Arizona Qualifying Event Notice Information for Employer to Plan Administrator
Description
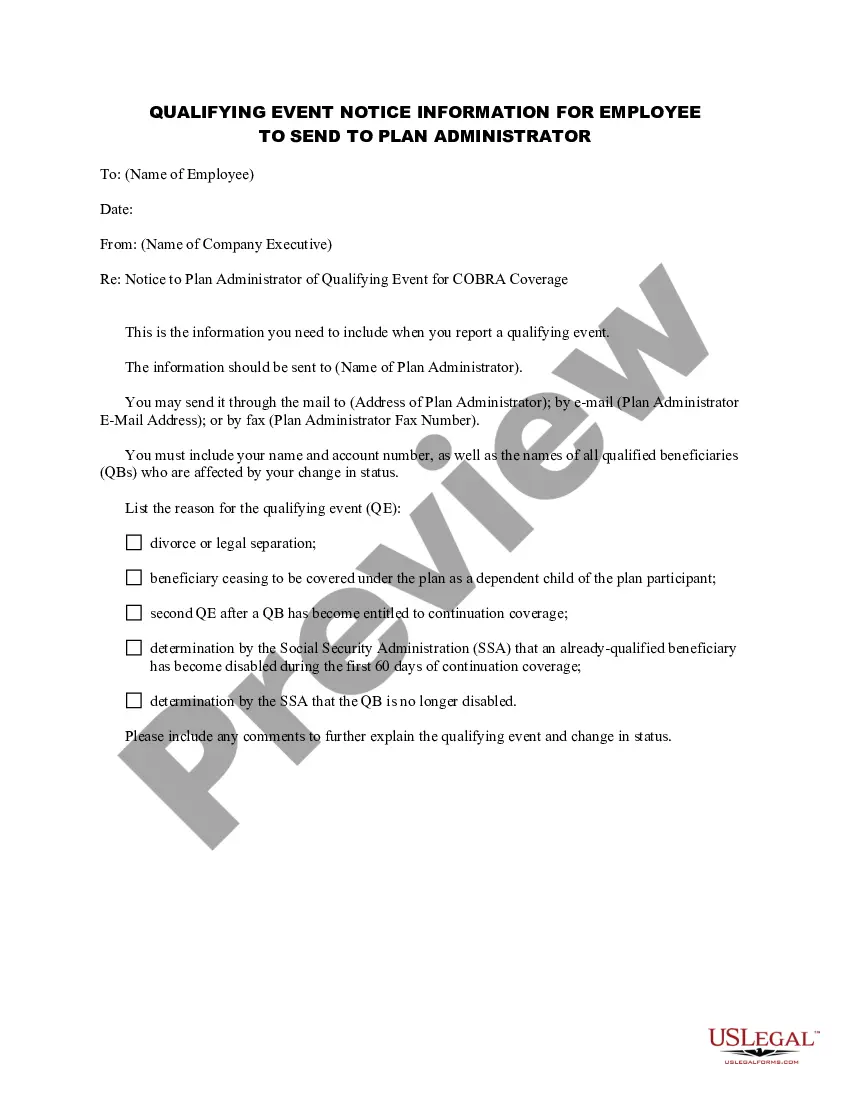
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
Locating the appropriate legal document template can be a challenge. Obviously, there are numerous templates accessible on the internet, but how do you locate the legal format you require.
Utilize the US Legal Forms website. This service offers a vast array of templates, including the Arizona Qualifying Event Notice Information for Employer to Plan Administrator, which you can employ for both business and personal purposes. All forms are vetted by professionals and adhere to state and federal regulations.
If you are already registered, Log In to your account and click the Download button to obtain the Arizona Qualifying Event Notice Information for Employer to Plan Administrator. Use your account to review the legal forms you have purchased previously. Go to the My documents tab in your account to retrieve another copy of the document you need.
Choose the document format and download the legal document template to your device. Complete, modify, print, and sign the purchased Arizona Qualifying Event Notice Information for Employer to Plan Administrator. US Legal Forms is the largest repository of legal forms where you can find numerous document templates. Use the service to obtain professionally crafted documents that conform to state regulations.
- First, ensure you have selected the correct form for your location/county.
- You can review the form using the Preview button and check the form details to make sure it is suitable for you.
- If the form does not meet your requirements, use the Search field to find the correct form.
- Once you are confident that the form is appropriate, click the Buy now button to acquire the form.
- Select the pricing plan you prefer and enter the required information.
- Create your account and complete the purchase using your PayPal account or credit card.
Form popularity
FAQ
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Arizona Healthcare Insurance: What you need to knowThere is no state law requiring employers to offer group healthcare insurance to their employees, but most employers do provide this benefit.
From a legal standpoint, there is no federal law that says companies must offer health insurance to their employees. However, employers' health insurance requirements do apply for some businesses depending on their size.
In Arizona, all employers with 50 or more full-time employees are required to offer some form of health insurance benefit. Once you have 50 employees, you are considered a large employer. This means that you may face penalties if you do not offer health insurance.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Are All Employers Required To Offer Health Insurance? Absolutely, yes. As a part of the Consolidated Revised Guidelines for resuming workplace operations by the Ministry of Home Affairs, on 15th April 2020, the Insurance Regulatory and Development Authority of India (IRDAI) released an order (No.