Cobra Coverage Complete Without
Description
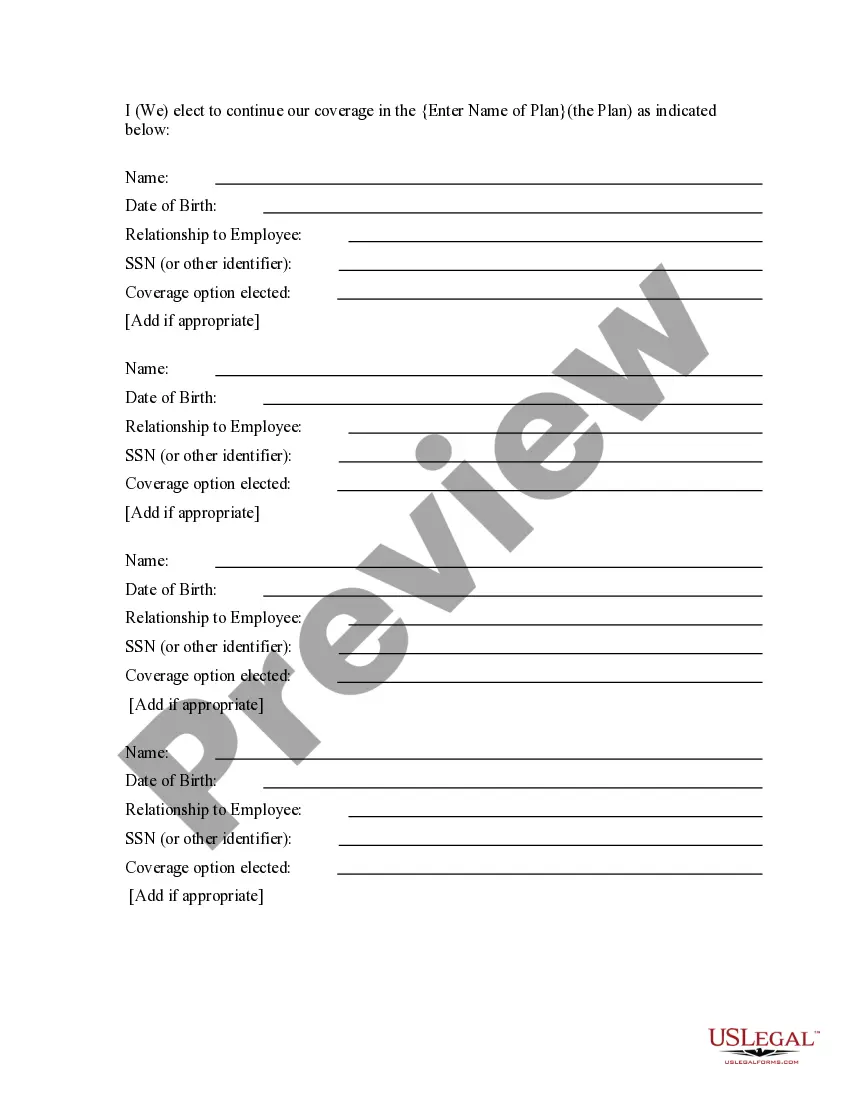
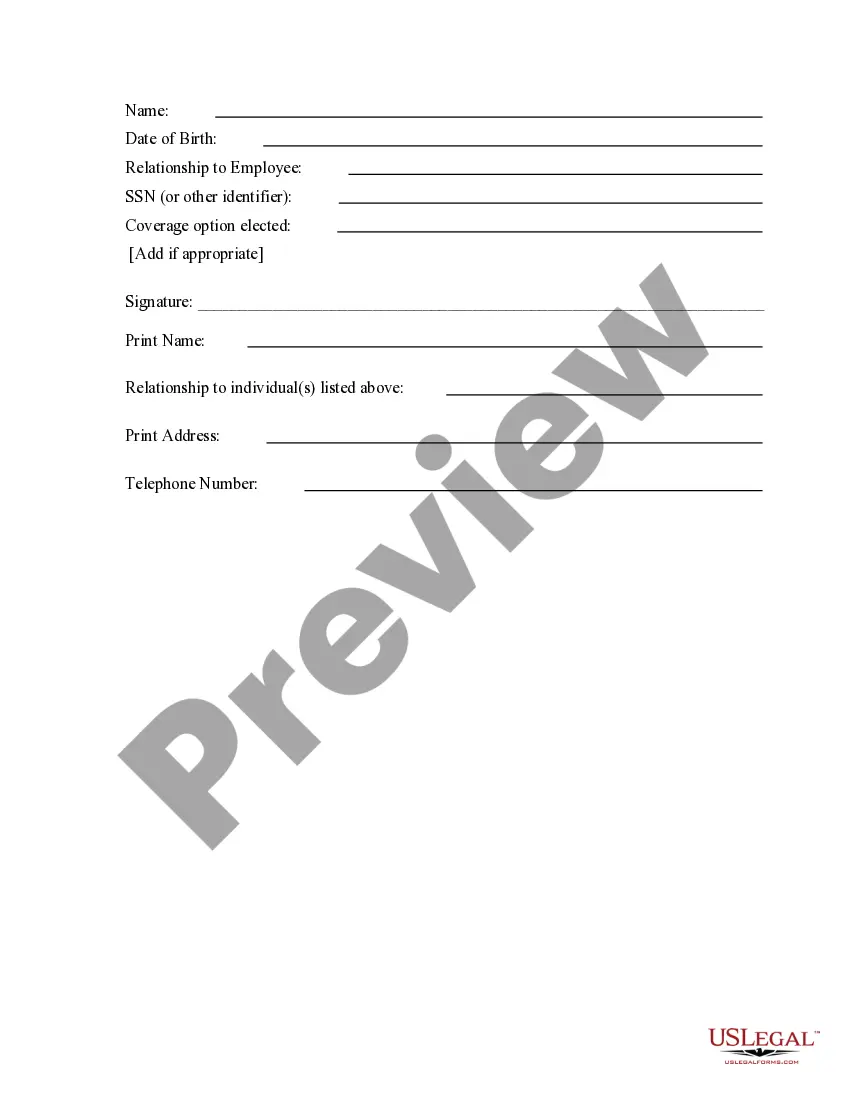
How to fill out COBRA Continuation Coverage Election Form?
Whether for commercial aims or personal affairs, everyone must confront legal matters at some stage in their life.
Filling out legal paperwork requires meticulous care, beginning with selecting the correct form template.
With an extensive US Legal Forms directory available, you don’t have to waste time searching for the suitable sample throughout the web. Make use of the library’s straightforward navigation to find the correct template for any circumstance.
- Locate the example you require by using the search bar or browsing the catalog.
- Review the description of the form to ensure it aligns with your circumstance, state, and county.
- Click on the form’s preview to inspect it.
- If it is the incorrect document, return to the search feature to find the Cobra Coverage Complete Without example you need.
- Download the document when it fits your requirements.
- If you have a US Legal Forms account, simply click Log in to access previously saved templates in My documents.
- If you do not possess an account yet, you can acquire the form by clicking Buy now.
- Choose the correct pricing plan.
- Fill out the profile registration form.
- Select your payment method: you can utilize a credit card or PayPal.
- Choose the file format you desire and download the Cobra Coverage Complete Without.
- Once it is downloaded, you can complete the form with editing software or print it and finish it by hand.
Form popularity
FAQ
