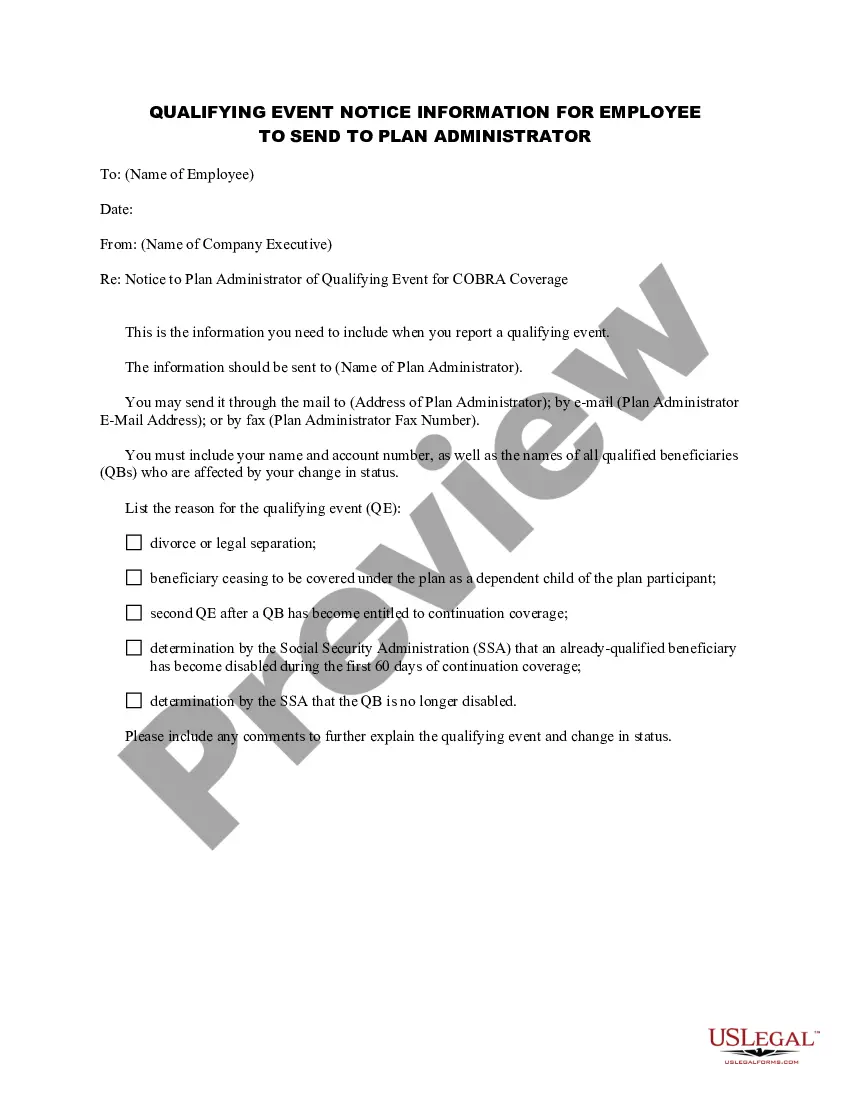
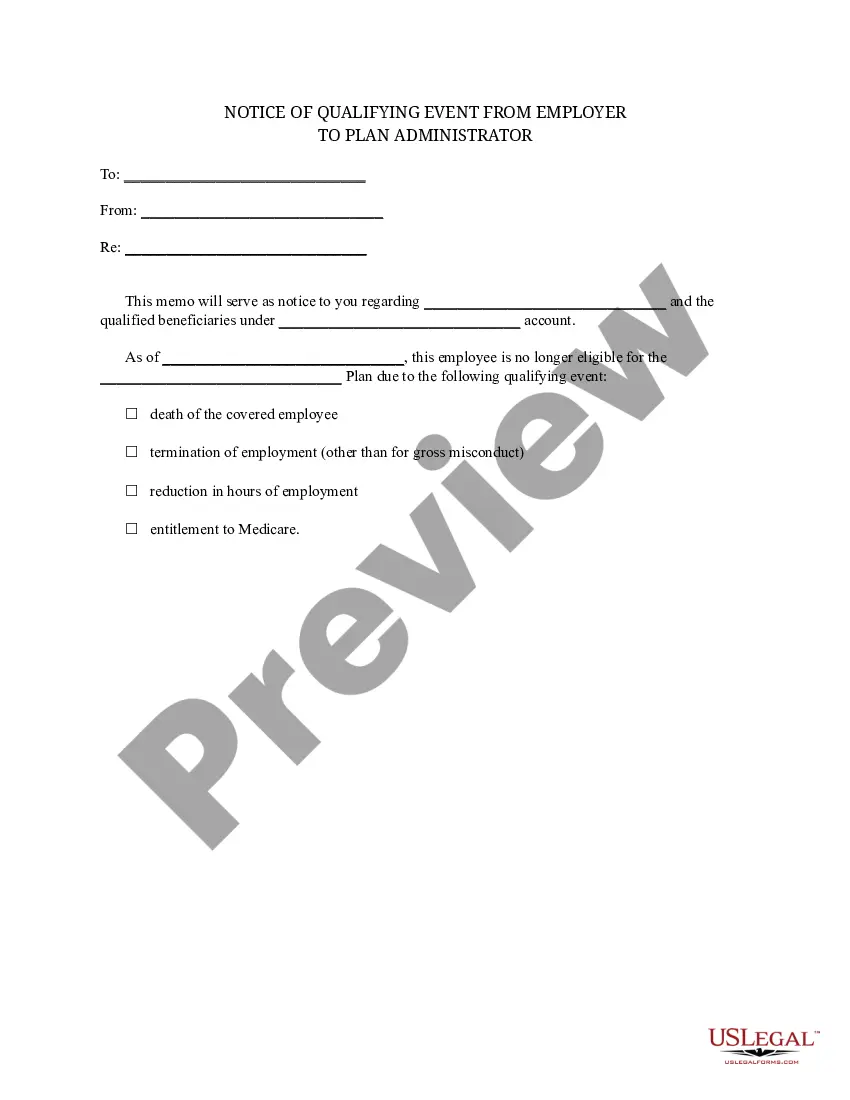
Vermont Notice of Qualifying Event from Employer to Plan Administrator
Description
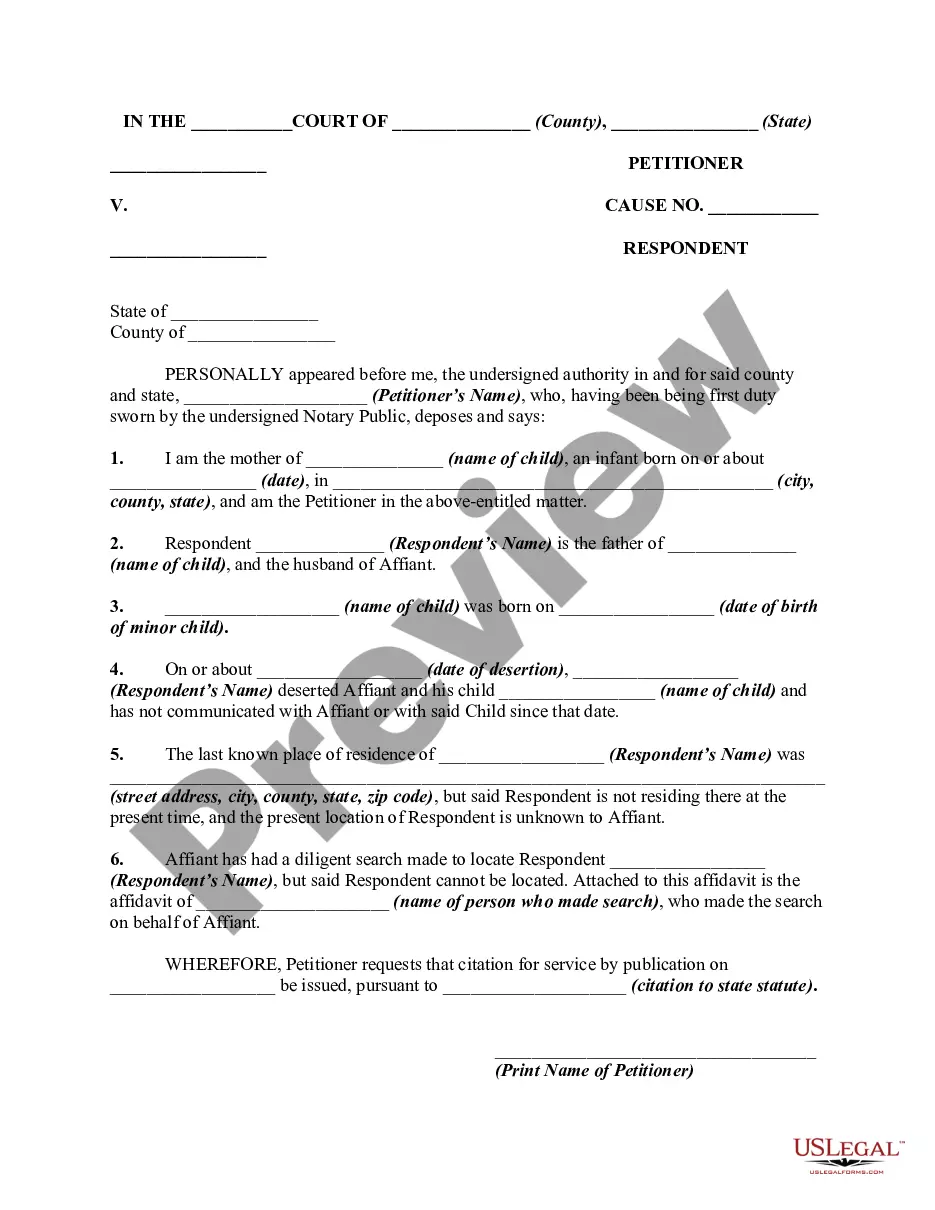
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
Selecting the ideal legal document template can be daunting. It goes without saying that there are numerous themes accessible online, but how can you locate the legal format you need? Use the US Legal Forms website.
The service provides thousands of templates, including the Vermont Notice of Qualifying Event from Employer to Plan Administrator, suitable for both business and personal needs. All forms are reviewed by professionals and comply with federal and state regulations.
