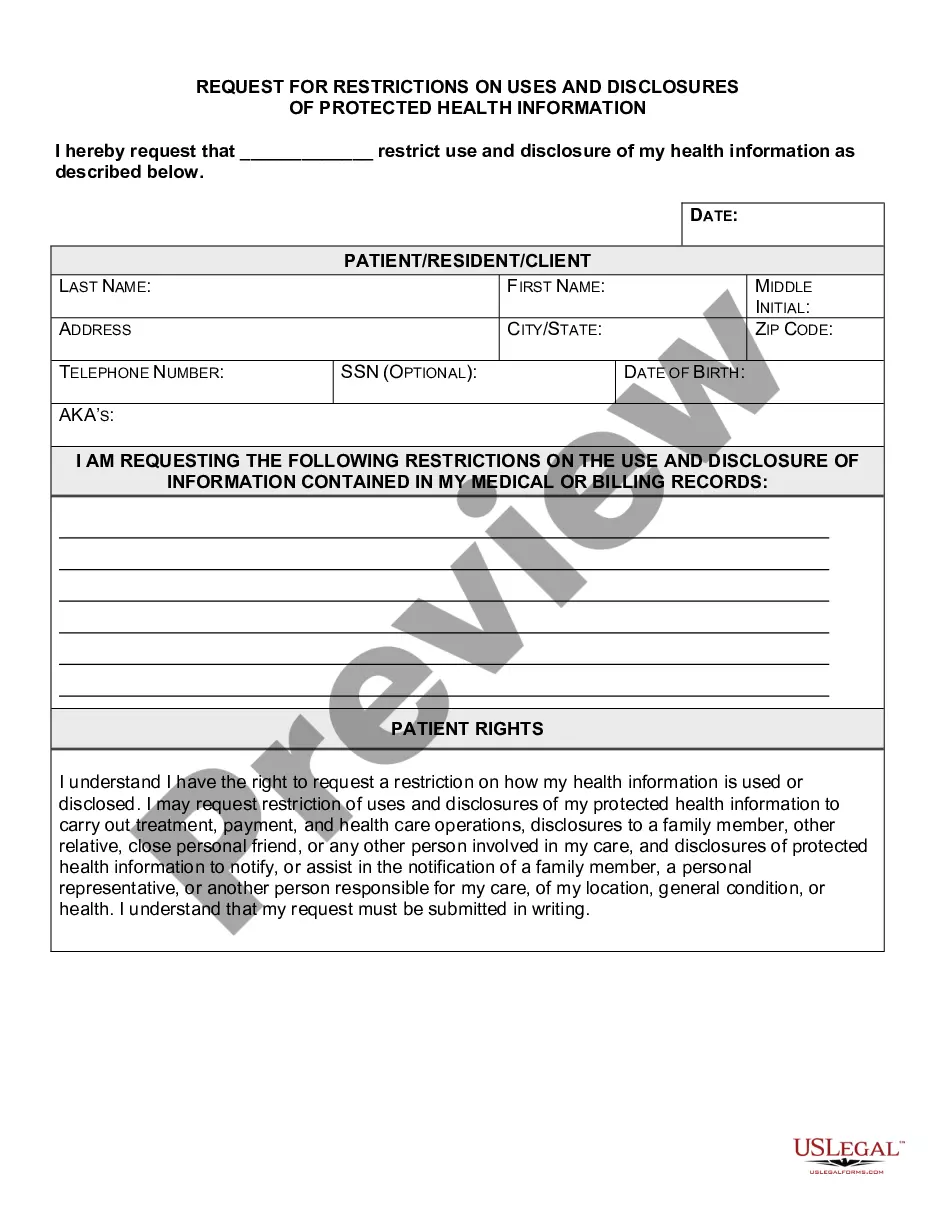
New York Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
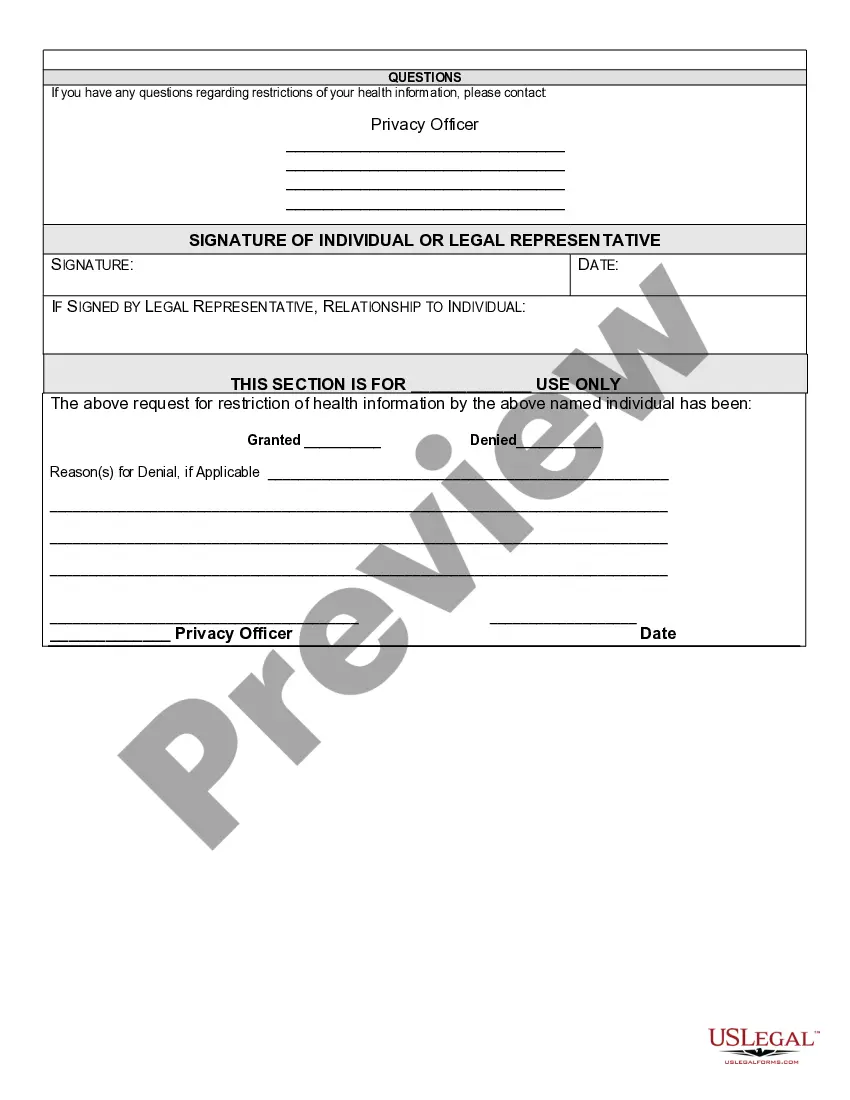
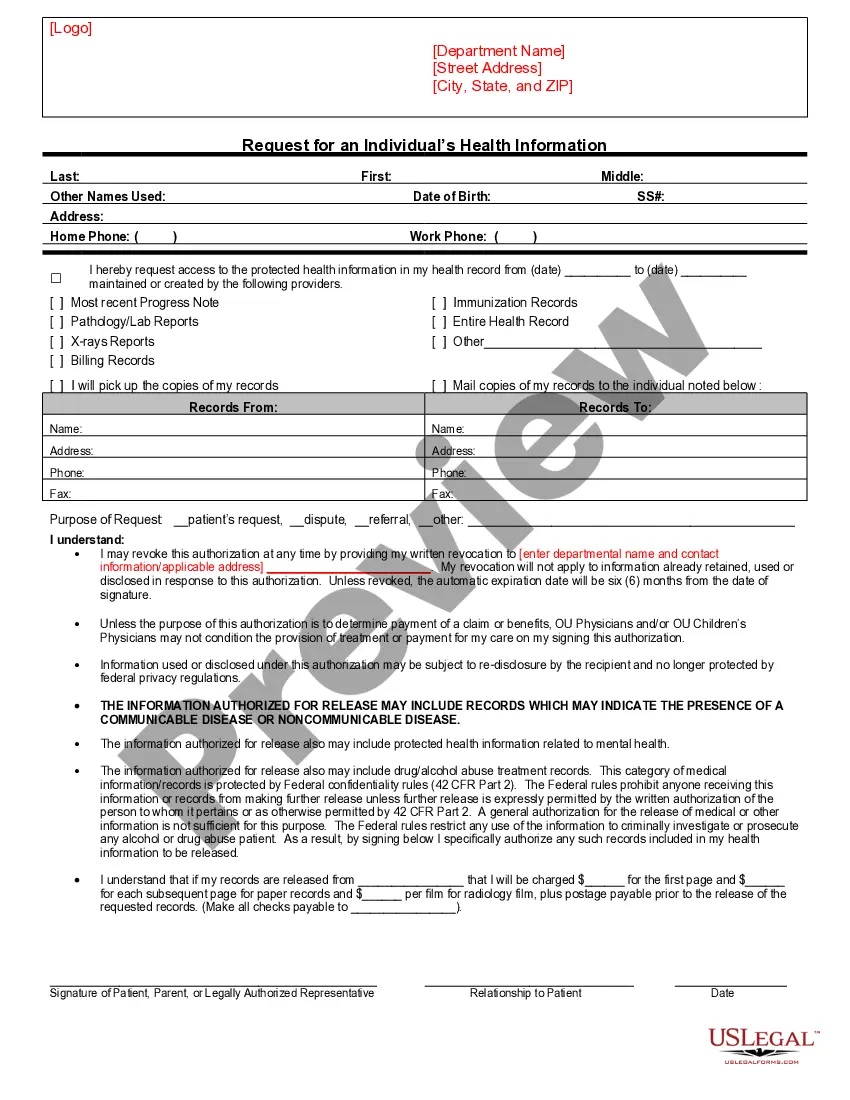
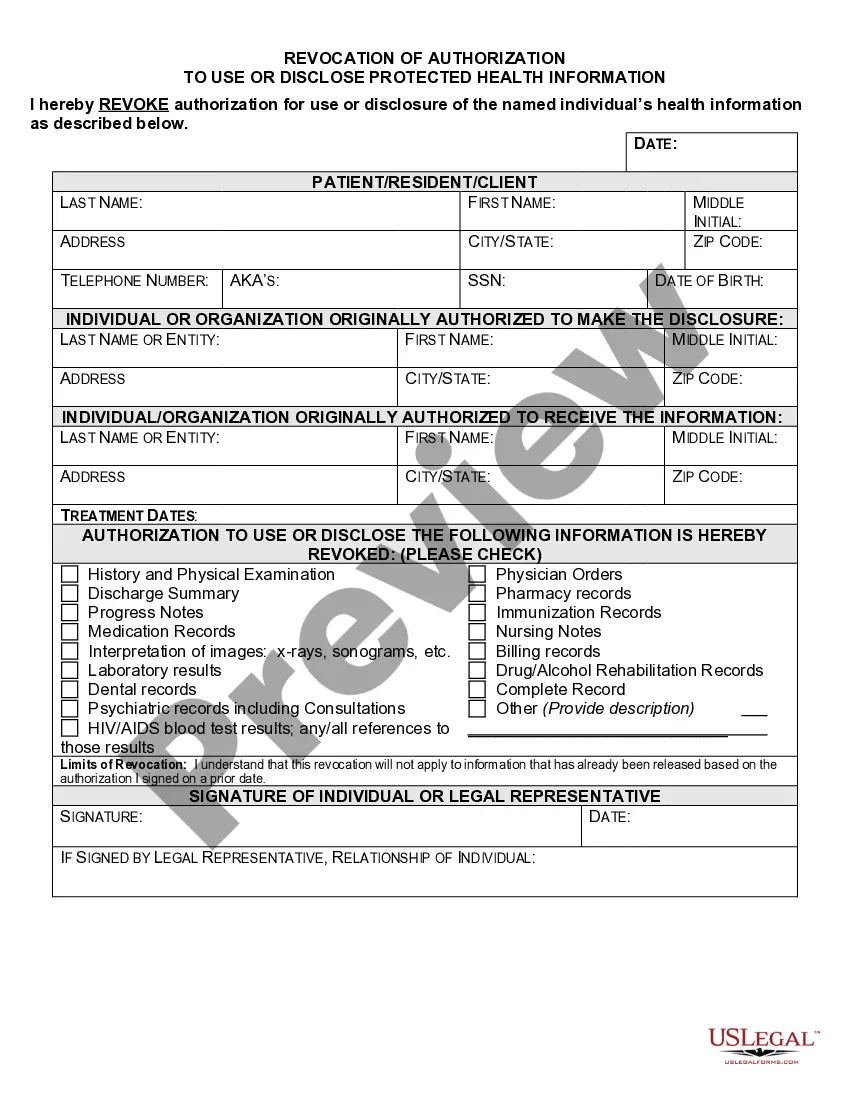
