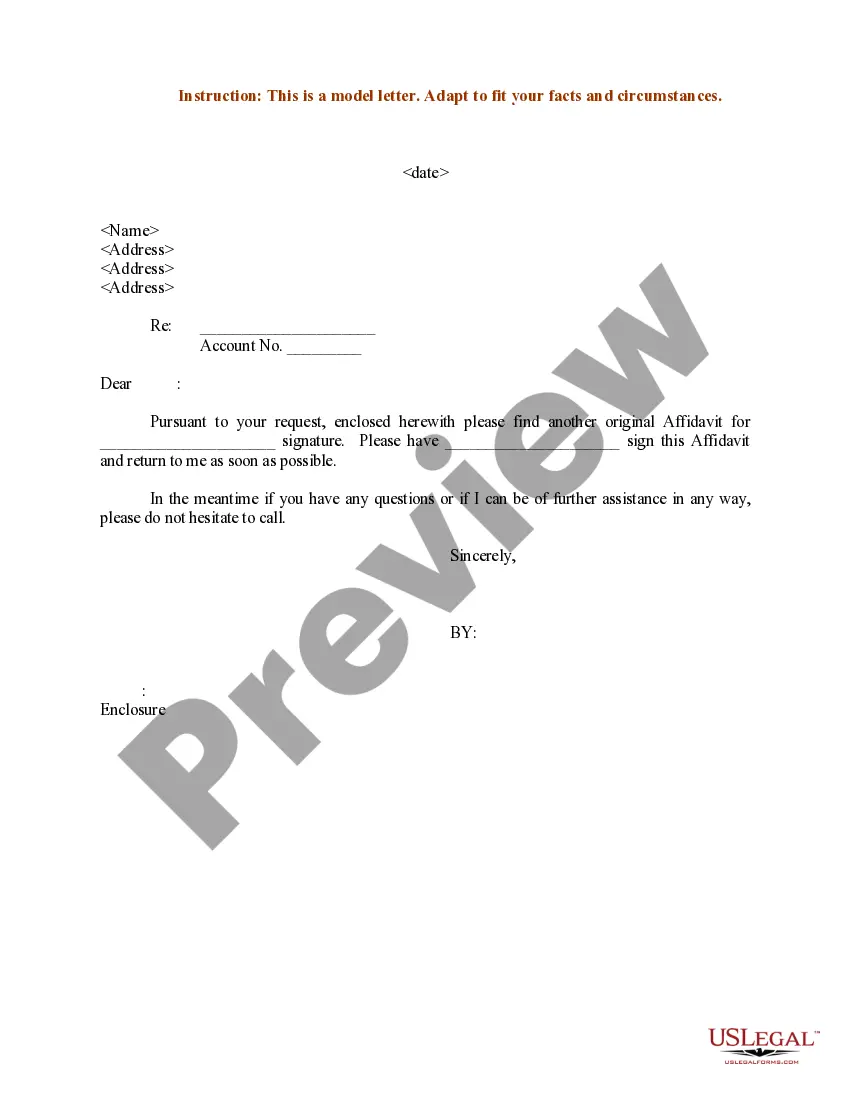
How to fill out Individual Notice Of Preexisting Condition Exclusion?
Are you in a circumstance where you need documents for various business or personal reasons almost every day.
There are numerous legal document templates accessible online, but locating ones you can trust is challenging.
US Legal Forms provides thousands of form templates, including the Massachusetts Individual Notice of Preexisting Condition Exclusion, designed to comply with state and federal requirements.
Once you find the appropriate form, click Purchase now.
Select the pricing plan you want, complete the required information to create your account, and finalize the purchase with your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Then, you can download the Massachusetts Individual Notice of Preexisting Condition Exclusion template.
- If you do not have an account and wish to start using US Legal Forms, follow these instructions.
- Obtain the form you require and ensure it is for the correct city/region.
