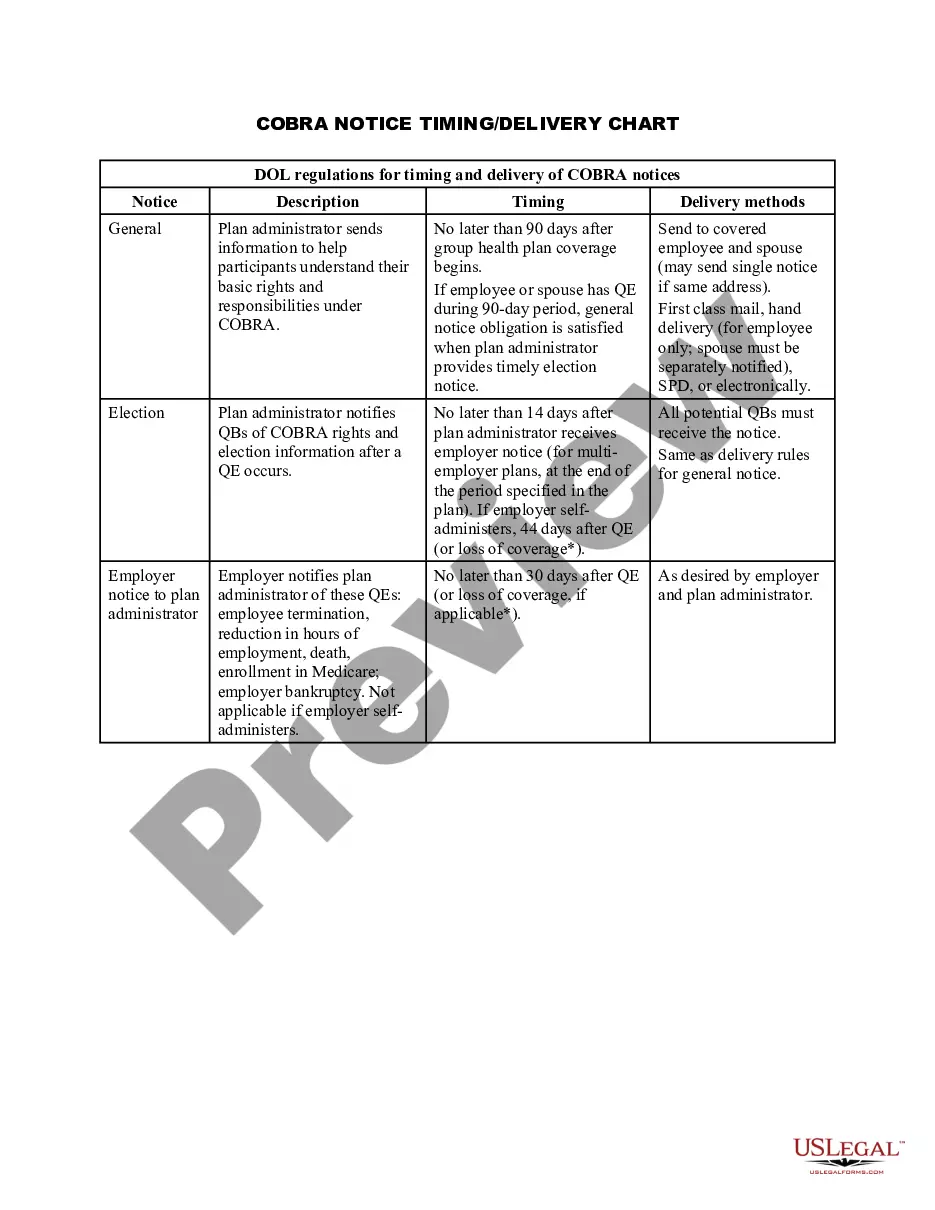
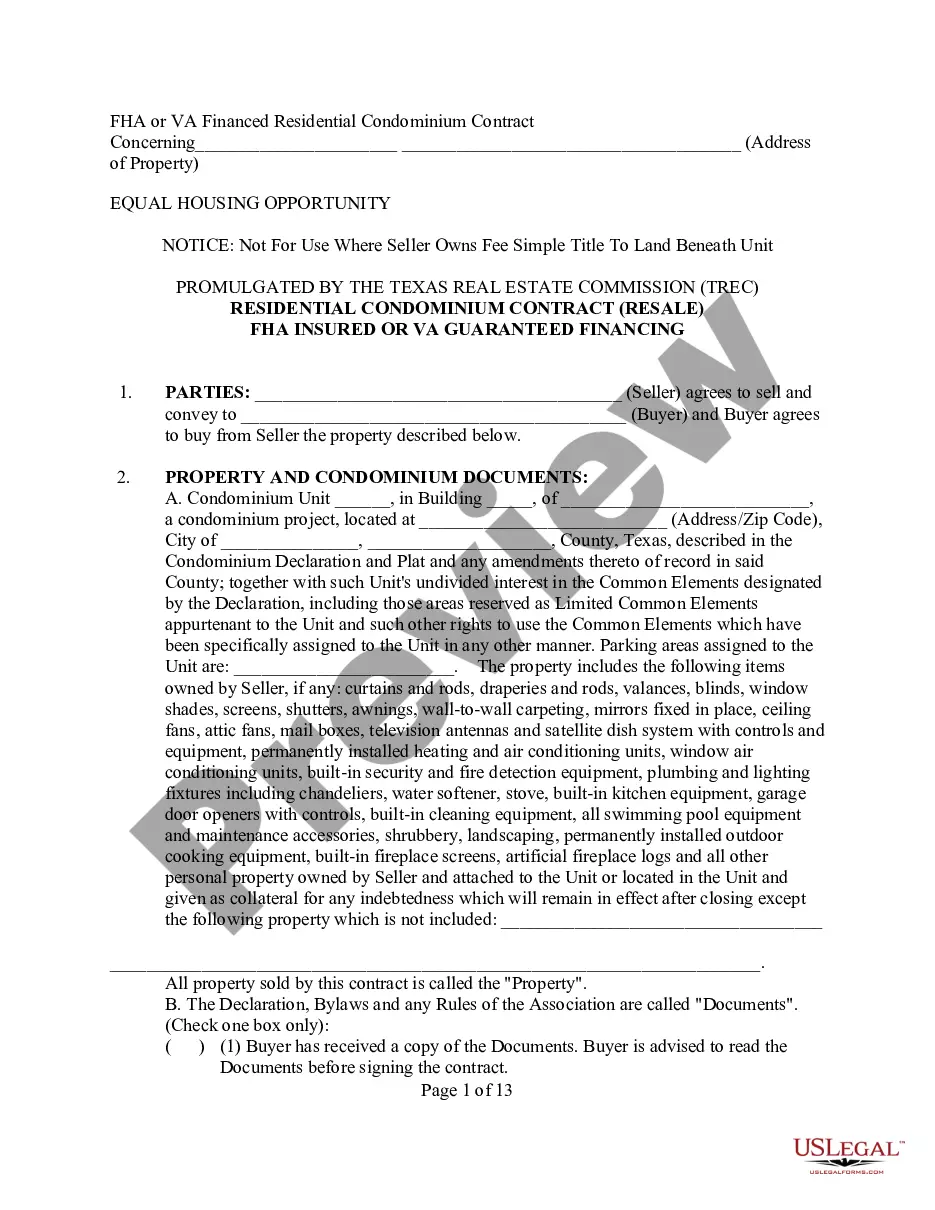
South Dakota COBRA Notice Timing Delivery Chart
Description
How to fill out COBRA Notice Timing Delivery Chart?
You can spend countless hours online searching for the legal document template that meets your federal and state requirements.
US Legal Forms offers a vast array of legal forms that are vetted by experts.
You can easily obtain or print the South Dakota COBRA Notice Timing Delivery Chart from the service.
