Cobra Coverage Complete Formula
Description
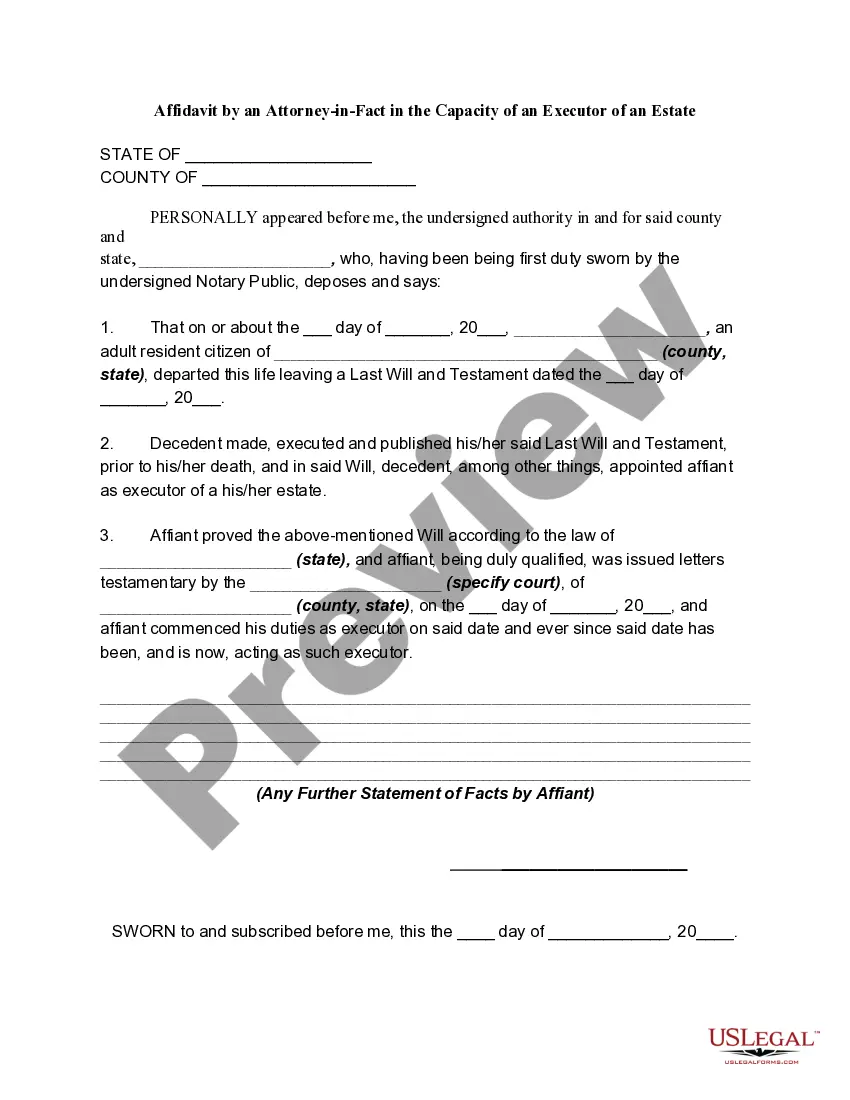
How to fill out COBRA Continuation Coverage Election Form?
Securing a reliable resource to obtain the latest and pertinent legal samples constitutes a significant part of navigating bureaucracy.
Selecting the appropriate legal documents requires precision and careful consideration, which underscores the importance of sourcing Cobra Coverage Complete Formula exclusively from trustworthy providers, such as US Legal Forms. An incorrect template can squander your time and delay your situation.
Once you have the document on your device, you can modify it with the editor or print it out to fill it in manually. Eliminate the hassle associated with your legal paperwork. Explore the vast US Legal Forms library to discover legal samples, assess their relevance to your circumstances, and download them instantly.
- Utilize the catalog navigation or search functionality to find your sample.
- Examine the document's details to ensure it aligns with your state and local requirements.
- Preview the document, if available, to confirm it is the template you need.
- Return to your search to locate a suitable template if the Cobra Coverage Complete Formula does not fulfill your requirements.
- If you are confident about the document’s applicability, download it.
- If you are a registered user, click Log in to verify your identity and access your chosen forms in My documents.
- If you do not possess an account, click Buy now to acquire the form.
- Choose the pricing option that meets your needs.
- Move on to the enrollment process to finalize your purchase.
- Conclude your transaction by selecting a payment method (credit card or PayPal).
- Pick the format for downloading the Cobra Coverage Complete Formula.
Form popularity
FAQ
The 60-day loophole for COBRA refers to the period during which you can enroll in COBRA continuation coverage from the date you receive your election notice. If you decide to opt for COBRA coverage, you can take advantage of this time frame to weigh your options. This is vital in utilizing the 'Cobra coverage complete formula' for effective decision-making. For more insights and assistance, the US Legal Forms platform can guide you through this process.
If your employer contributes $400 per month, the total cost of your job-based plan is $650 per month. To calculate your total monthly COBRA premium, add a 2% service charge to the $650 for a grand total of $663 per month. Here's a sample calculation: Your contribution: $125 per paycheck X 2 = $250 per month.
Both full- and part-time employees are counted to determine whether a plan is subject to COBRA. Each part-time employee counts as a fraction of a full-time employee, with the fraction equal to the number of hours worked divided by the hours an employee must work to be considered full time.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Individuals who are employed by California employers at the time they become eligible for COBRA continuation coverage and whose COBRA coverage would otherwise end in 18 months may, under Cal-COBRA, continue their coverage with the same group carrier or HMO for up to a total of 36 months.
With COBRA insurance, the individual becomes responsible for the costs the employer once was responsible for. This may result in paying average monthly premiums of $623 to continue your individual coverage or $1,778 for family coverage. COBRA premiums range depending on if you have an individual or family plan.