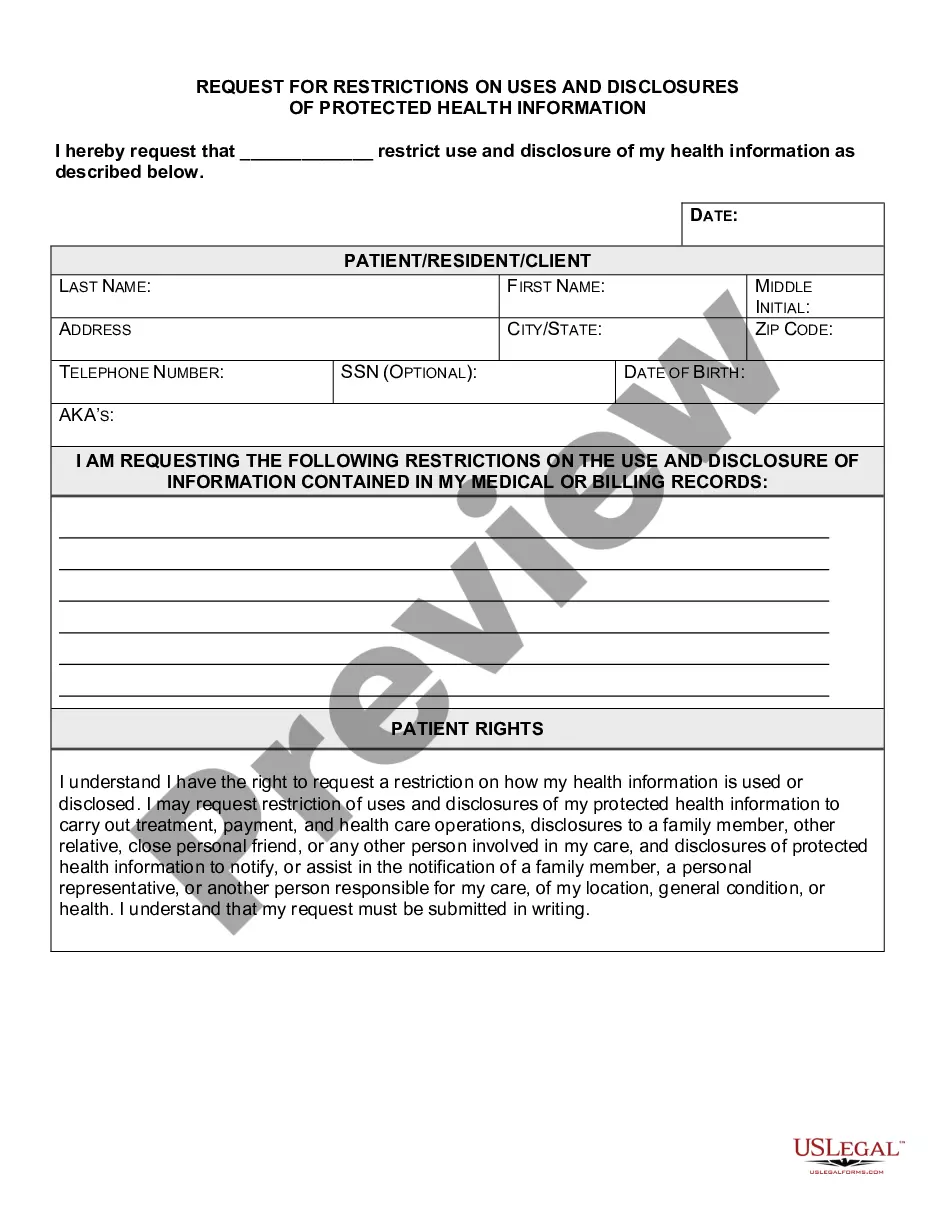
South Carolina Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
US Legal Forms - one of the most prominent collections of legal documents in America - offers a variety of legal form templates that you can download or print.