If you're already a member, Log In to your account and click on the Obtain button to access the Vermont Notice of Qualifying Event from Employer to Plan Administrator. Use your account to search through the legal forms you have previously ordered. Visit the My documents section of your account to retrieve another copy of the document you need.
Complete, modify, print, and sign the obtained Vermont Notice of Qualifying Event from Employer to Plan Administrator. US Legal Forms is the largest library of legal forms where you can find a variety of document templates. Use the service to obtain professionally crafted documents that comply with state requirements.
- First, ensure you have chosen the correct form for your city/state.
- You can view the form using the Preview option and read the form description to confirm it is the appropriate one for you.
- If the form does not meet your requirements, utilize the Search field to locate the correct form.
- Once you are confident that the form is suitable, click on the Buy now button to purchase the form.
- Select the pricing plan you prefer and enter the necessary information. Create your account and complete the transaction using your PayPal account or credit card.
- Choose the document format and download the legal document template to your device.
Form popularity
FAQ
The income limit for Vermont Health Connect varies based on household size and other factors. Generally, the program provides assistance to those whose income falls within certain federal guidelines. If you want to understand how the Vermont Notice of Qualifying Event from Employer to Plan Administrator impacts your eligibility for programs like Vermont Health Connect, consulting a knowledgeable source can provide clarity.