Yes, there are cheaper alternatives to COBRA that you can consider. For example, Medicaid and subsidized marketplace insurance can provide more budget-friendly options. Exploring these alternatives can help ensure you secure adequate coverage while avoiding the higher costs associated with COBRA coverage complete without losing essential health benefits. US Legal Forms offers resources to help you find the right coverage.
COBRA coverage can sometimes be less expensive than some employer-sponsored insurance options. However, many individuals find that COBRA premiums may still be higher than other available plans. It’s important to evaluate your specific situation and compare the costs and benefits of COBRA coverage complete without other insurance alternatives. Tools like US Legal Forms can help you understand your options better.
Applying for COBRA begins with the employer who provided the health plan to notify you of your right to continuation. The employer has 30 days to notify the group health plan of the qualifying event. After that, the employer has 14 days to notify you of your COBRA right to keep your work health insurance.
COBRA coverage is retroactive if elected and paid for by the qualified beneficiary.
There are three basic requirements that must be met in order for you to be entitled to elect COBRA continuation coverage: Your group health plan must be covered by COBRA; ? A qualifying event must occur; and ? You must be a qualified beneficiary for that event.
First, you should contact your former employer's human resources department to request a new copy of the paperwork. They may be able to send it to you electronically or by mail. If you are unable to obtain a new copy from your former employer, you can also contact the COBRA administrator for your health plan.
If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan. If you miss the deadline, you may lose the chance to sign up for Federal COBRA or Cal-COBRA. Call the Help Center if you have any questions.