Virginia Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
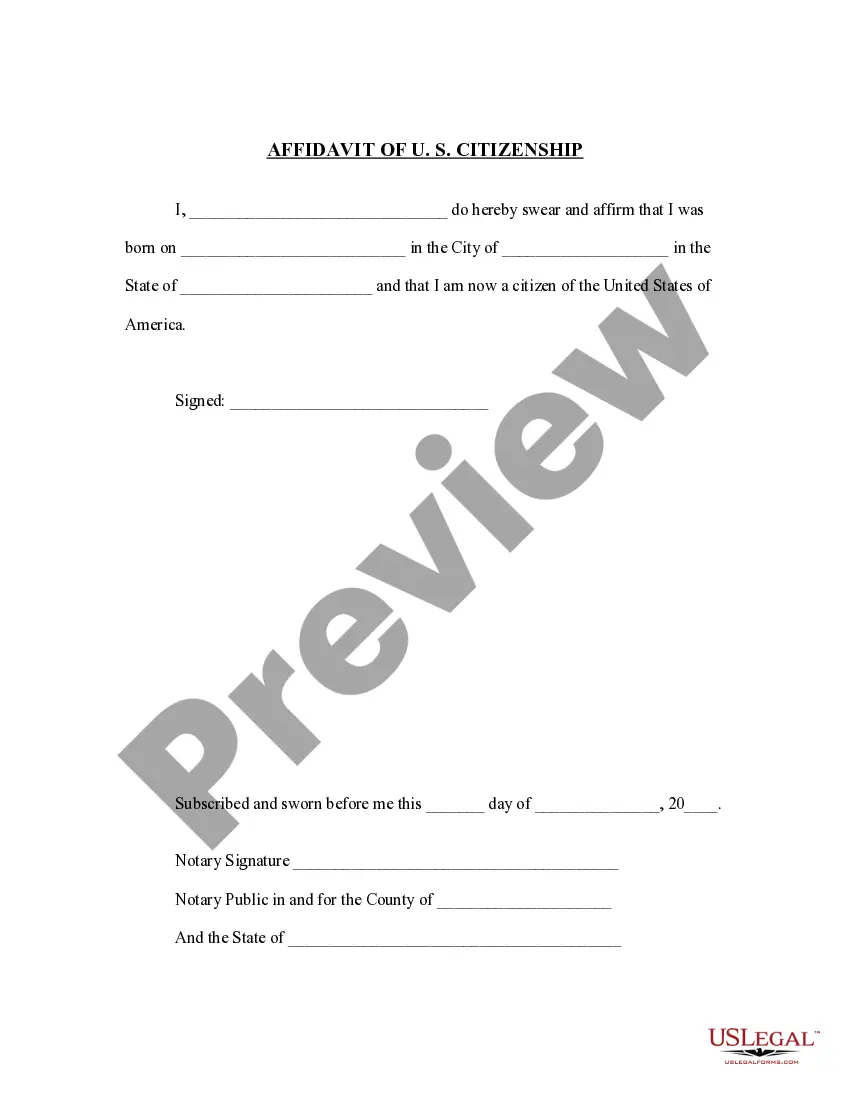
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
You can spend time online searching for the valid documents template that meets the state and federal requirements you will need.
US Legal Forms offers thousands of valid forms that are reviewed by experts.
It is easy to download or print the Virginia Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from our services.
To find another version of your form, use the Search field to locate the template that suits your needs.
- If you already possess a US Legal Forms account, you can Log In and click the Download button.
- After that, you may complete, modify, print, or sign the Virginia Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
- Every valid document template you obtain is yours permanently.
- To obtain another copy of any acquired form, visit the My documents tab and click the associated button.
- If you are using the US Legal Forms site for the first time, follow the simple instructions below.
- First, ensure you have selected the correct document template for the county/city of your choice.
- Review the form description to make sure you have chosen the right one.
Form popularity
FAQ
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
D.C., Maryland, and Virginia all have mini-COBRA laws that apply to employers with fewer than 20 employees. The D.C. mini-COBRA law provides for 3 months of continuation coverage, except in the case of terminations for gross misconduct.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
In most cases, COBRA provides for continuation of health plan coverage for up to 18 months following the work separation. COBRA rights accrue once a "qualifying event" occurs - basically, a qualifying event is any change in the employment relationship that results in loss of health plan benefits.
Step 5: Election Form and Payment If Cal-COBRA coverage is elected within 60 days of when the election notice was sent, the employer must allow 45 days from the date of election for the initial premiums owed to be paid.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
Did you know there is a continuation provision that applies to Virginia employers NOT subject to COBRA? It's called Virginia State Continuation coverage aka mini-cobra. Employers must notify individuals within 14 days of learning that a person covered under the health plan is no longer eligible for coverage.
Under Florida COBRA insurance, employees can continue their healthcare coverage for a minimum of 18 months, while their spouses and children may receive coverage for up to three years.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
D.C., Maryland, and Virginia all have mini-COBRA laws that apply to employers with fewer than 20 employees. The D.C. mini-COBRA law provides for 3 months of continuation coverage, except in the case of terminations for gross misconduct.