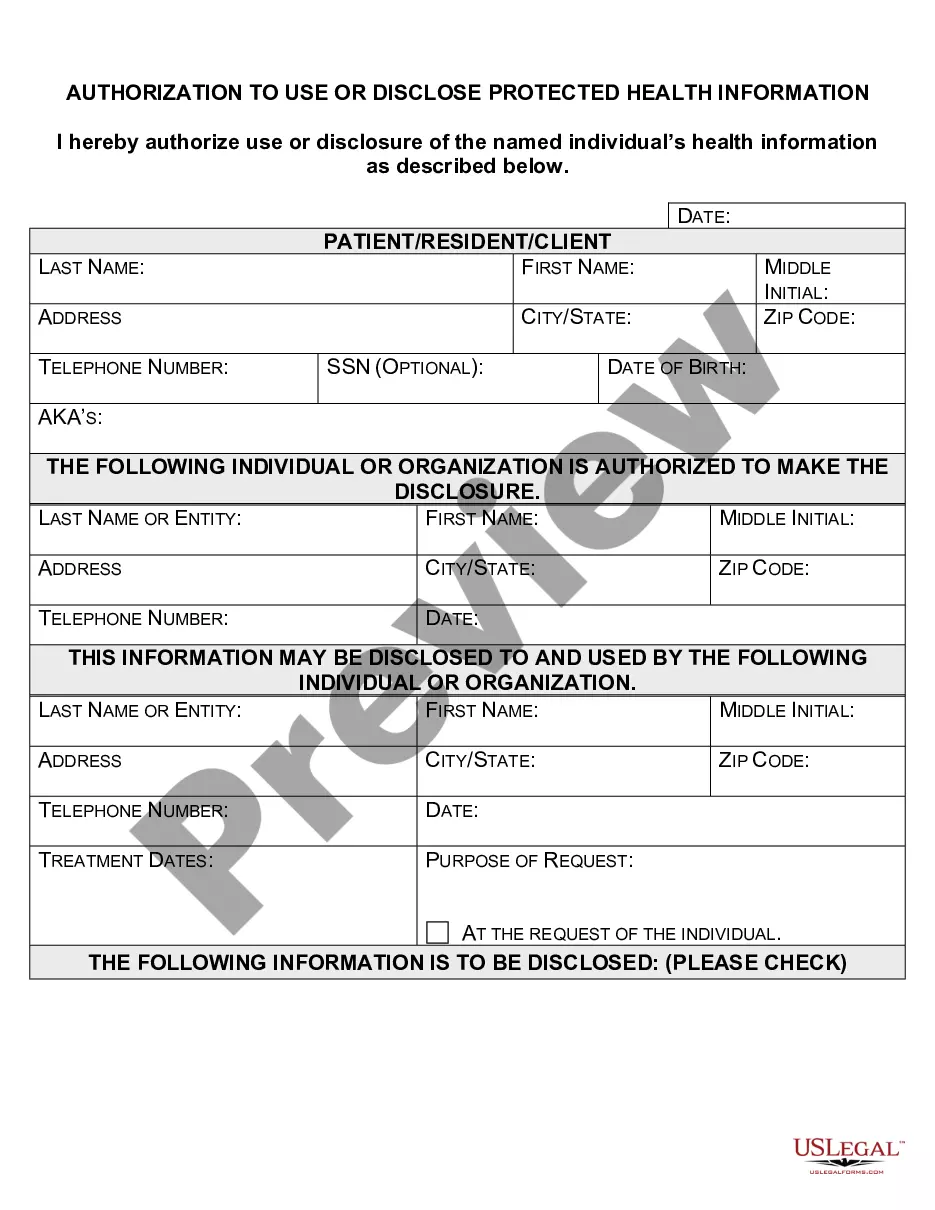
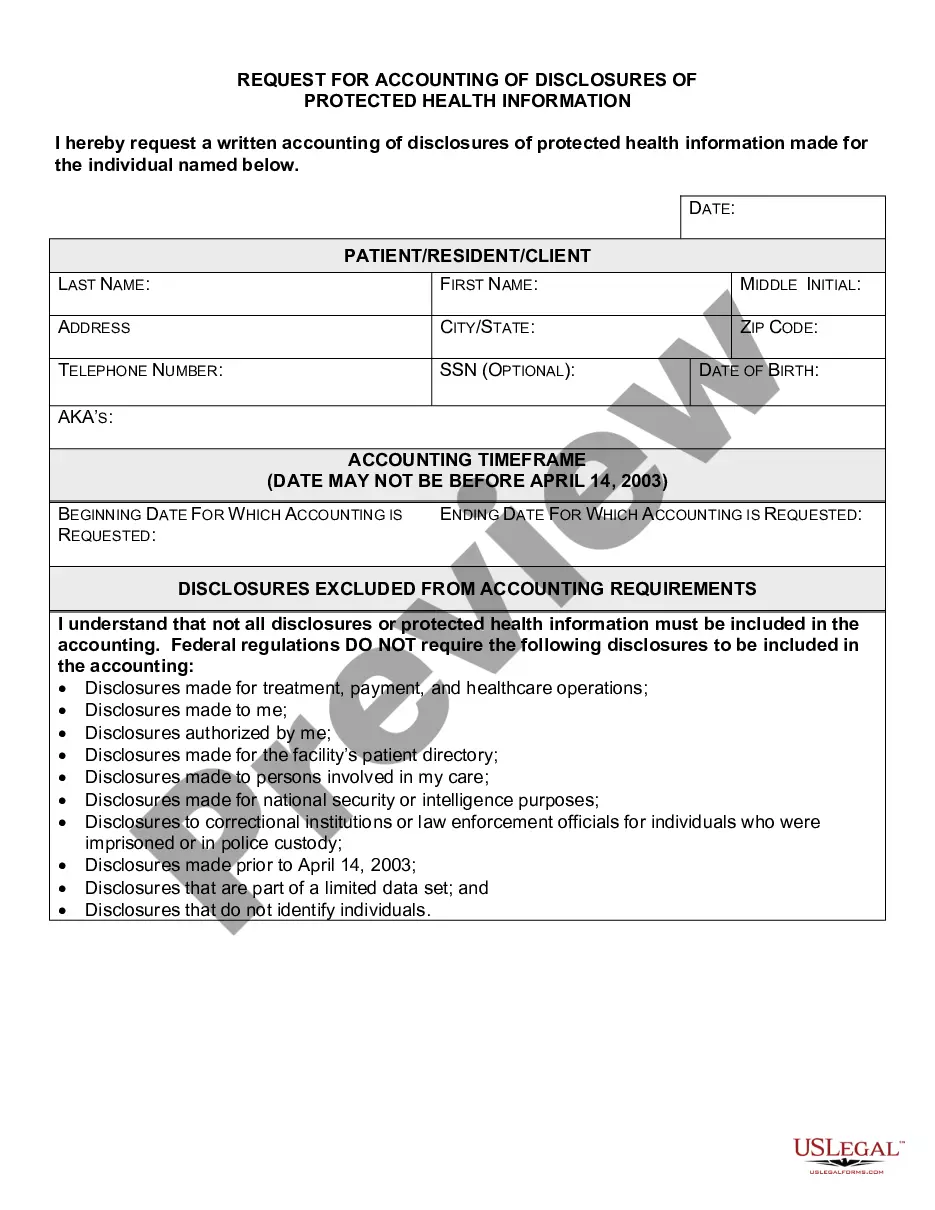
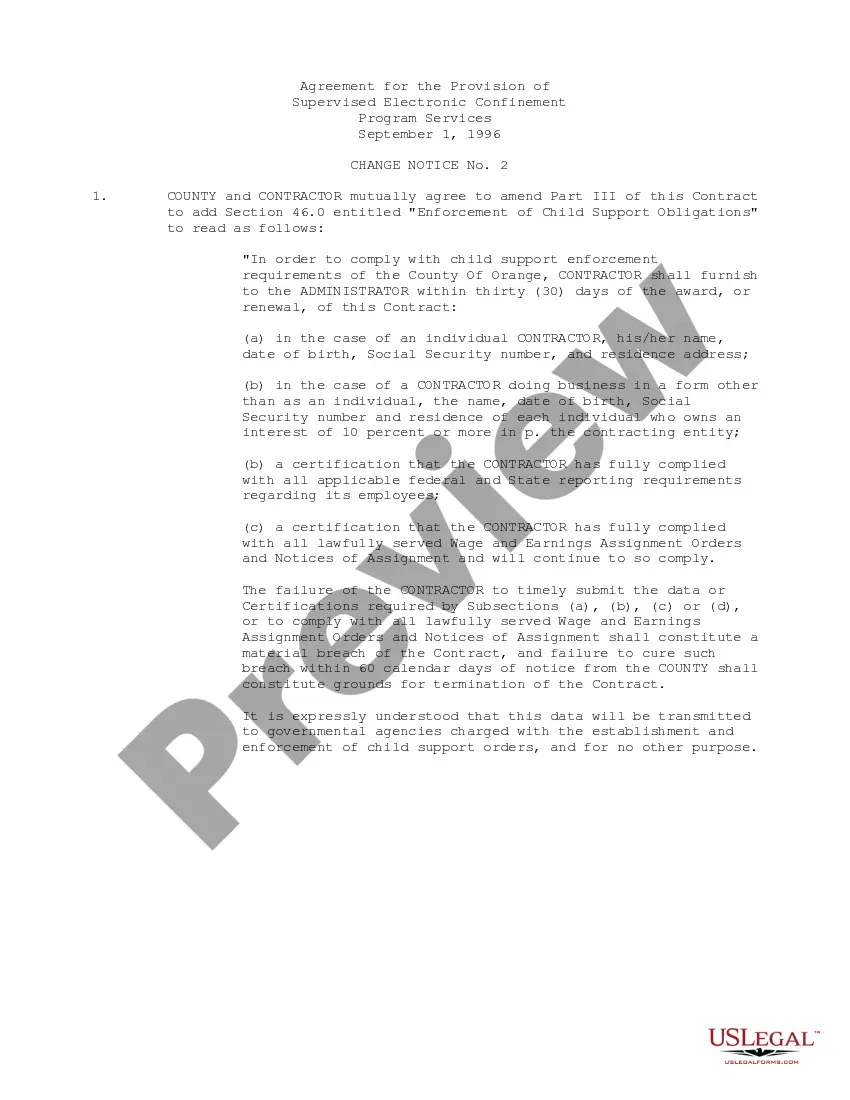
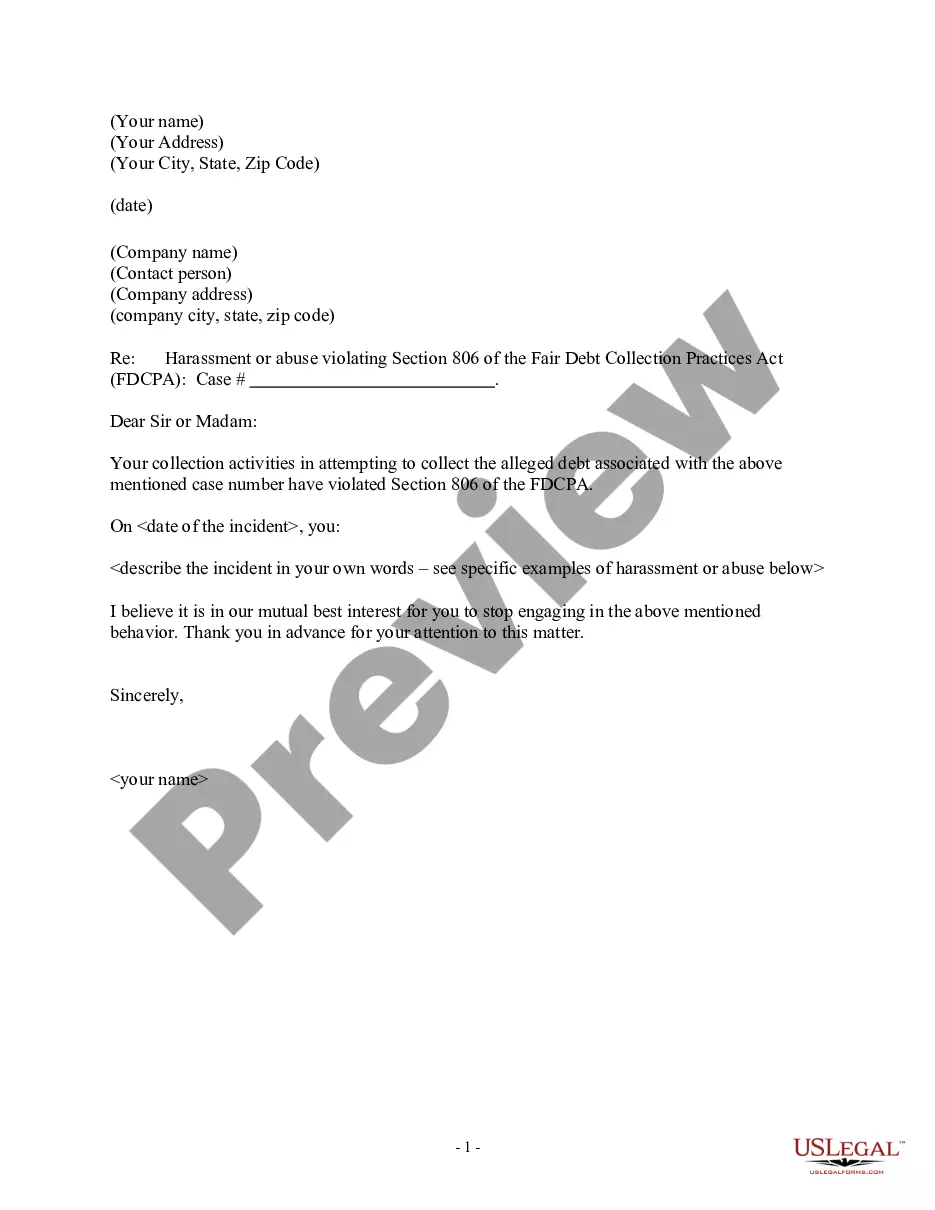
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
You might spend countless hours online searching for the proper legal document template that complies with the federal and state requirements you have.
US Legal Forms offers thousands of legal forms that are reviewed by professionals.
You can easily download or create the New York Request for Restrictions on Uses and Disclosures of Protected Health Information from their service.
To find another version of the form, use the Search field to locate the template that meets your needs.
- If you already have a US Legal Forms account, you can sign in and click the Download option.
- After that, you can complete, edit, print, or sign the New York Request for Restrictions on Uses and Disclosures of Protected Health Information.
- Every legal document template you purchase is yours for a lifetime.
- To obtain another copy of any purchased form, go to the My documents section and click the relevant option.
- If you are using the US Legal Forms website for the first time, follow the simple steps below.
- First, ensure you have selected the correct document template for the location of your choice.
- Review the form outline to make sure you have identified the right form.
