Riverside California Model General Notice of COBRA Continuation Coverage Rights
Description
How to fill out Model General Notice Of COBRA Continuation Coverage Rights?
How long does it usually take you to create a legal document.
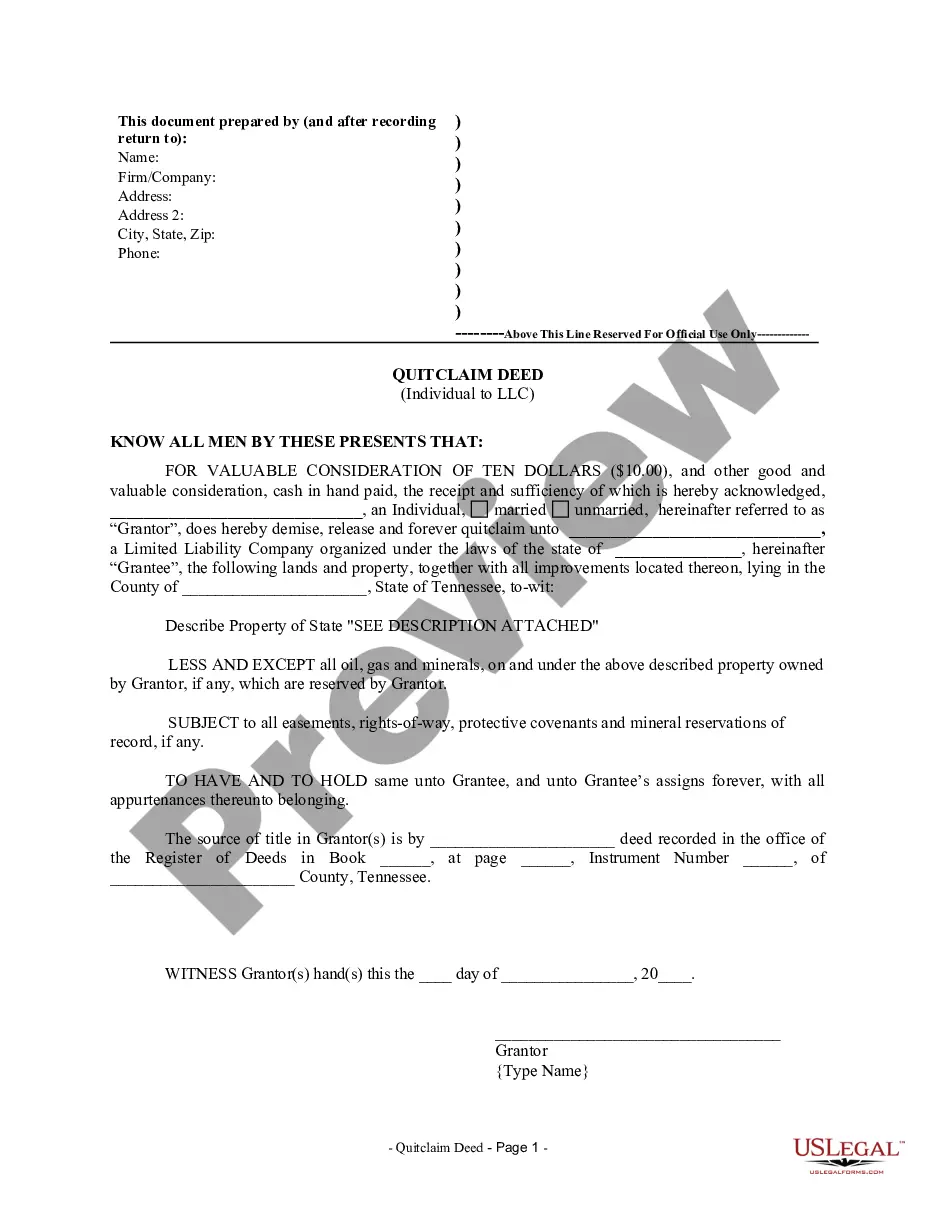
As each state has its own laws and regulations for various life circumstances, finding a Riverside Model General Notice of COBRA Continuation Coverage Rights that meets all local regulations can be exhausting, and hiring a professional lawyer for it can be costly. Numerous online services provide the most common state-specific templates for download, but utilizing the US Legal Forms library is the most advantageous.