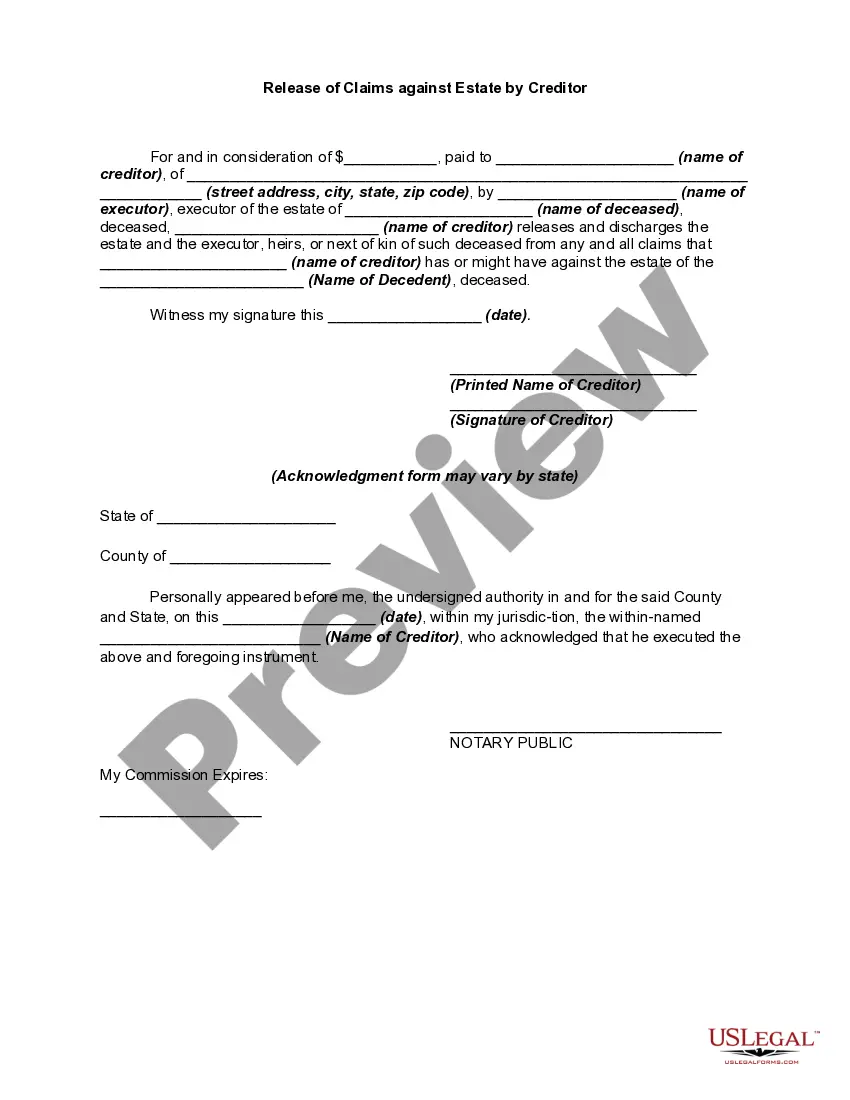
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Once a qualified beneficiary elects COBRA coverage, they have 45 calendar days from the date of election to pay all retroactive premiums to the plan or its designee. The retroactive premium payment is the premium to cover the period from the date of loss of coverage to the date of election.
Starting in 2017, Vermont employers that have more than four FTE employees (age 18 or older, working 30 or more hours) are required to offer health insurance coverage and employers are required to pay a portion of the cost. Employers that do not offer health insurance must pay the HCC on a quarterly basis.
Coverage. Your employment with the State of Vermont is terminated. If you are entitled to choose continuation of coverage, you may remain in the State's group health plans for a period of 18 or 36 months depending on the qualifying event.
The qualifying event for COBRA purposes is the employee's loss of employment date. However, the election period does not end until 60 days from the sent date of the election form to the employee or until 60 days after the loss of coverage, whichever is later.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
A plan, however, may provide longer periods of coverage beyond the maximum period required by law. When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA continuation coverage may be terminated if we don't receive timely payment of the premium. What is the grace period for monthly COBRA premiums? After election and initial payment, qualified beneficiaries have a 30-day grace period to make monthly payments (that is, 30 days from the due date).
Premium Payments Once a qualified beneficiary elects COBRA coverage, they have 45 calendar days from the date of election to pay all retroactive premiums to the plan or its designee. The retroactive premium payment is the premium to cover the period from the date of loss of coverage to the date of election.