Massachusetts Notice of Special Enrollment Rules
Description
How to fill out Notice Of Special Enrollment Rules?
US Legal Forms - one of the most notable collections of legal documents in the United States - provides a vast selection of legal document templates that you can either obtain or create. By using the website, you can access thousands of documents for business and personal purposes, categorized by type, region, or keywords.
You can find the latest versions of documents such as the Massachusetts Notice of Special Enrollment Rules in just a few moments.
If you already have an account, Log In to obtain the Massachusetts Notice of Special Enrollment Rules from your US Legal Forms library. The Download button will appear on every document you view. You have access to all previously saved documents in the My documents section of your account.
Select the format and download the document to your device.
Make modifications. Fill out, edit, print, and sign the saved Massachusetts Notice of Special Enrollment Rules.
- If you are using US Legal Forms for the first time, here are some straightforward steps to get started.
- Ensure you have selected the correct form for your location/region.
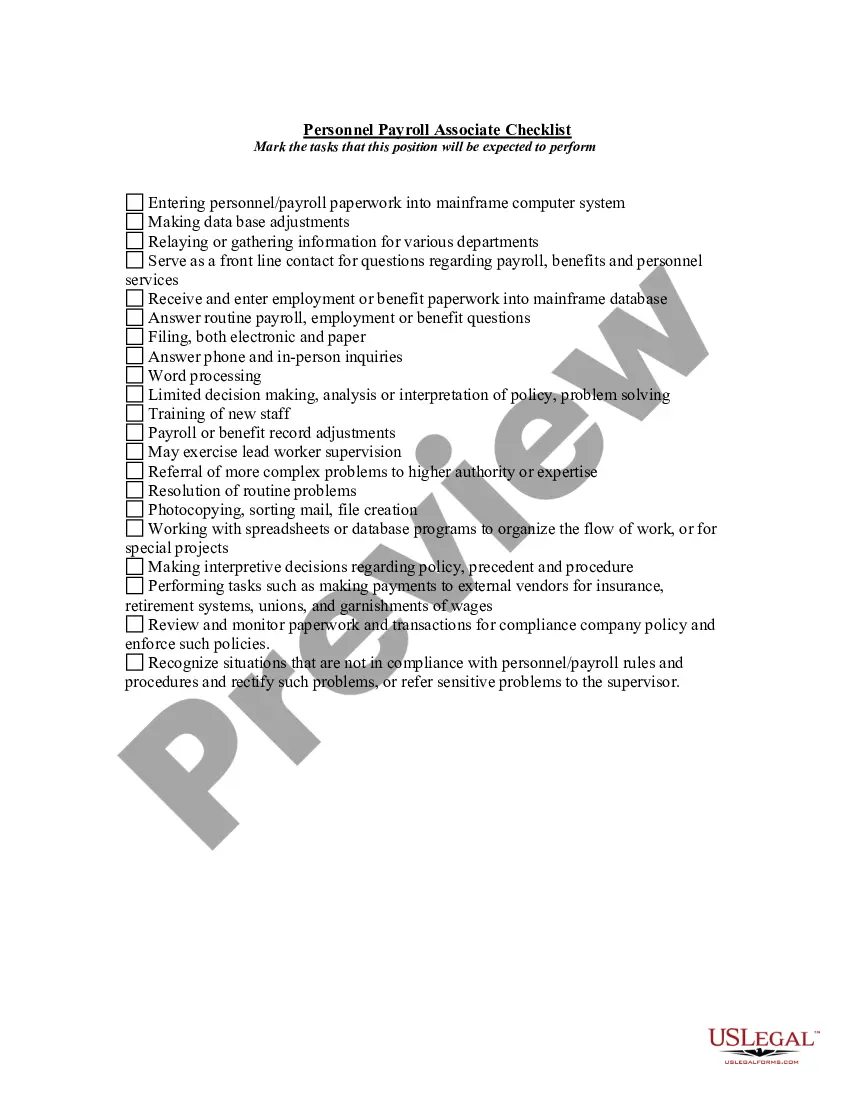
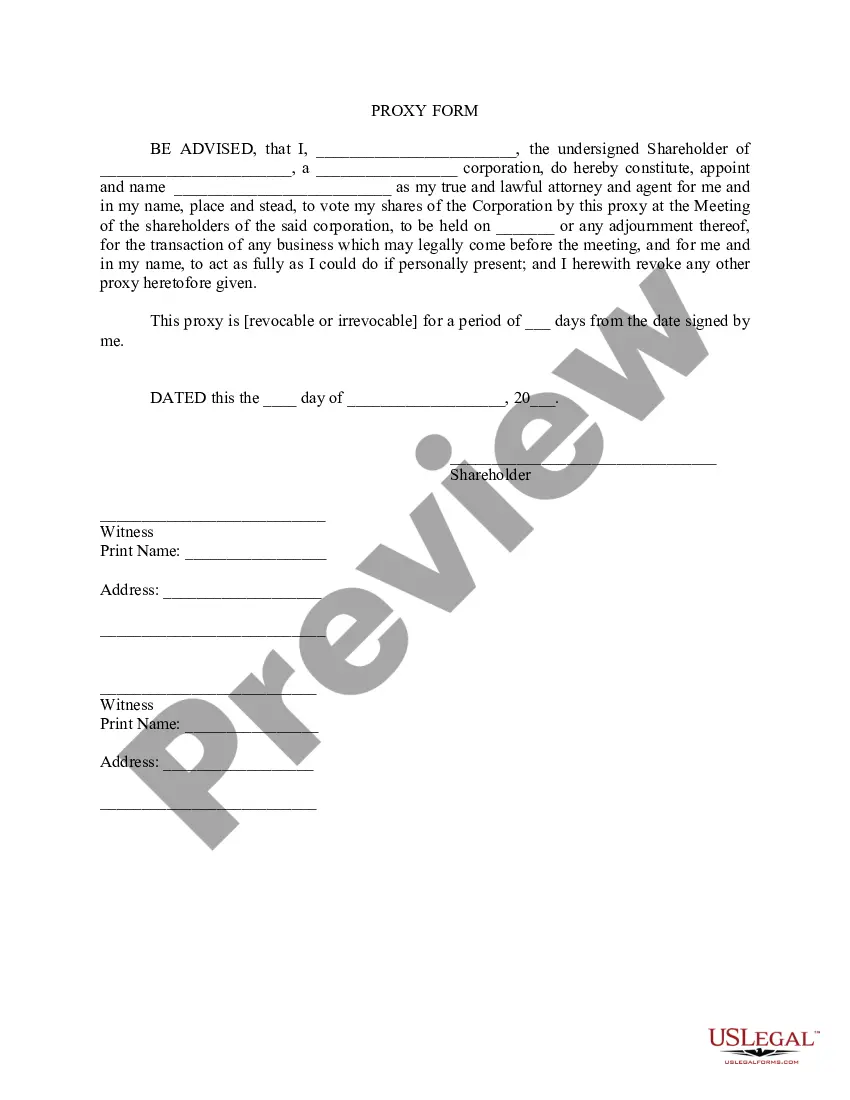
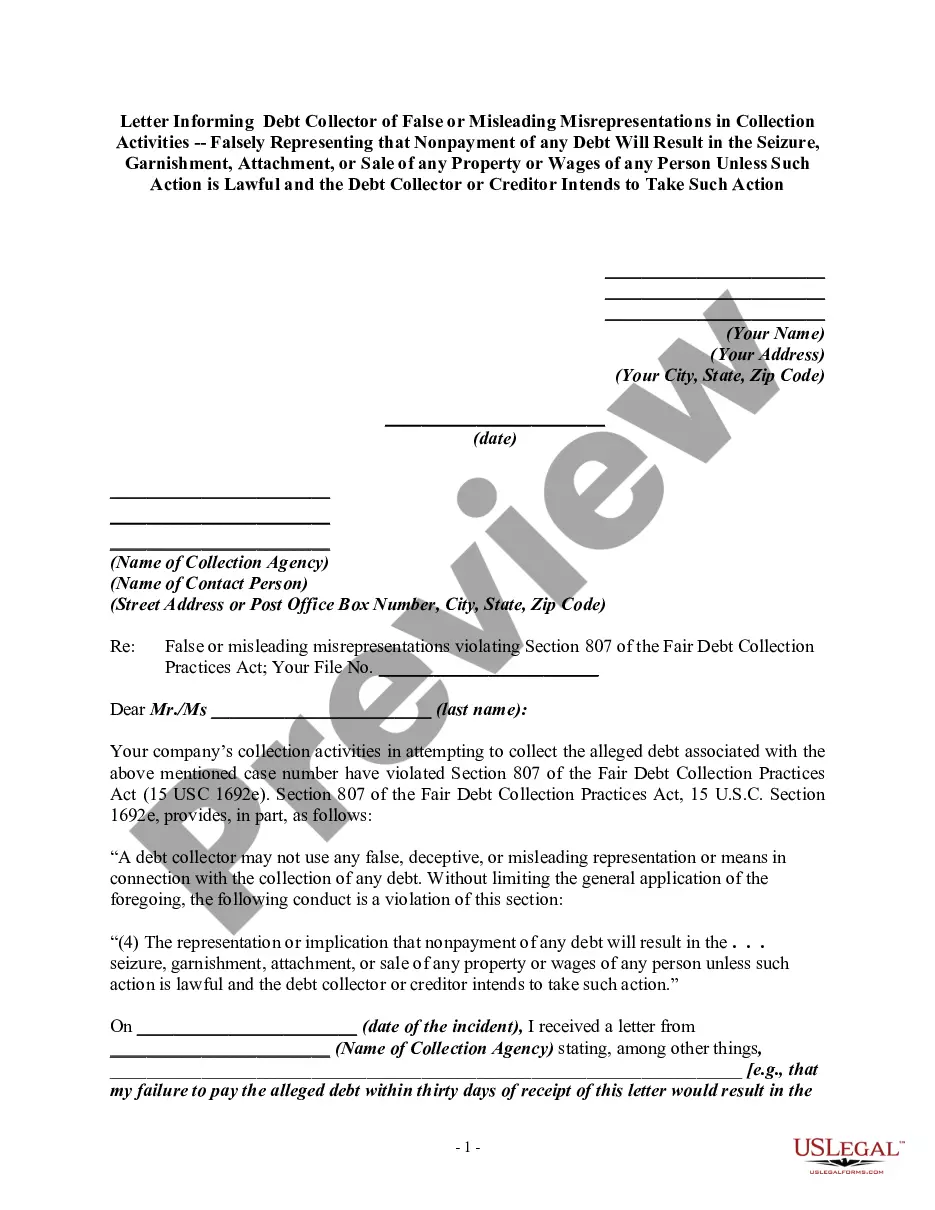
- Click the Preview option to examine the document’s details.
- Review the description of the document to make sure it is the correct one for your needs.
- If the document does not meet your requirements, utilize the Search field at the top of the screen to find the one that does.
- Once you are satisfied with the document, confirm your selection by clicking the Buy now button. Then, choose your preferred payment plan and provide your details to create an account.
- Process the payment. Use your credit card or PayPal account to finalize the transaction.
Form popularity
FAQ
A change in your situation like getting married, having a baby, or losing health coverage that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
You may apply for MassHealth at any time during the year. You DO NOT need an open enrollment waiver from OPP to apply for MassHealth. Please visit MASSHEALTH or call their customer service line at 1-800-841-2900 for eligibility, benefits, or other helpful information.
A change in your situation like getting married, having a baby, or losing health coverage that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
Open Enrollment Period (1) The period of time designated by the employer's health or other benefit plan when employees may enroll in new benefit plans or make changes to existing benefit plans.
Normally, coverage is only available for purchase during the annual open enrollment period, but a special enrollment period allows people to sign up for coverage outside of that annual window, as long as they have a qualifying event.
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
Special enrollment periods are typically 60-days long and will allow you to purchase major medical insurance.
Period of enrollment means the period that the title IV institution has established for which institutional charges are generally assessed (i.e., length of the student's course, program, or academic year.)
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.