Vermont Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
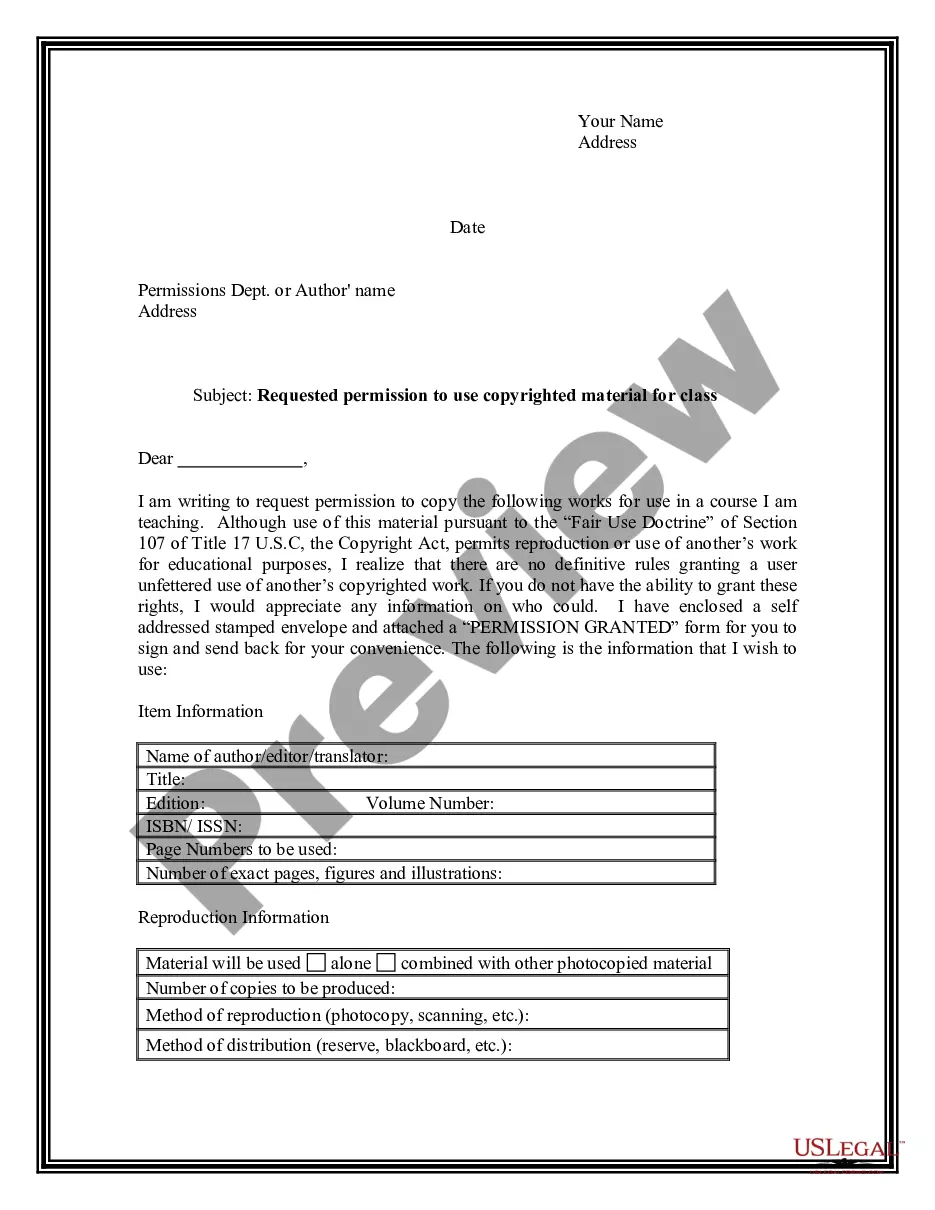
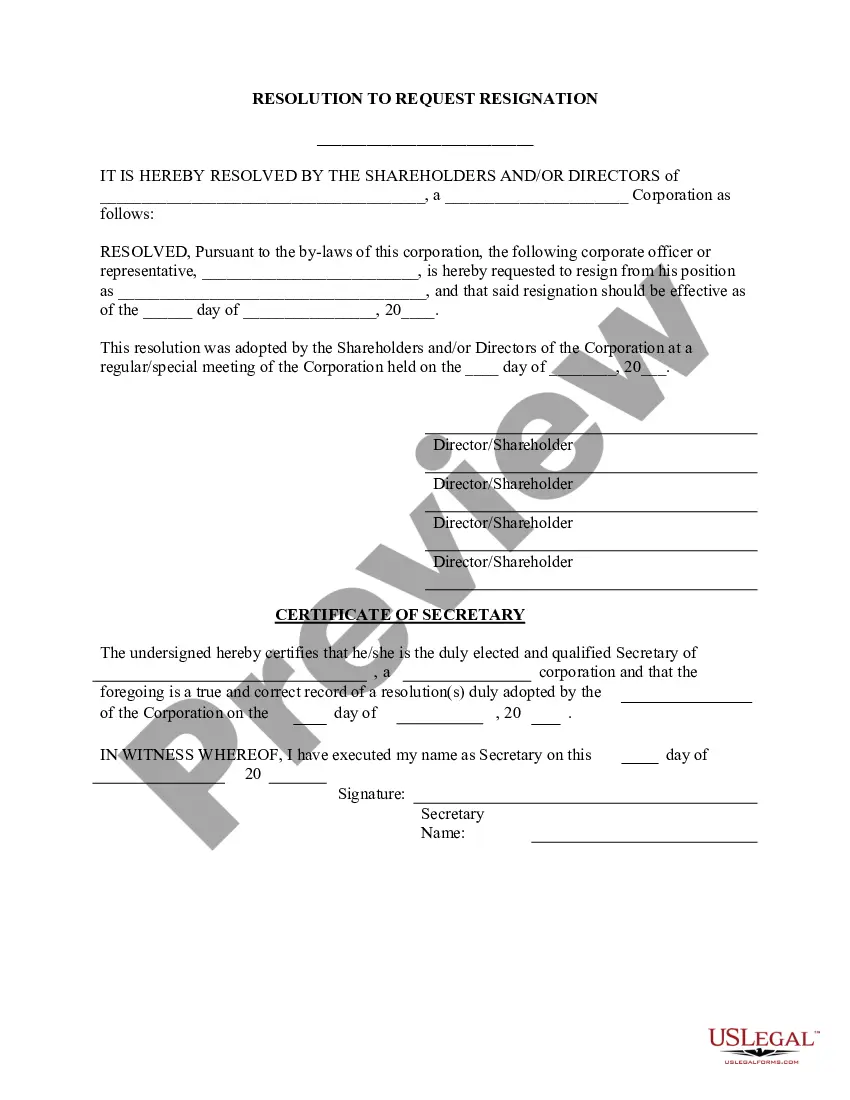
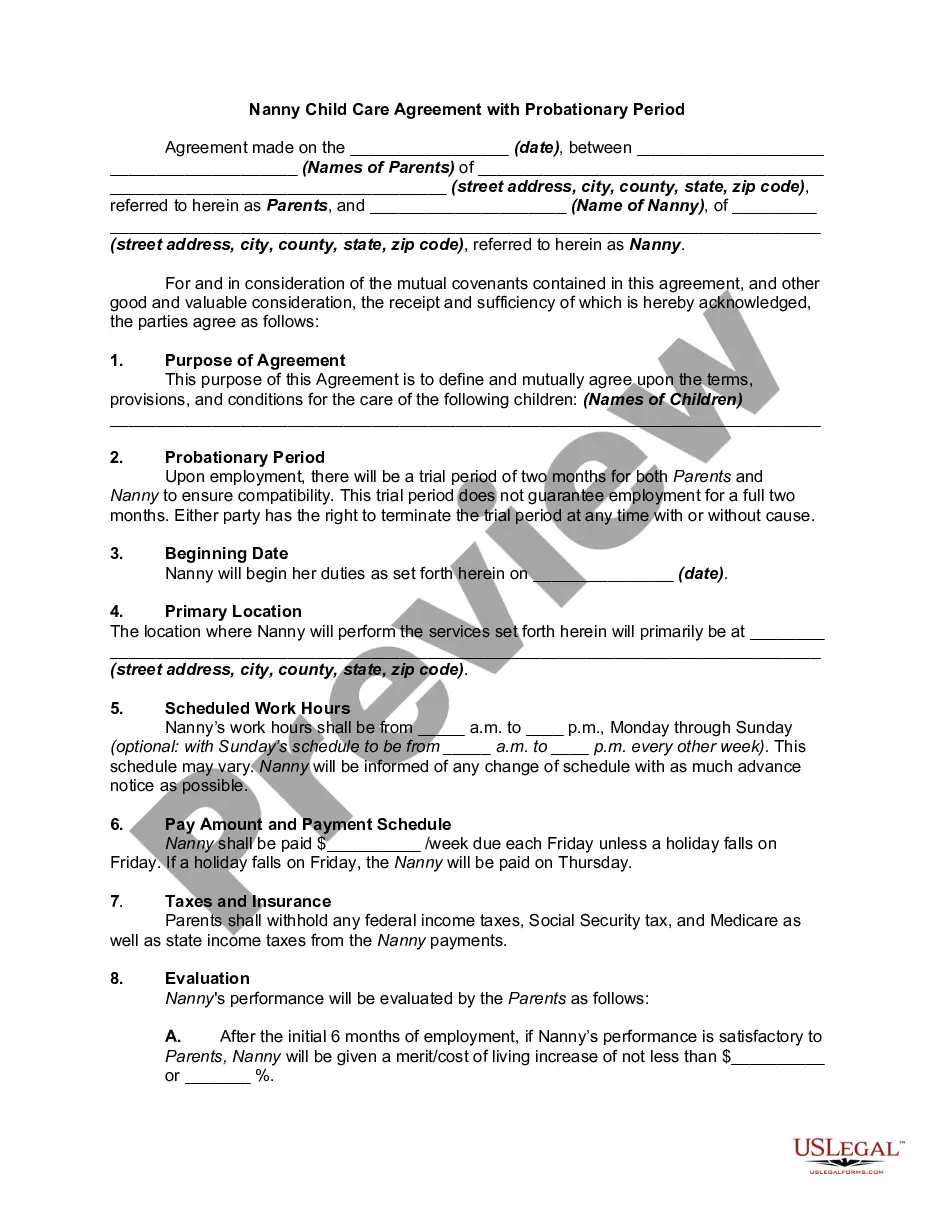
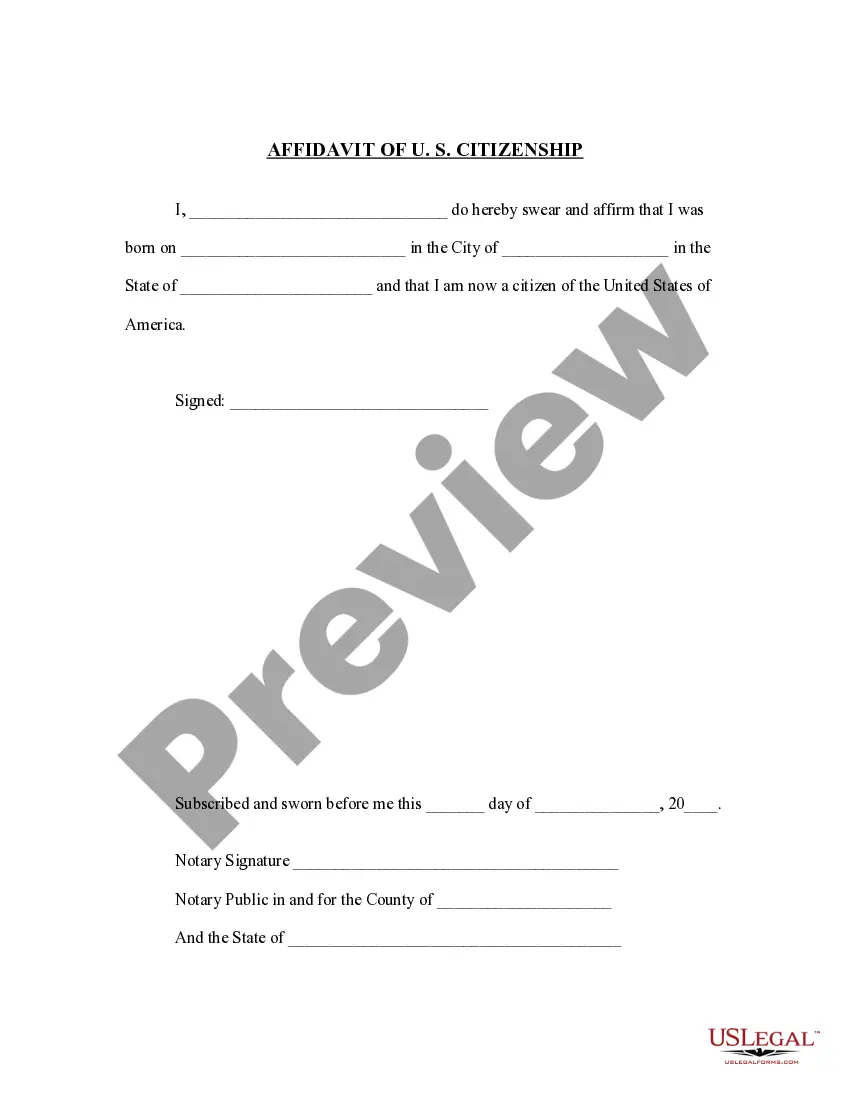
You can invest several hours on the Internet trying to find the legal file design that meets the state and federal needs you require. US Legal Forms offers a large number of legal kinds that are examined by professionals. You can easily down load or print the Vermont Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from the support.
If you have a US Legal Forms bank account, you can log in and click on the Down load key. Afterward, you can complete, revise, print, or signal the