Nebraska General Notice of Preexisting Condition Exclusion
Description
How to fill out General Notice Of Preexisting Condition Exclusion?
Have you ever found yourself in a context where you need documentation for both organizations or particular functions nearly every day.
There are numerous authentic document templates accessible online, yet finding versions you can trust is challenging.
US Legal Forms offers thousands of form templates, including the Nebraska General Notice of Preexisting Condition Exclusion, which can be filled out to satisfy federal and state regulations.
Once you acquire the appropriate form, click Purchase now.
Choose the pricing plan you prefer, complete the necessary details to create your account, and pay for your order using your PayPal, Visa, or Mastercard.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Nebraska General Notice of Preexisting Condition Exclusion template.
- If you do not possess an account and wish to start using US Legal Forms, follow these steps.
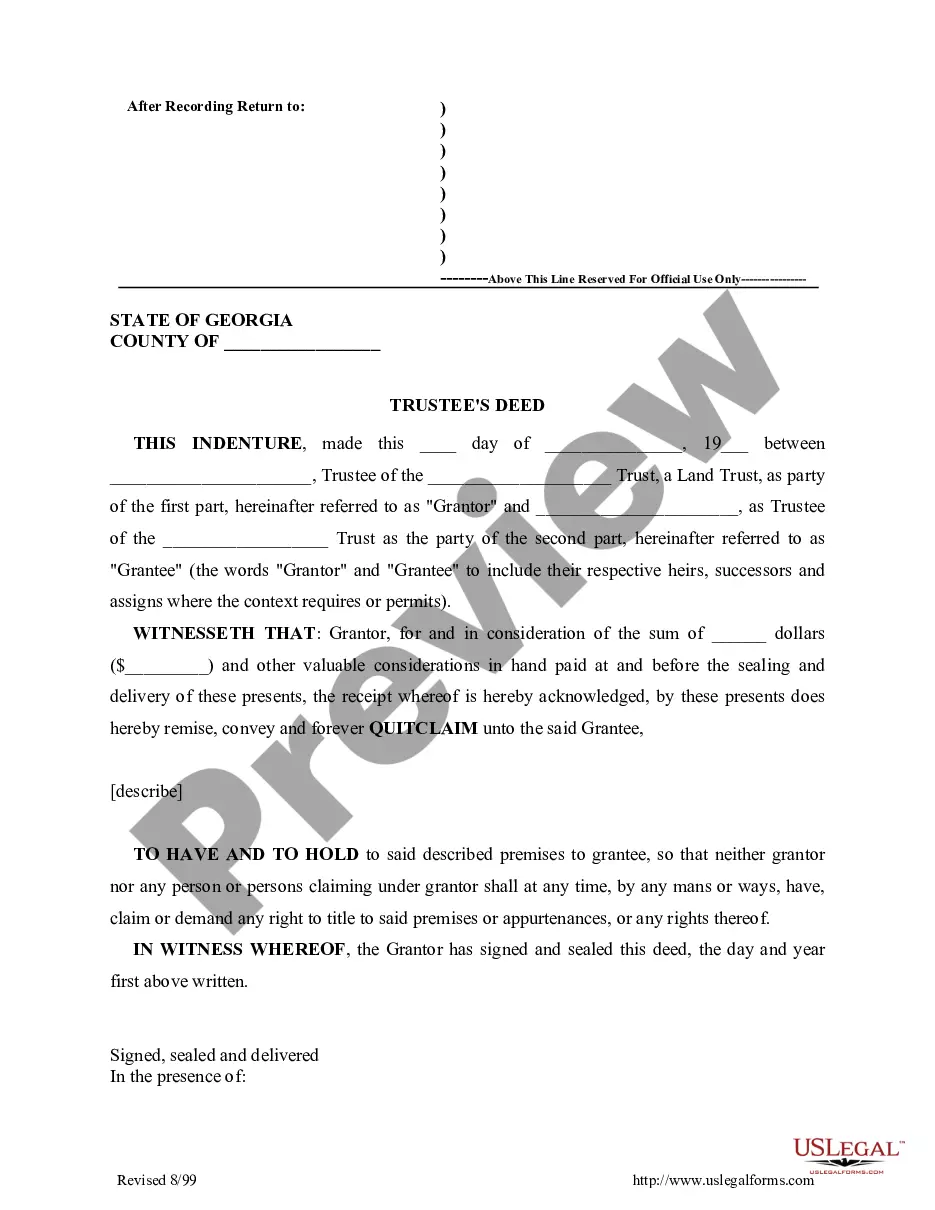
- Find the form you need and ensure it is for the correct state/area.