Form popularity
FAQ
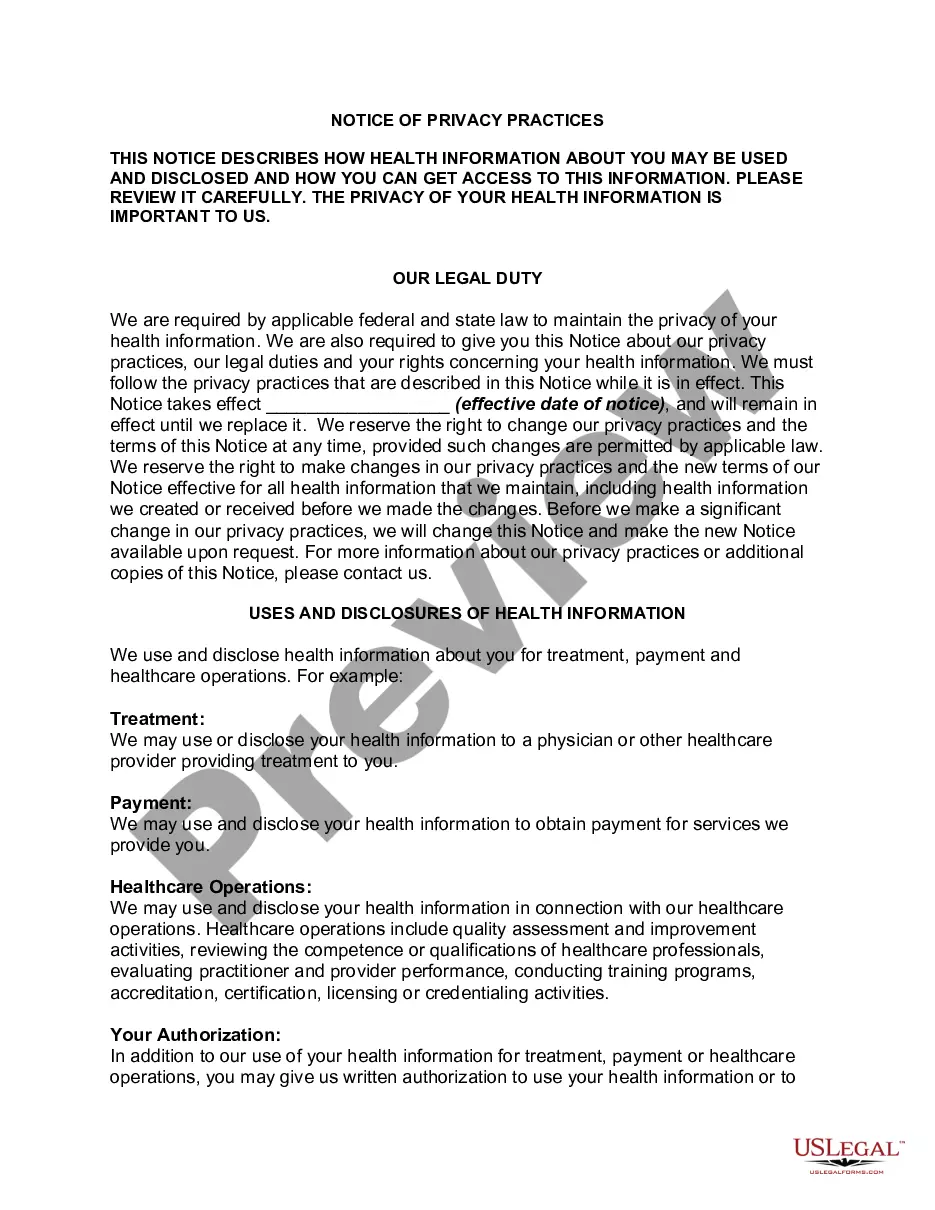
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
One fact sheet addresses Permitted Uses and Disclosures for Health Care Operations, and clarifies that an entity covered by HIPAA (covered entity), such as a physician or hospital, can disclose identifiable health information (referred to in HIPAA as protected health information or PHI) to another covered entity (or
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
HIPAA Exceptions DefinedTo public health authorities to prevent or control disease, disability or injury. To foreign government agencies upon direction of a public health authority. To individuals who may be at risk of disease. To family or others caring for an individual, including notifying the public.
Regardless of the method by which de-identification is achieved, the Privacy Rule does not restrict the use or disclosure of de-identified health information, as it is no longer considered protected health information, according to HHS.
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.
Covered entities may disclose protected health information to: Public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability. Public health or other government authorities authorized to receive reports of child abuse and neglect.
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item