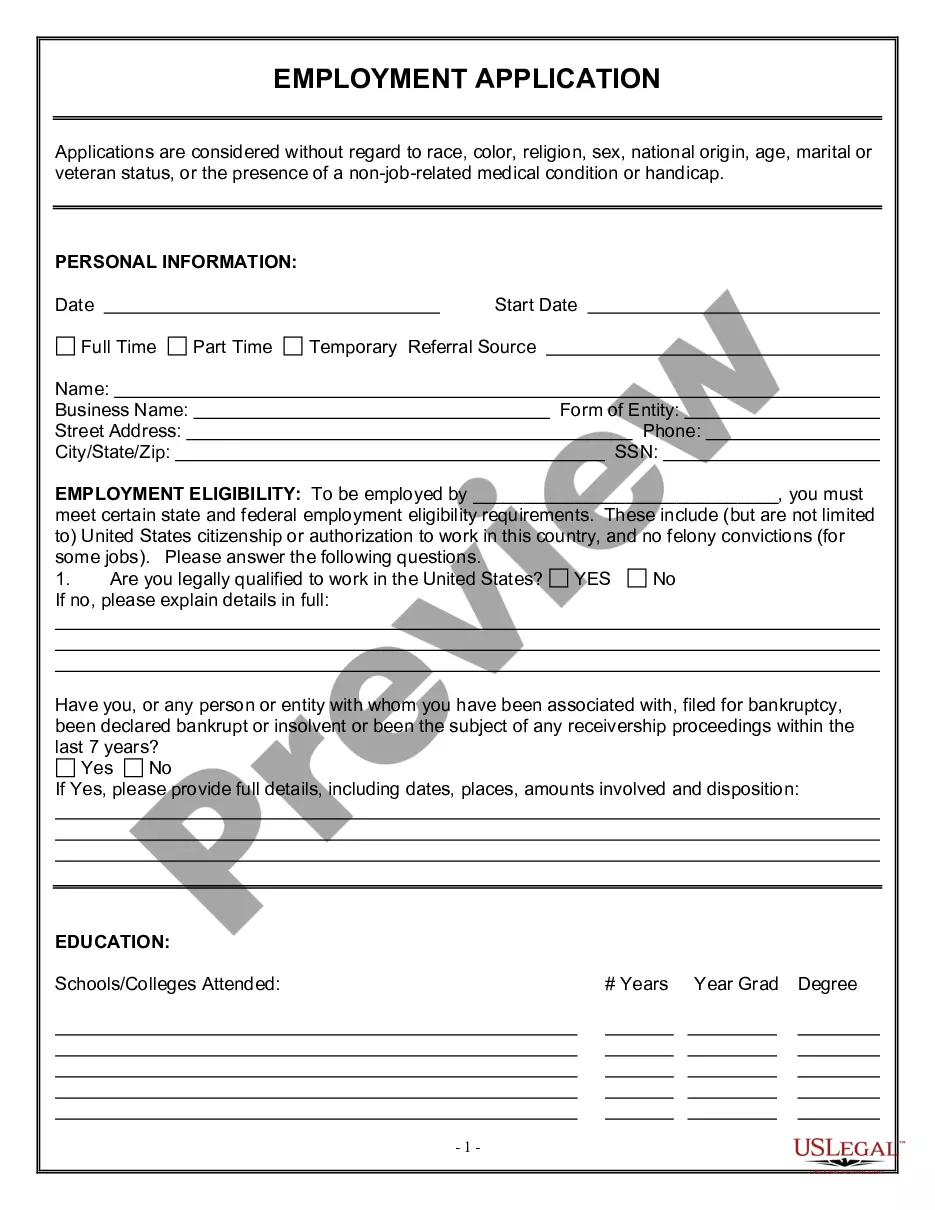
First, make sure you have selected the correct document template for the area/town you choose. Review the form details to ensure you have chosen the correct form. If available, use the Review button to look at the document template as well.
