Vermont Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
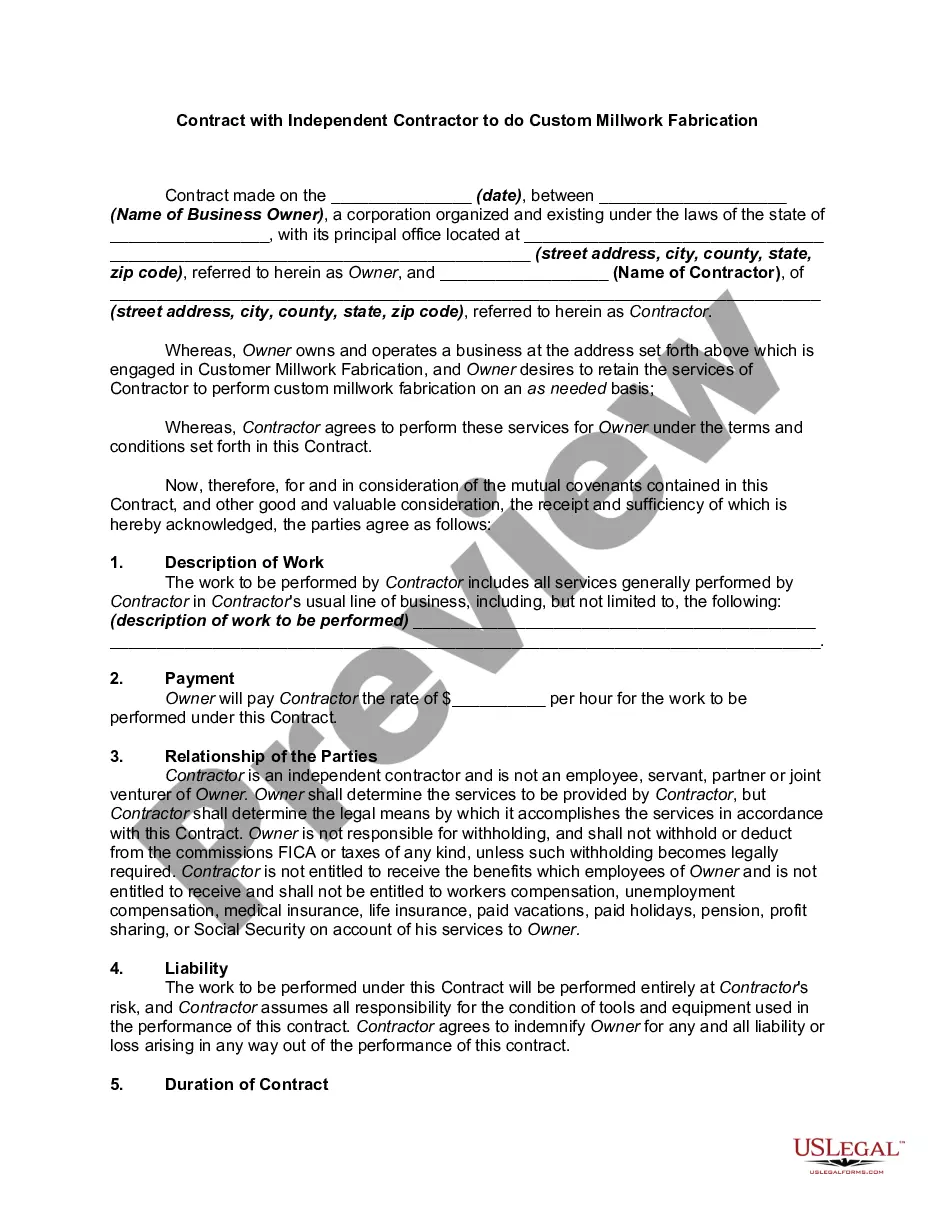
You can invest hours online searching for the legal document template that meets the state and federal requirements you need.
US Legal Forms offers thousands of legal documents that have been reviewed by experts.
You can conveniently access or print the Vermont Qualifying Event Notice Information for Employer to Plan Administrator from our platform.
First, ensure you have chosen the correct document template for your region/city that you select. Review the document description to confirm you have selected the right form. If available, utilize the Preview option to review the document template as well.
- If you already have a US Legal Forms account, you can Log In and select the Download option.
- Then, you can complete, modify, print, or sign the Vermont Qualifying Event Notice Information for Employer to Plan Administrator.
- All legal document templates you acquire are yours to keep indefinitely.
- To obtain another copy of any downloaded form, go to the My documents tab and select the appropriate option.
- If you're using the US Legal Forms website for the first time, follow the simple instructions provided below.
Form popularity
FAQ
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
From a legal standpoint, there is no federal law that says companies must offer health insurance to their employees. However, employers' health insurance requirements do apply for some businesses depending on their size.
Do I have to have health insurance? When Vermonters file their state taxes, they must report if they had health insurance (including Medicaid and Medicare) for each month of the year. There is no cash penalty for not having health insurance, but it is important that every Vermonter is covered.
Under the Consolidated Omnibus Budget Reconciliation Act (COBRA) , continuation of health coverage starts from the date the covered employee's health insurance ends and, depending on the type of qualifying event, may last for 18 months, 29 months or 36 months.
Apply for Health Insurance If you are uninsured, visit Vermont Health Connect or call 855-899-9600. Vermont Health Connect is the state's health insurance marketplace.
Coverage. Your employment with the State of Vermont is terminated. If you are entitled to choose continuation of coverage, you may remain in the State's group health plans for a period of 18 or 36 months depending on the qualifying event.
Medicaid provides free or low-cost health coverage to eligible needy persons.
Starting in 2017, Vermont employers that have more than four FTE employees (age 18 or older, working 30 or more hours) are required to offer health insurance coverage and employers are required to pay a portion of the cost. Employers that do not offer health insurance must pay the HCC on a quarterly basis.
Coverage. Your employment with the State of Vermont is terminated. If you are entitled to choose continuation of coverage, you may remain in the State's group health plans for a period of 18 or 36 months depending on the qualifying event.