New Mexico Individual Notice of Preexisting Condition Exclusion
Description
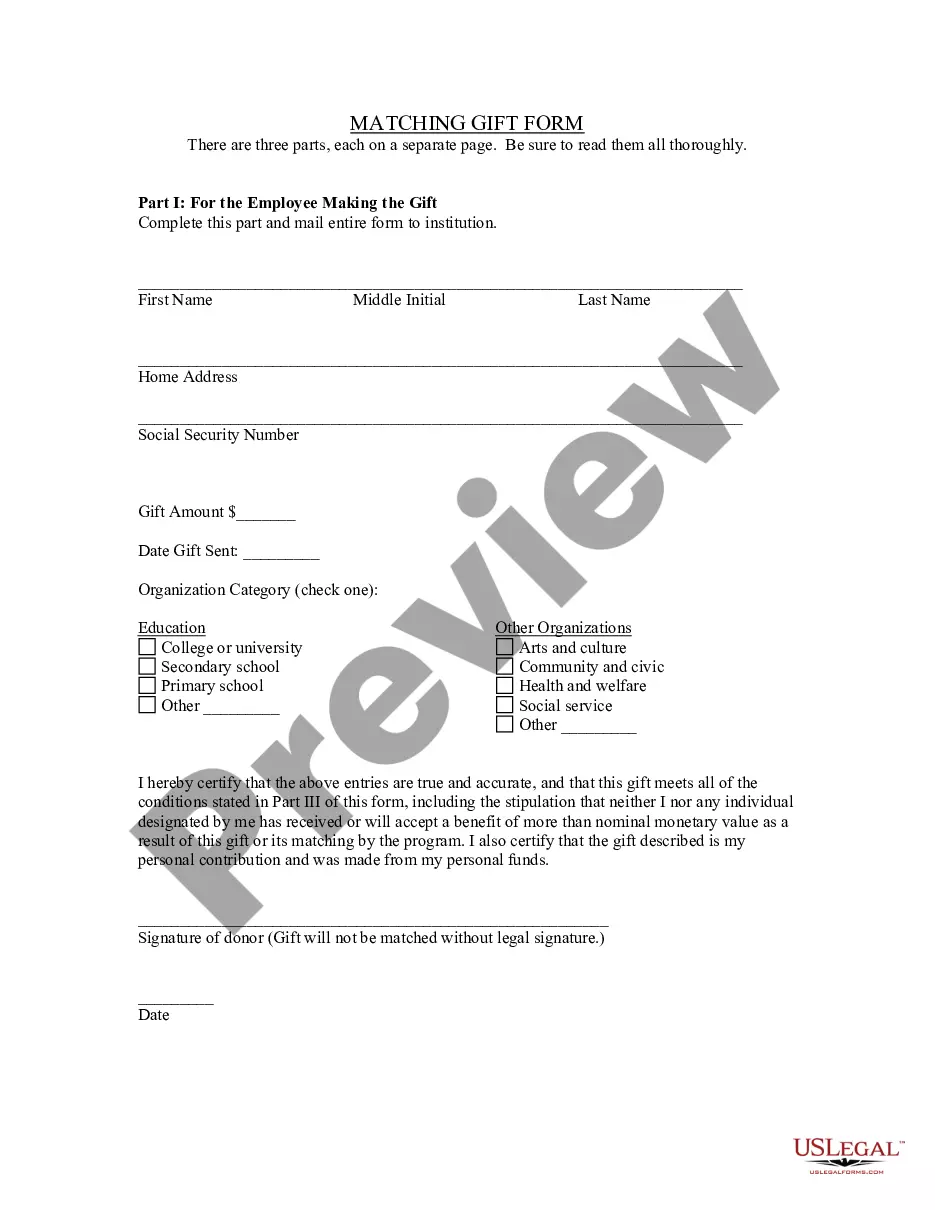
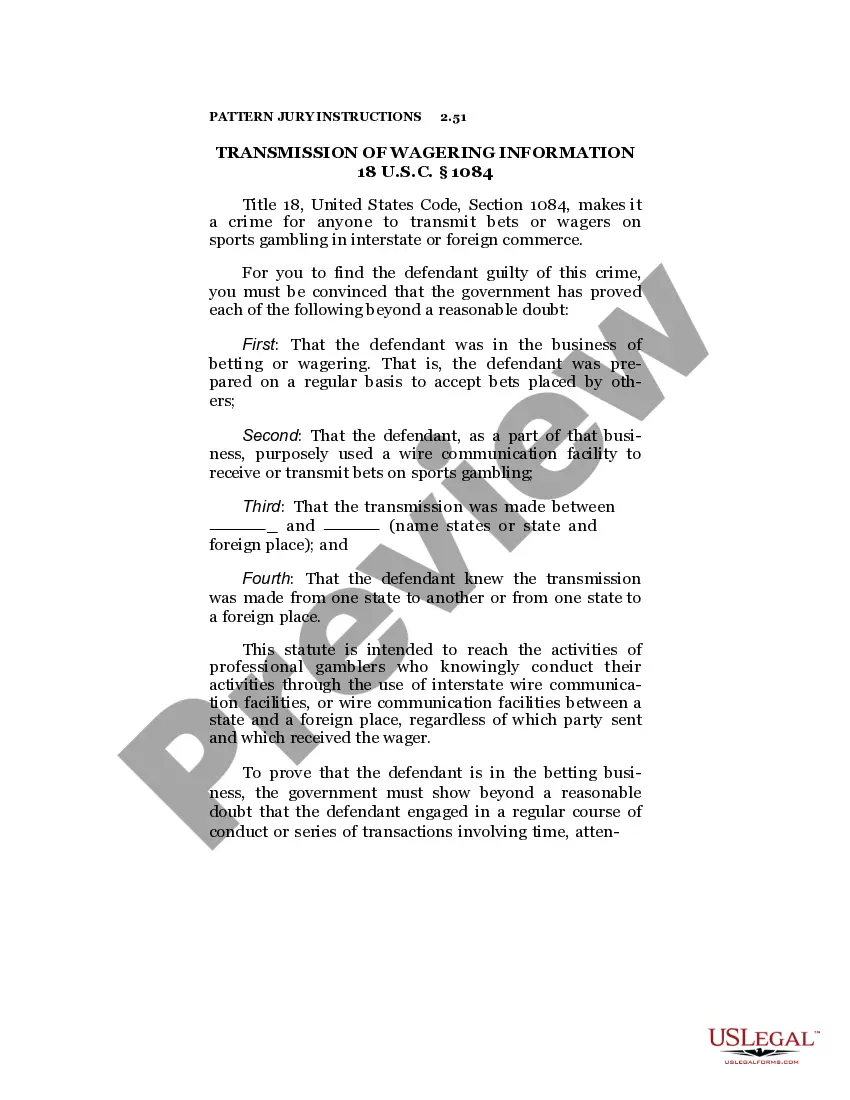