- If you already possess a US Legal Forms account, you can Log In and then click the Download button.
- Next, you can complete, modify, print, or sign the South Dakota COBRA Notice Timing Delivery Chart.
- Each legal document template you acquire is yours indefinitely.
- To obtain an additional copy of any purchased form, visit the My documents tab and click the appropriate button.
- If you are using the US Legal Forms website for the first time, follow these easy steps.
Form popularity
FAQ
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
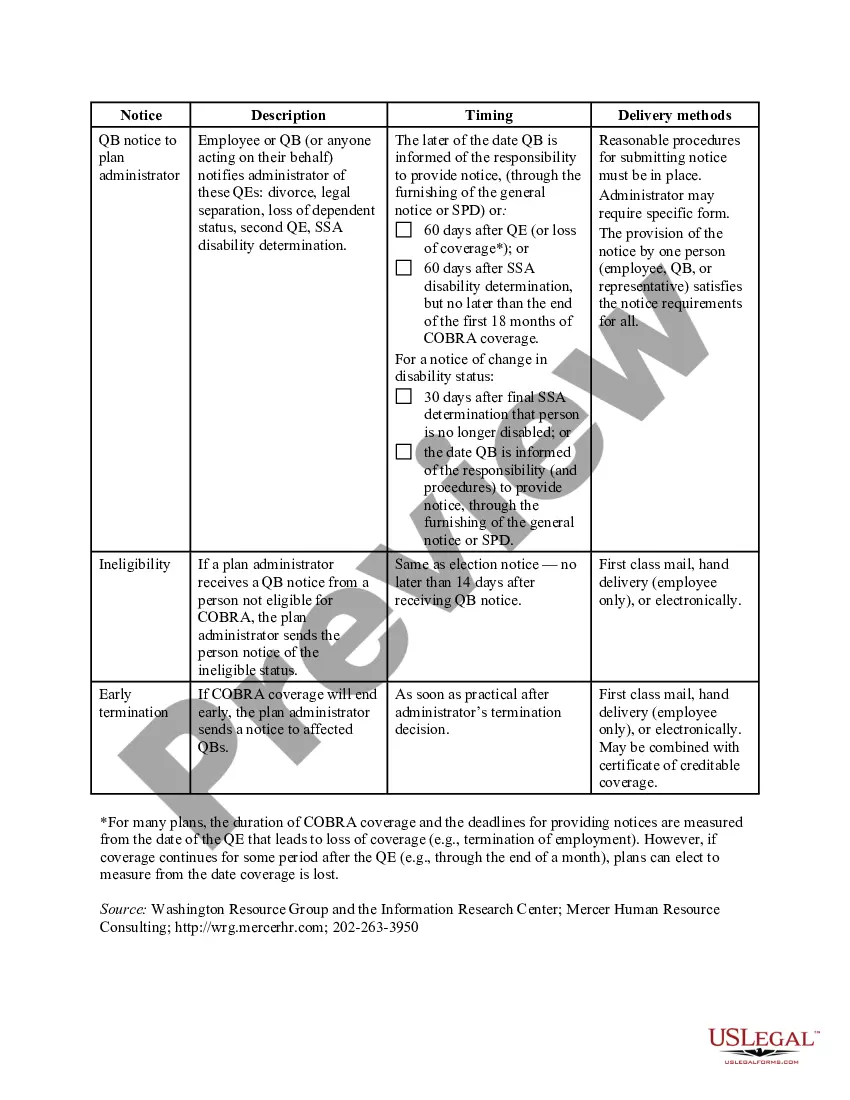
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
COBRA allows a 30-day grace period. If your premium payment is not received within the 30-day grace period, your coverage will automatically be terminated without advance warning. You will receive a termination letter at that time to notify you of a lapse in your coverage due to non-payment of premiums.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
COBRA is automatically available to you if you stop working at a qualified employer that provided group health insurance, but your participation in the program is not automatic. You must complete an enrollment form within the specified period of time and pay your first insurance premium.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.