Vermont Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. Each legal file design you get is yours permanently. To obtain yet another duplicate for any obtained kind, go to the My Forms tab and click on the related key.
If you work with the US Legal Forms website the first time, keep to the straightforward recommendations listed below:
- Initially, make certain you have selected the proper file design to the area/city of your choice. Look at the kind description to ensure you have picked out the appropriate kind. If accessible, make use of the Preview key to look throughout the file design too.
- In order to find yet another edition in the kind, make use of the Look for industry to obtain the design that fits your needs and needs.
- After you have located the design you desire, simply click Purchase now to proceed.
- Pick the costs strategy you desire, type in your qualifications, and sign up for a merchant account on US Legal Forms.
- Complete the deal. You can utilize your credit card or PayPal bank account to cover the legal kind.
- Pick the formatting in the file and down load it in your gadget.
- Make changes in your file if needed. You can complete, revise and signal and print Vermont Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
Down load and print a large number of file themes using the US Legal Forms web site, which offers the most important variety of legal kinds. Use expert and condition-certain themes to tackle your business or person requires.
Form popularity
FAQ
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
If you are entitled to elect COBRA continuation coverage, you must be given an election period of at least 60 days (starting on the later of the date you are furnished the election notice or the date you would lose coverage) to choose whether or not to elect continuation coverage.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
Loss of Coverage Letter Letter from your previous health carrier indicating an involuntary loss of coverage. The supporting document must indicate your name, the names of any dependents that were covered under the prior plan and the date the previous health coverage ended.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.