- Utilize the Review button to examine the form.
- Verify the information to ensure you have selected the right form.
- If the form is not what you're looking for, use the Search area to locate the form that meets your needs and criteria.
Form popularity
FAQ
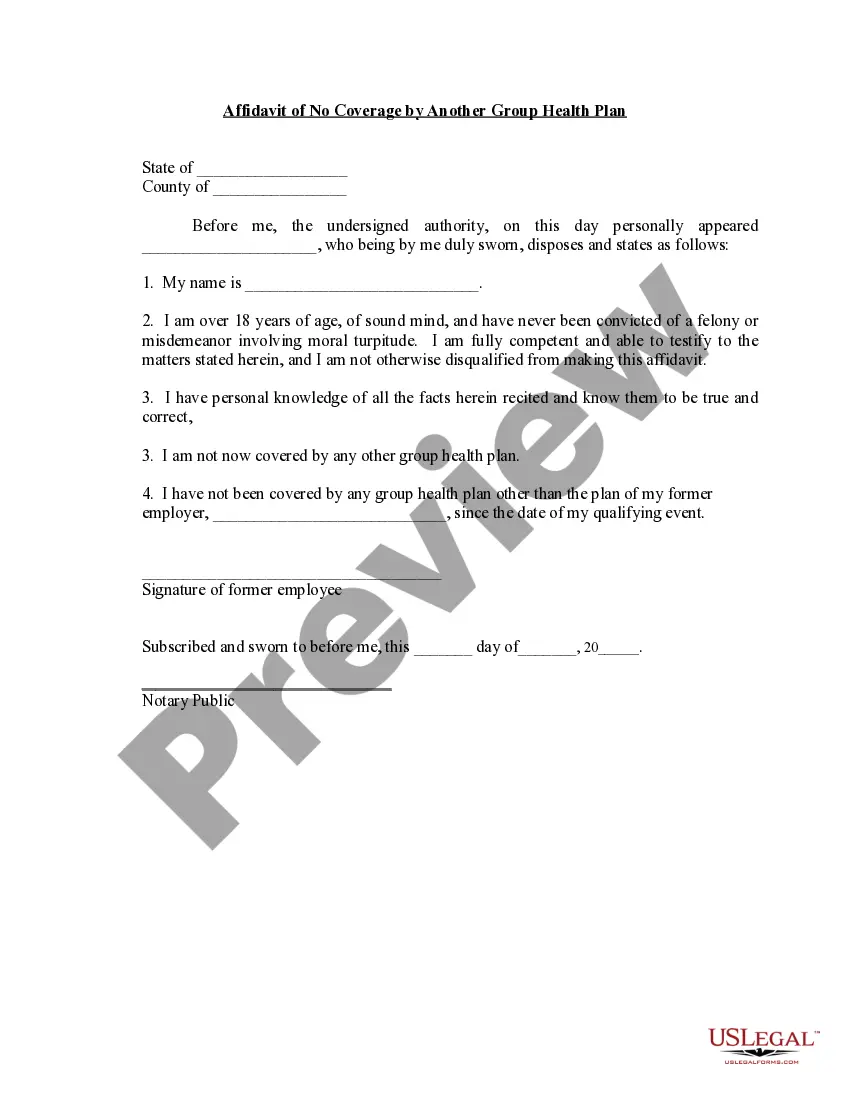
Pre-existing condition exclusions are clauses in health insurance policies that restrict coverage for ailments or conditions that existed before the policy was issued. These exclusions can limit your access to essential health care services when you need them most. The Nebraska General Notice of Preexisting Condition Exclusion provides crucial information on how these clauses operate. By familiarizing yourself with these exclusions, you can make informed decisions about your health care and insurance options.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
However, a feature of a travel insurance policy known as a pre-existing medical condition exclusion waiver could let you, for instance, cancel a trip due to a flare up of an existing condition and then be reimbursed for nonrefundable travel costs.
Examples of pre-existing conditions include cancer, asthma, diabetes, and even pregnancy. Under the Affordable Care Act (Obamacare), health insurance companies cannot refuse to cover you because of any pre-existing conditions nor can they charge you more money for coverage or subject you to a waiting period.
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions. They tend to be chronic or long-term.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.