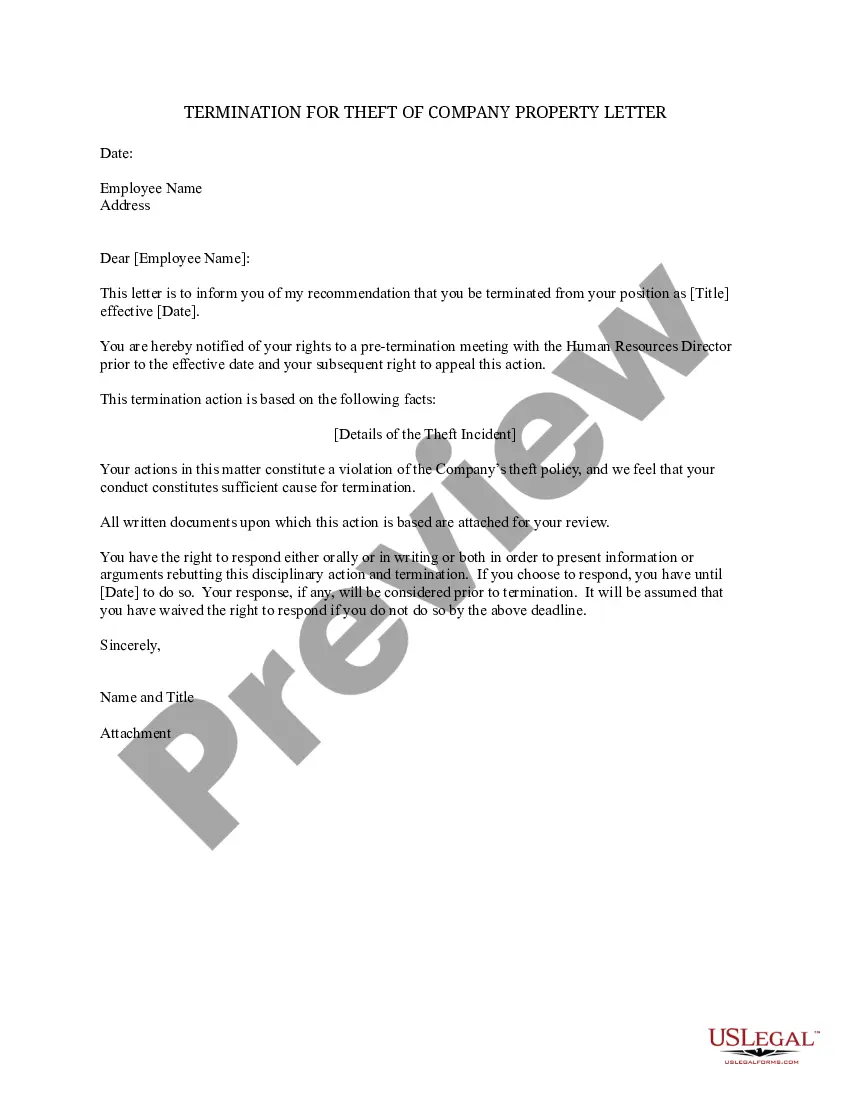
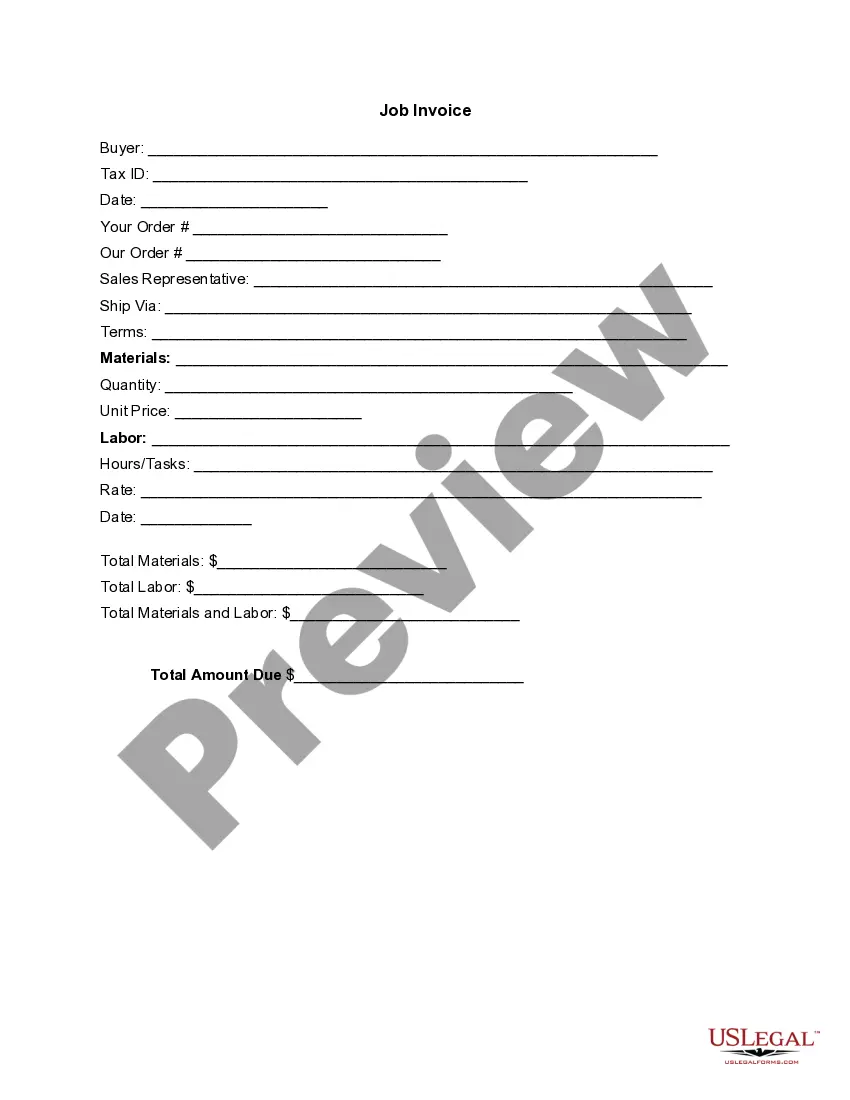
How to fill out Individual Notice Of Preexisting Condition Exclusion?
Locating the appropriate legitimate document template could pose a challenge.
Clearly, there exists a multitude of templates available online, but how can you secure the valid document you need.