Through the website, you can access thousands of forms for business and personal purposes, organized by categories, states, or keywords. You can find the most recent versions of forms like the South Carolina Request for Restrictions on Uses and Disclosures of Protected Health Information in moments.
If you already hold a registration, Log In and download the South Carolina Request for Restrictions on Uses and Disclosures of Protected Health Information from the US Legal Forms library. The Download button will appear on every form you view. You can access all previously downloaded forms in the My documents section of your account.
Complete the transaction. Use your credit card or PayPal account to finalize the purchase.
Select the format and download the form to your device. Edit it. Fill out, modify, print, and sign the downloaded South Carolina Request for Restrictions on Uses and Disclosures of Protected Health Information.
Each template you added to your account does not have an expiration date and is yours indefinitely. Therefore, if you want to download or print another copy, simply visit the My documents section and click on the form you need.
Gain access to the South Carolina Request for Restrictions on Uses and Disclosures of Protected Health Information with US Legal Forms, the most extensive library of legal document templates. Utilize thousands of professional and state-specific templates that fulfill your business or personal requirements.
- Ensure you have selected the appropriate form for your city/region.
- Click the Preview button to review the contents of the form.
- Examine the form summary to confirm that you have chosen the correct form.
- If the form does not satisfy your needs, use the Search box at the top of the screen to find one that does.
- If you are satisfied with the form, confirm your choice by clicking the Get now button.
- Then, select your preferred payment plan and provide your details to register for an account.
Form popularity
FAQ