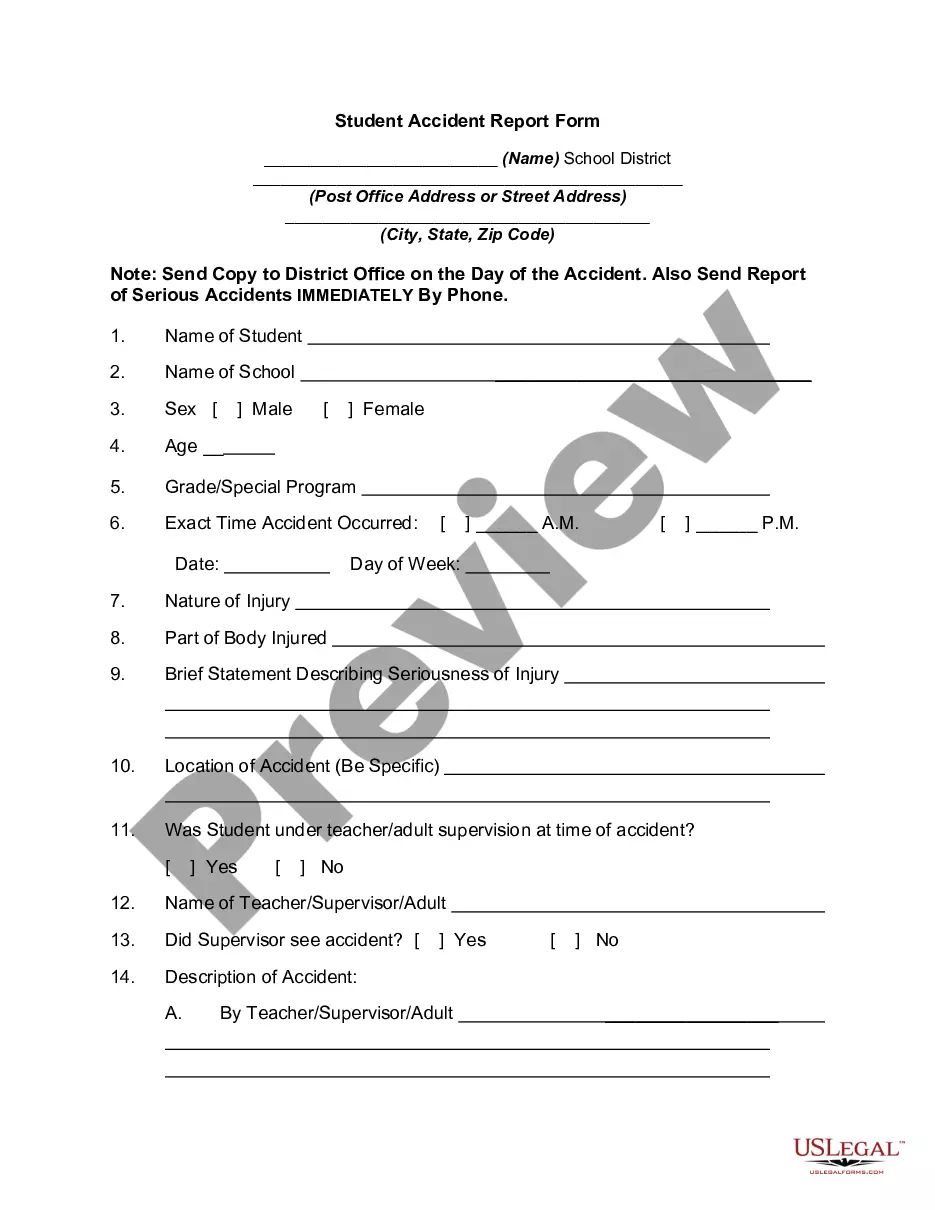
- Utilize the Preview button to examine the form.
- Review the description to confirm you have selected the correct form.
- If the form isn't what you need, use the Search field to find the form that fits your criteria and needs.
Form popularity
FAQ
Yes. Under the Affordable Care Act, health insurance companies can't refuse to cover you or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Some of the most common pre-existing conditions include thyroid, high blood pressure, diabetes, asthma, cholesterol, etc. Most health insurance companies have a waiting period that can last from a couple of months to a few years before you start covering pre-existing illnesses.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
If you had a pre-existing condition exclusion period, you didn't have coverage for any care or services related to your pre-existing condition for a predetermined amount of time, despite paying your monthly premiums.
In Massachusetts, health plans cannot deny health insurance coverage for an individual because that person has a pre-existing condition. However, health plans can limit coverage of that specific condition for up to six months, unless the person has had continuous health insurance coverage.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.