Utilize the US Legal Forms website. The service offers a wide array of templates, including the New Mexico Individual Notice of Preexisting Condition Exclusion, suitable for both business and personal uses.
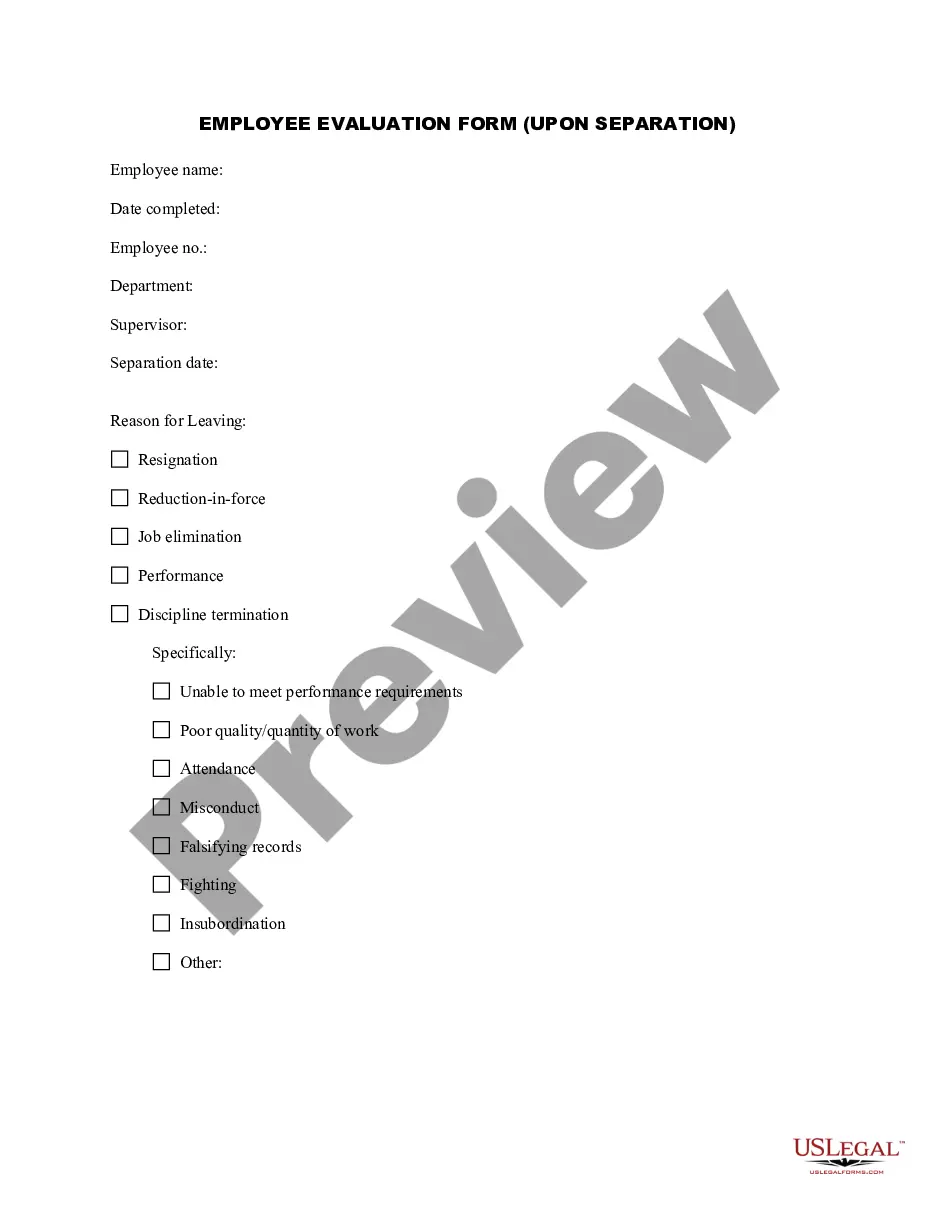
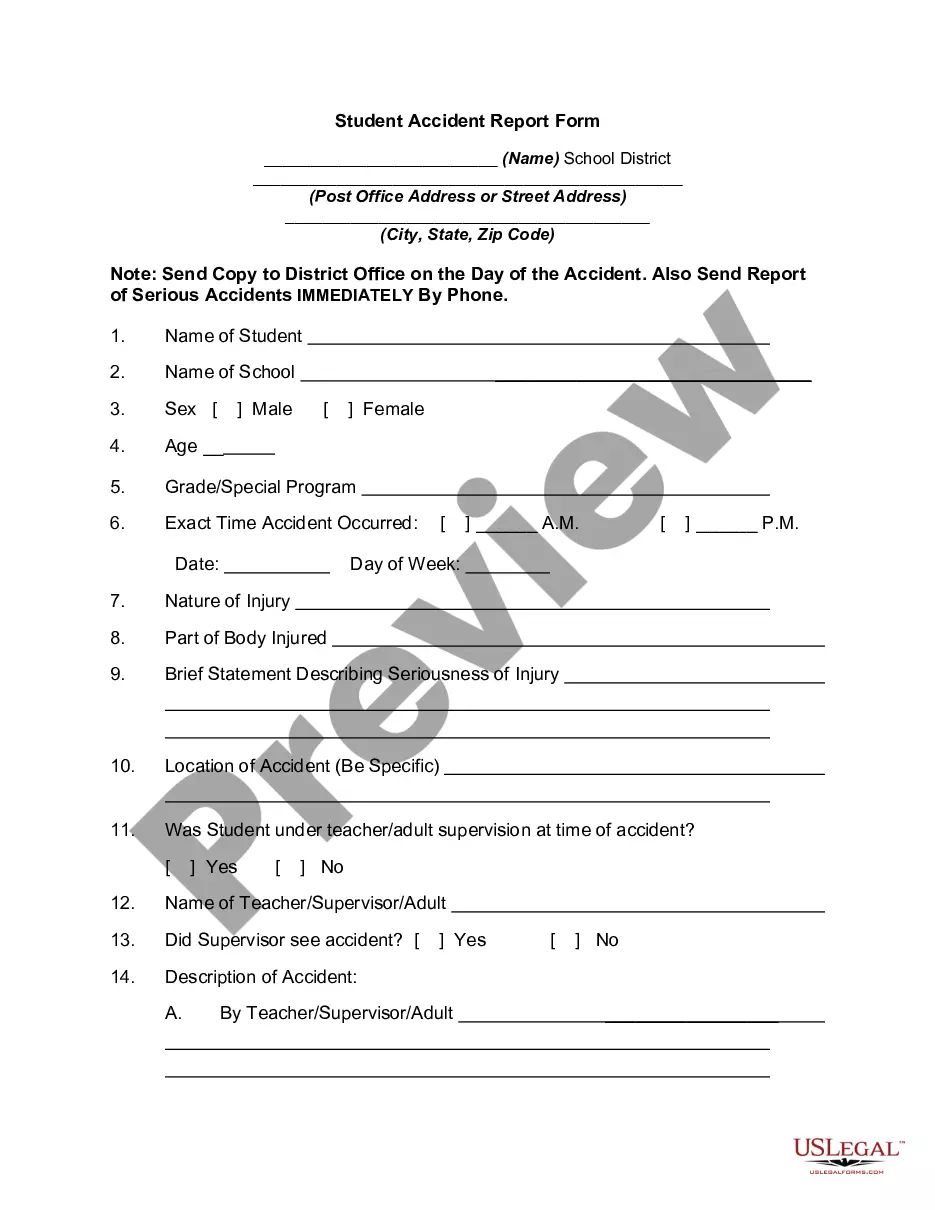
You can view the document using the Review button and read the document description to confirm it is suitable for your needs.
- All forms are verified by professionals and adhere to state and federal regulations.
- If you are already registered, Log In to your account and click the Download button to obtain the New Mexico Individual Notice of Preexisting Condition Exclusion.
- Use your account to search through the legal documents you have previously purchased.
- Navigate to the My documents section of your account and download an additional copy of the document you need.
- If you are a new user of US Legal Forms, here are straightforward instructions to follow.
- First, make sure you have selected the correct document for your area or county.
Form popularity
FAQ
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy.
Today, insurers cannot deny coverage to somebody based on pre-existing conditions, nor charge more. A pre-existing condition is any health problem or ailment that was previously diagnosed at the time of applying for coverage.
Depending on your condition, you may be eligible for coverage, but with exclusions. This means that any services or items related to your pre-existing condition will be excluded under your plan, but all other eligible treatments for ailments not related to your condition will be covered.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
Clinical Nurse Specialist, Kay Greveson, explains: A pre-existing medical condition can be affected by changes in temperature and climate and should always be declared, even if it is being controlled by medication.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
existing condition exclusion can not be longer than 12 months from your enrollment date (18 months for a late enrollee). existing condition exclusion that is applied to you must be reduced by the prior creditable coverage you have that was not interrupted by a significant break in coverage.