When dealing with de-identified health information, the South Carolina Request for Restrictions on Uses and Disclosures of Protected Health Information does not apply. This type of information has been stripped of personal identifiers, which means it cannot be linked back to an individual. Therefore, there are typically no restrictions on its use or disclosure. However, it's still important to handle all health information with care and consult legal guidelines.
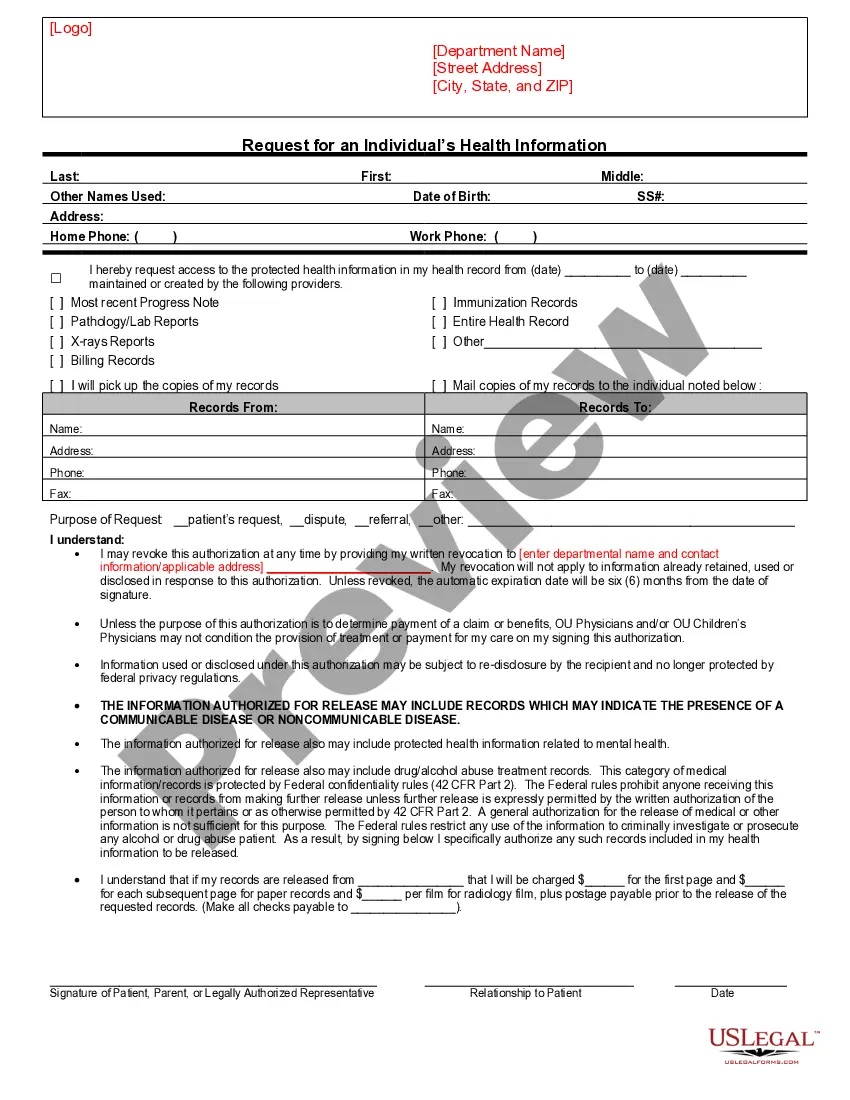
Valid HIPAA Authorizations: A ChecklistNo Compound Authorizations. The authorization may not be combined with any other document such as a consent for treatment.Core Elements.Required Statements.Marketing or Sale of PHI.Completed in Full.Written in Plain Language.Give the Patient a Copy.Retain the Authorization.
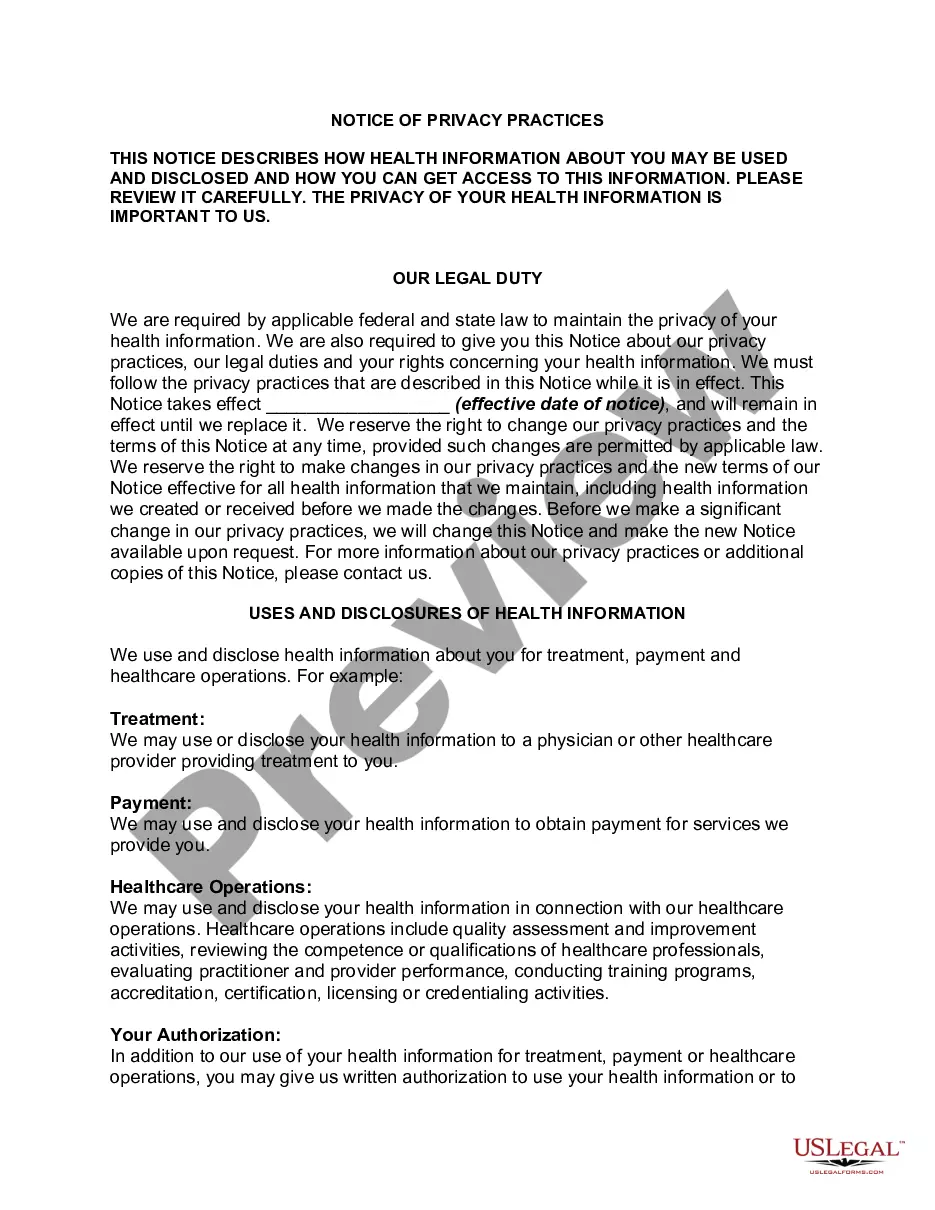
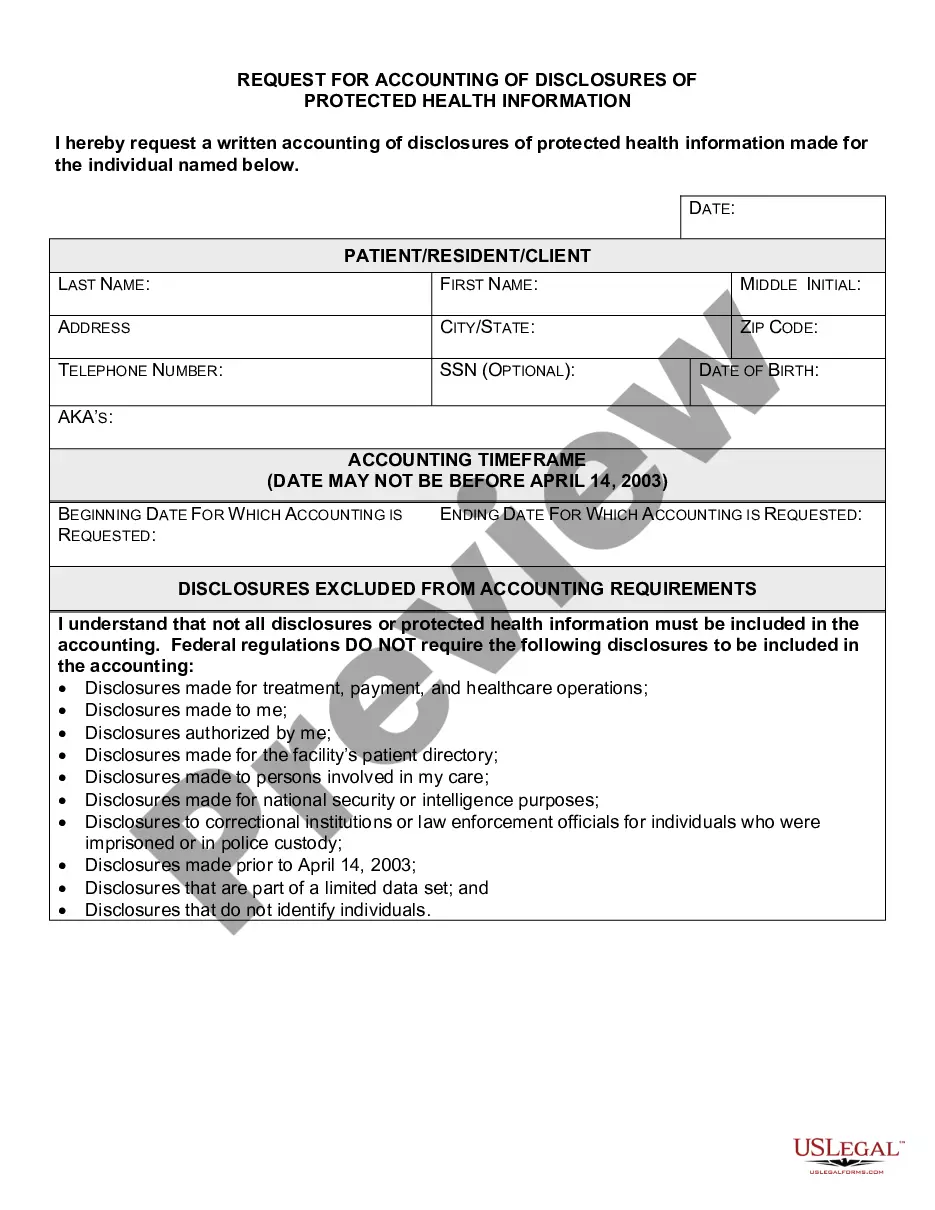
Since its initial adoption, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule has granted individuals the right to request restrictions regarding the use and disclosure of their protected health information (PHI) for treatment, payment, and healthcare operations (TPO).
