New Mexico General Notice of Preexisting Condition Exclusion
Description
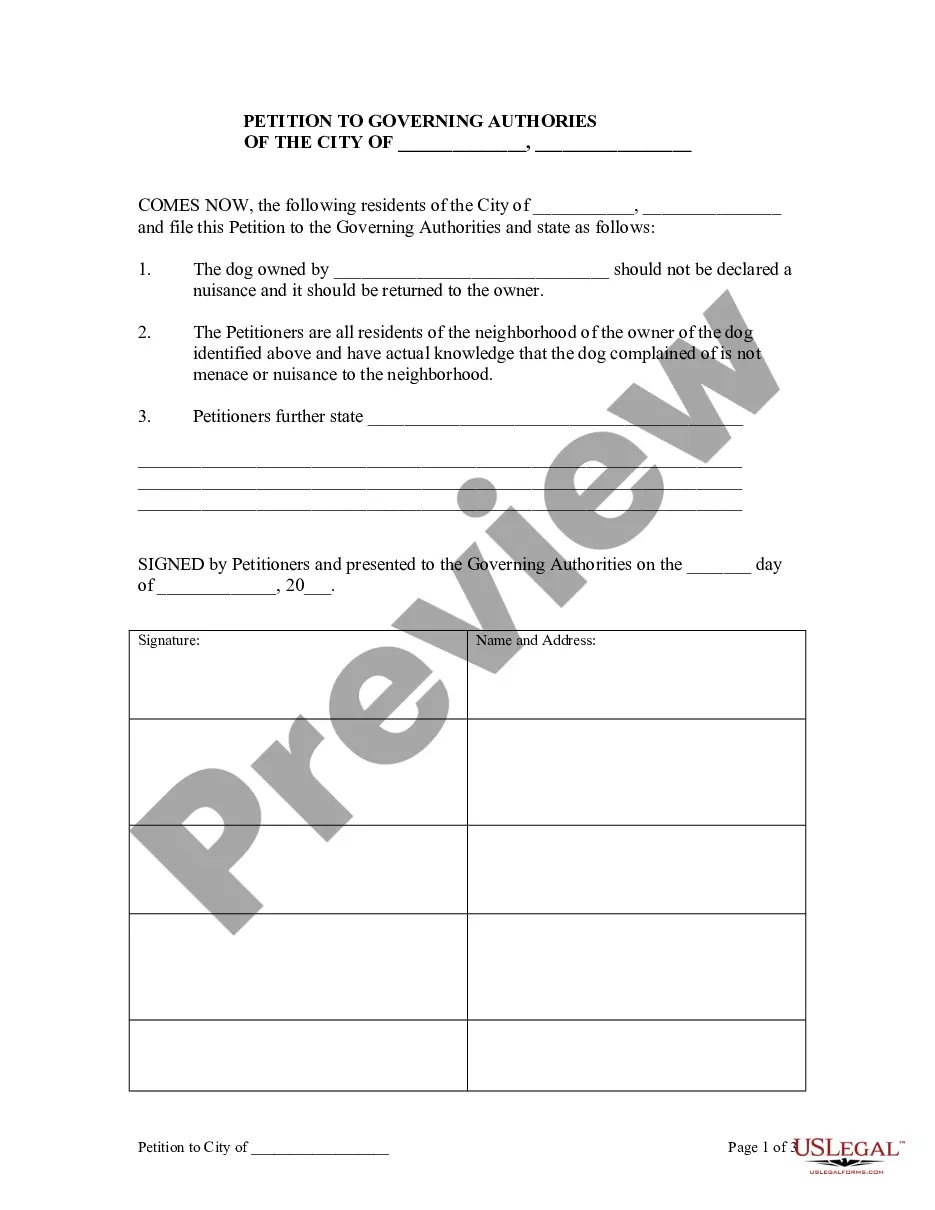
How to fill out General Notice Of Preexisting Condition Exclusion?
You might spend numerous hours online trying to discover the legal template that fulfills the federal and state criteria you need.
US Legal Forms provides a substantial collection of legal documents that are verified by professionals.
You can effortlessly download or print the New Mexico General Notice of Preexisting Condition Exclusion from the platform.
If available, utilize the Review feature to examine the template as well.
- If you already possess a US Legal Forms account, you can sign in and select the Acquire option.
- Subsequently, you can complete, modify, print, or sign the New Mexico General Notice of Preexisting Condition Exclusion.
- Each legal template you purchase remains yours indefinitely.
- To obtain another copy of a purchased form, navigate to the My documents section and click on the relevant option.
- If you’re using the US Legal Forms website for the first time, follow the simple instructions below.
- First, make sure you have selected the appropriate template for your chosen region/city.
- Review the form description to confirm you have chosen the correct document.
Form popularity
FAQ
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions. They tend to be chronic or long-term.
Clinical Nurse Specialist, Kay Greveson, explains: A pre-existing medical condition can be affected by changes in temperature and climate and should always be declared, even if it is being controlled by medication.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy.
Today, insurers cannot deny coverage to somebody based on pre-existing conditions, nor charge more. A pre-existing condition is any health problem or ailment that was previously diagnosed at the time of applying for coverage.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.