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
HIPAA Exceptions DefinedTo public health authorities to prevent or control disease, disability or injury. To foreign government agencies upon direction of a public health authority. To individuals who may be at risk of disease. To family or others caring for an individual, including notifying the public.
Obtaining consent (written permission from individuals to use and disclose their protected health information for treatment, payment, and health care operations) is optional under the Privacy Rule for all covered entities.
Regardless of the method by which de-identification is achieved, the Privacy Rule does not restrict the use or disclosure of de-identified health information, as it is no longer considered protected health information, according to HHS.
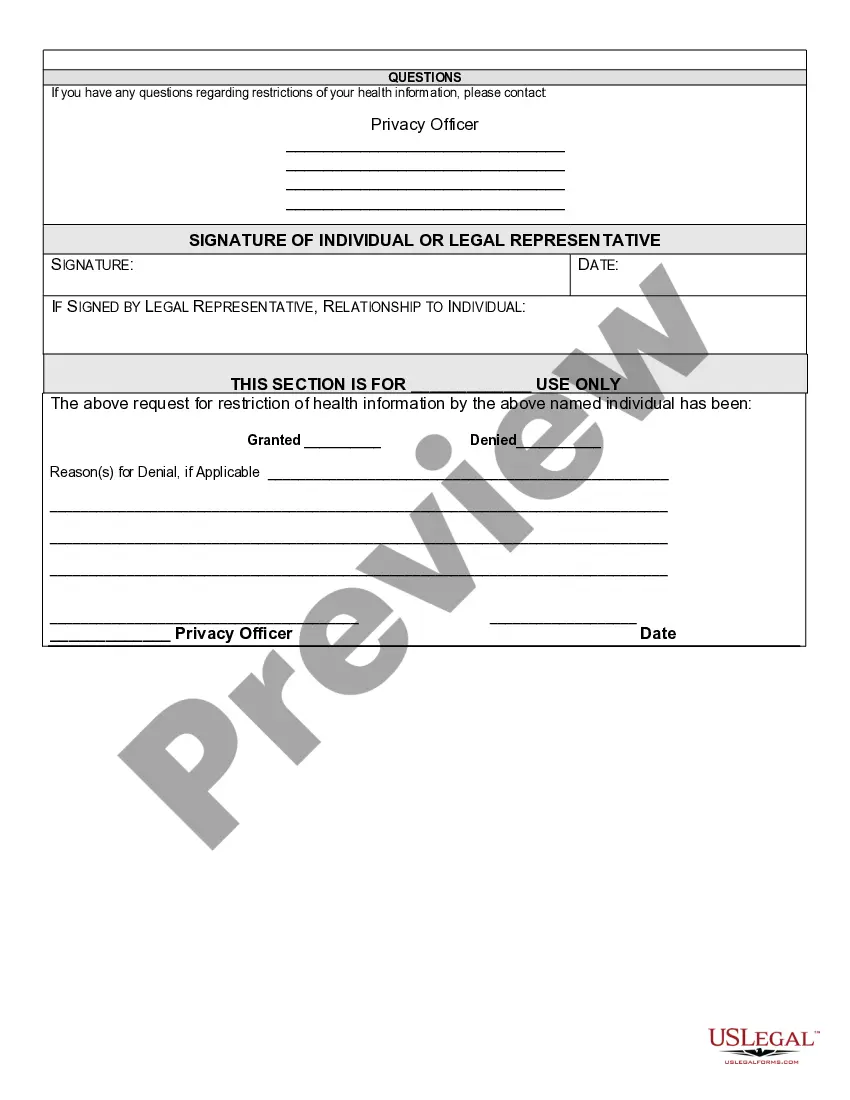
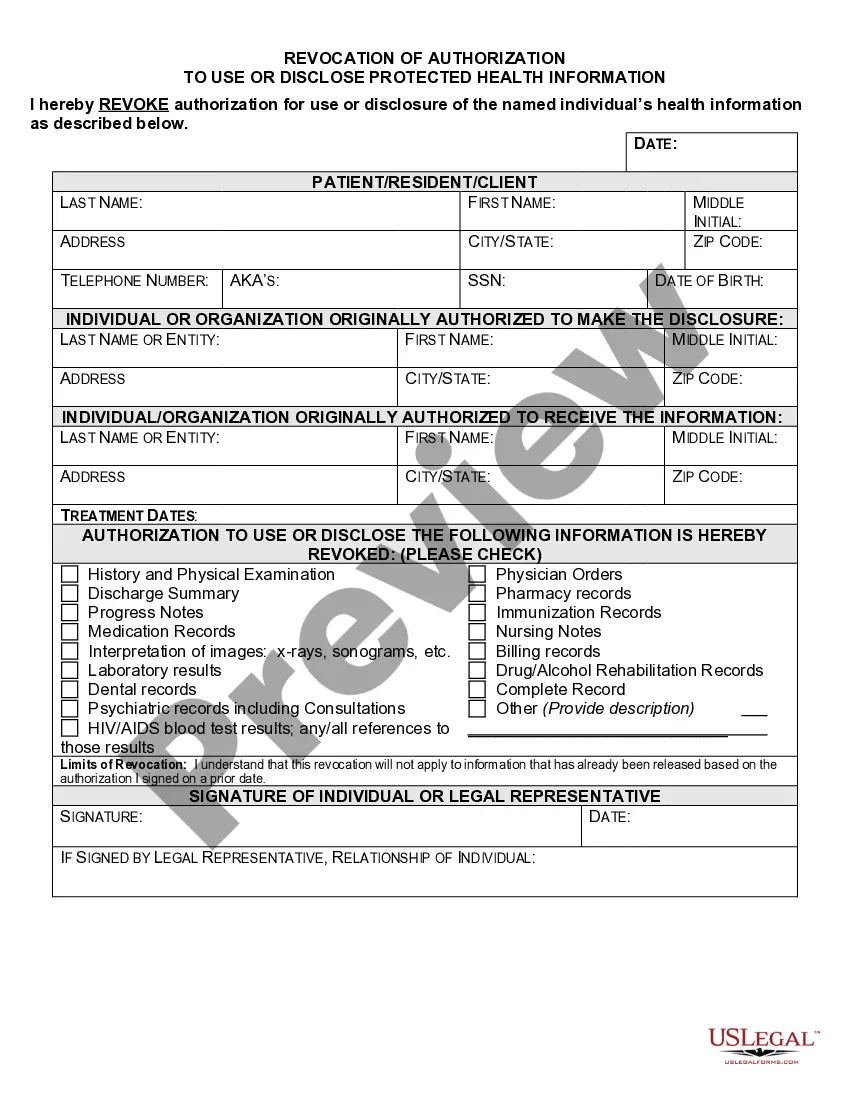
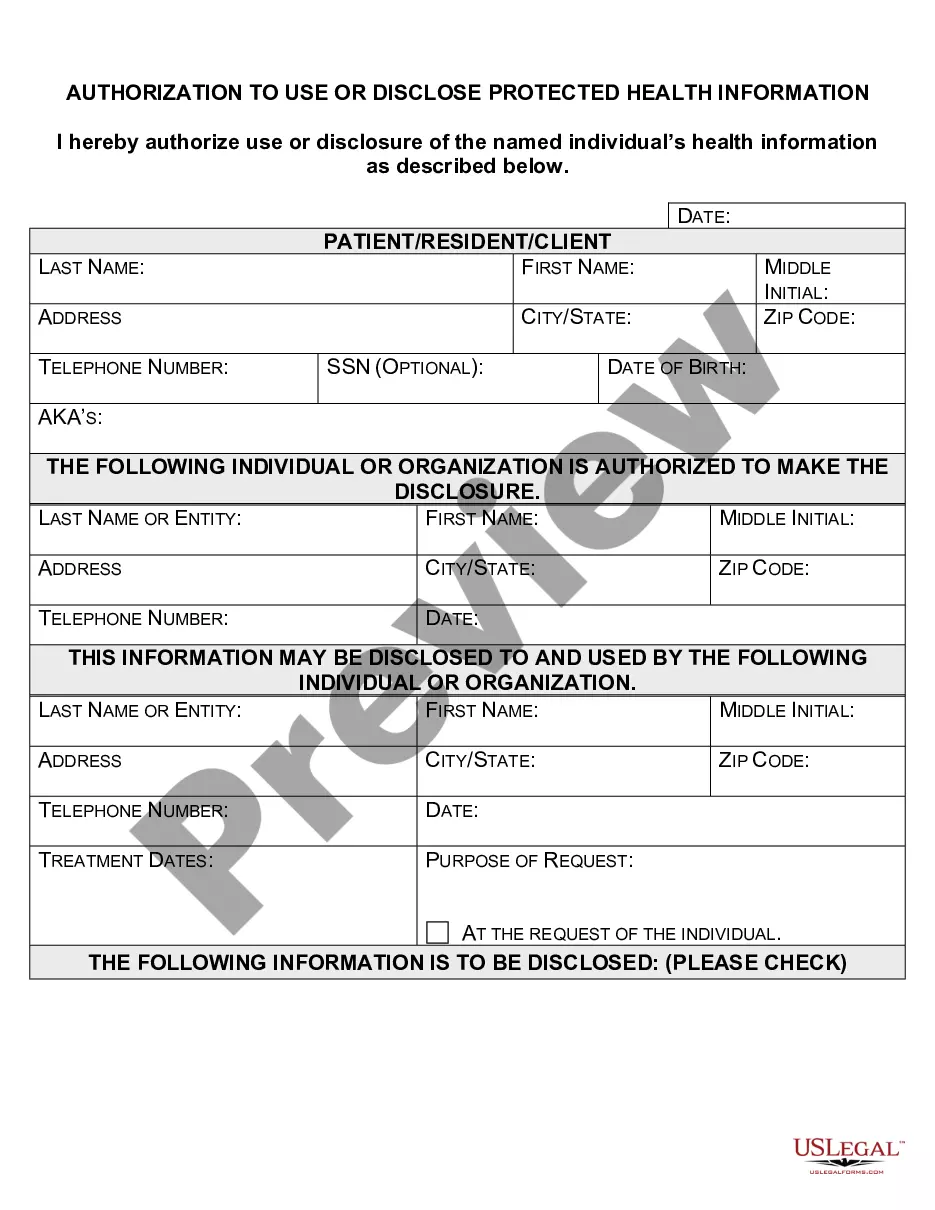
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
A patient authorization is not required for disclosure of PHI between Covered Entities if the disclosure is needed for purposes of treatment or payment or for healthcare operations. You may disclose the PHI as long as you receive a request in writing.
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.