US Legal Forms offers the largest online collection of templates, organized by states and areas of application. Along with the Riverside Model General Notice of COBRA Continuation Coverage Rights, you can acquire any specific document needed to manage your business or personal matters, adhering to your county's regulations. All samples are verified by professionals for their accuracy, ensuring you can prepare your documents correctly.
Print the document or use any preferred online editor to complete it electronically. Regardless of how often you need to utilize the acquired template, you can find all the files you've ever saved in your profile by accessing the My documents tab. Give it a try!
- Using the service is exceptionally straightforward.
- If you already have an account on the website and your subscription is active, you merely need to Log In, select the required template, and download it.
- You can save the document in your profile at any time in the future.
- If you are new to the platform, there are a few additional steps to complete before obtaining your Riverside Model General Notice of COBRA Continuation Coverage Rights.
- Review the information on the current page.
- Read the description of the template or Preview it (if available).
- Look for another document using the related option in the header.
- Click Buy Now once you are confident in your choice of document.
- Select the subscription plan that fits you best.
- Create an account on the site or Log In to continue to payment options.
- Make a payment via PayPal or with your credit card.
- Change the file format if necessary.
- Click Download to save the Riverside Model General Notice of COBRA Continuation Coverage Rights.
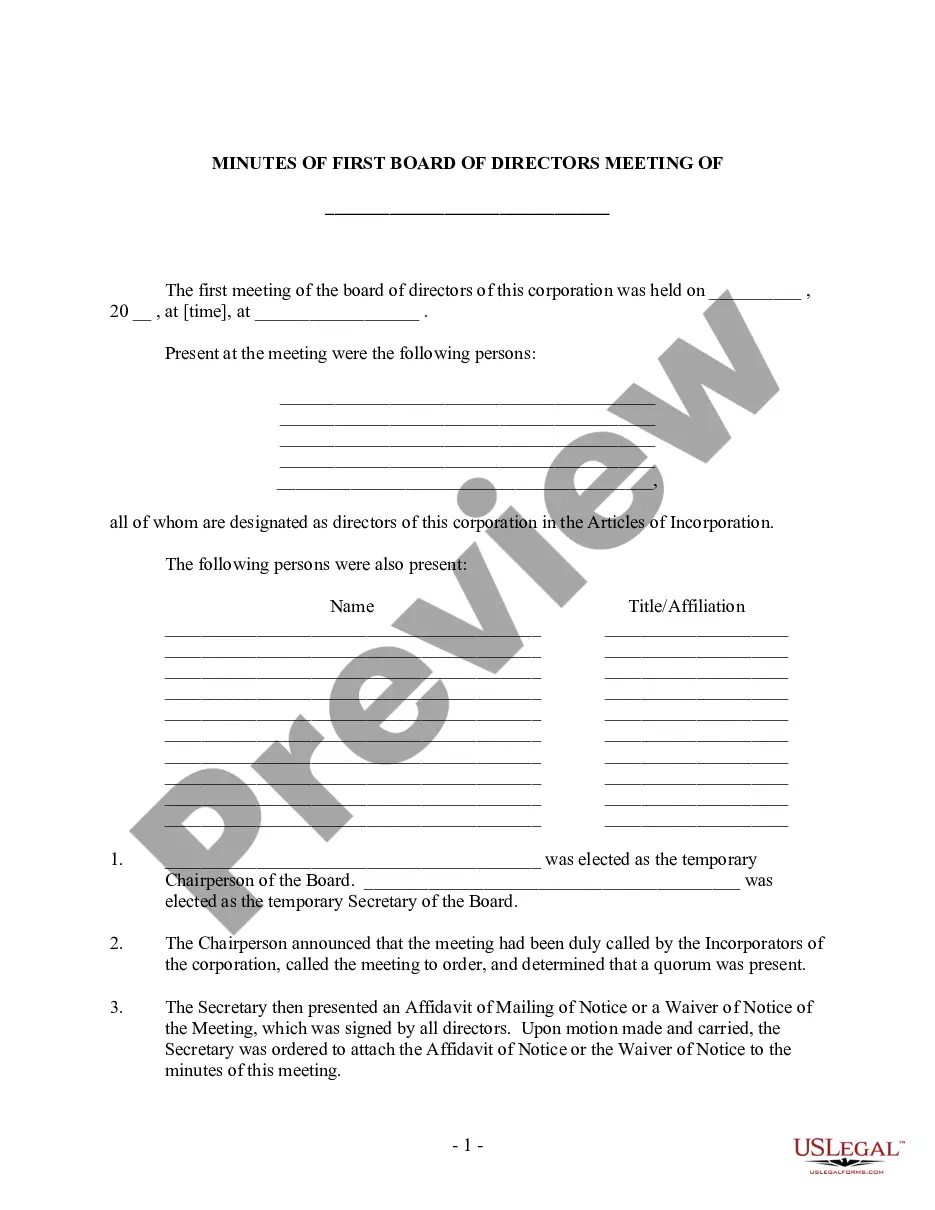
Form popularity
FAQ
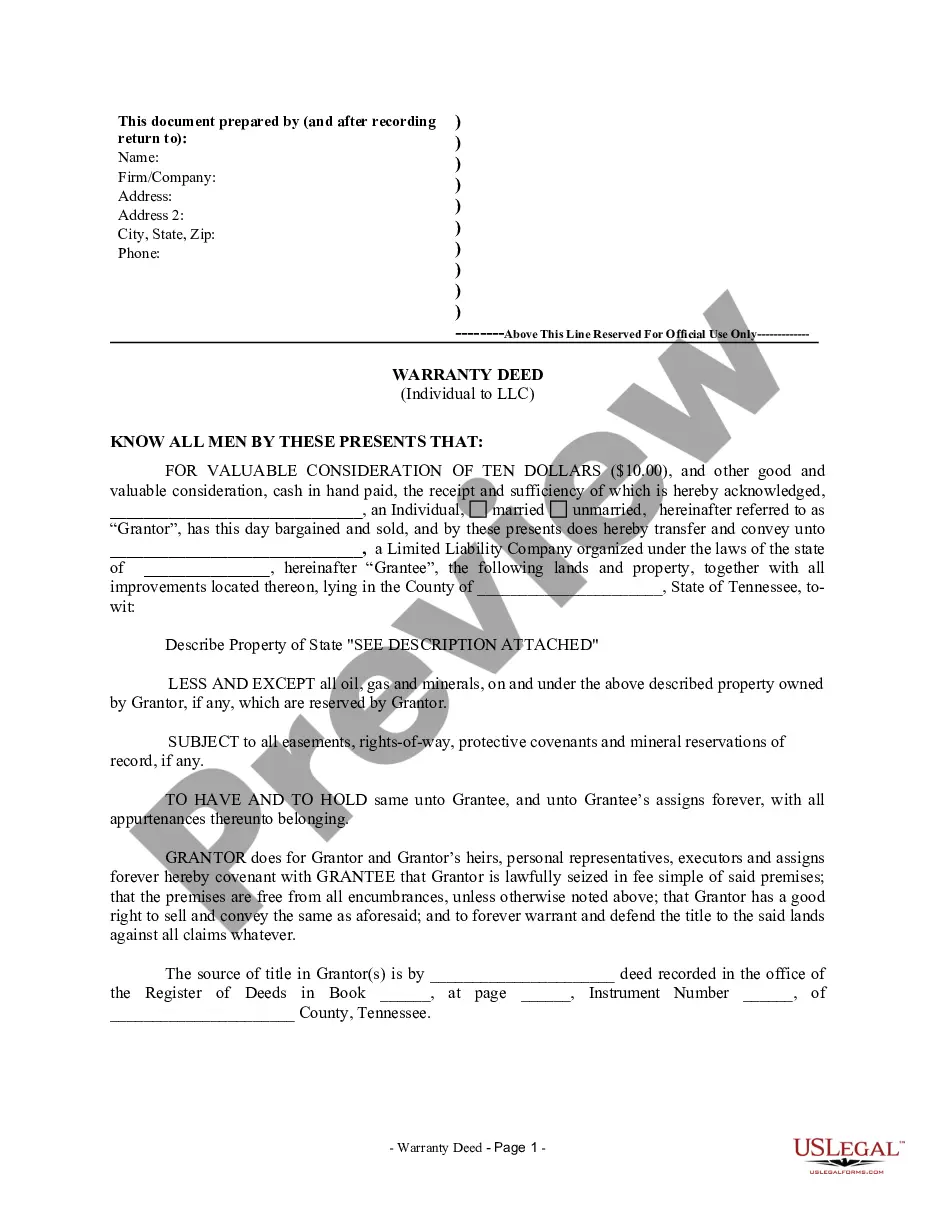
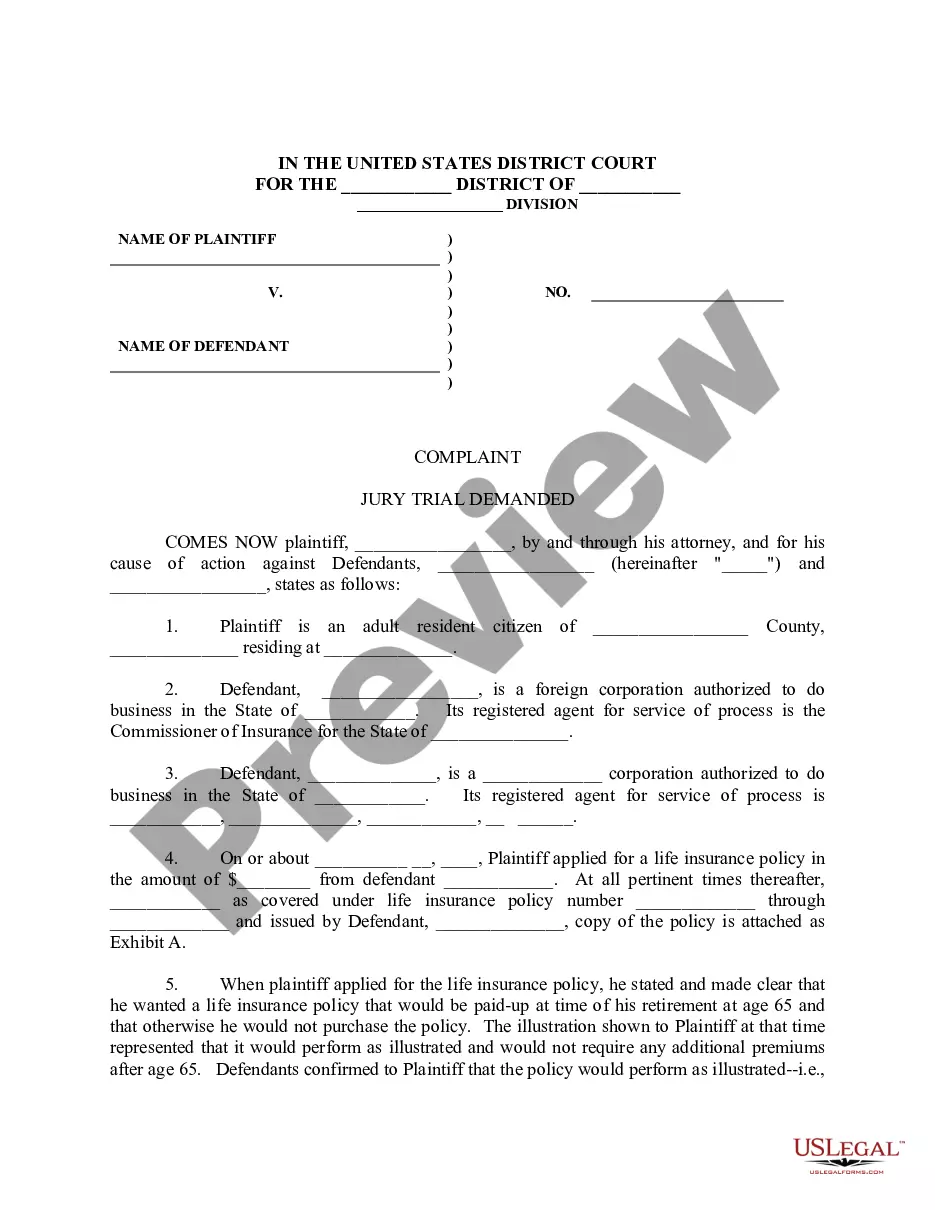
COBRA continuation rights are legal entitlements that allow you to keep your employer-sponsored health insurance after experiencing certain events, such as job loss or reduced hours. The Riverside California Model General Notice of COBRA Continuation Coverage Rights outlines these rights, ensuring you know how to maintain your health insurance coverage. It is important to understand these rights to secure necessary medical care. By utilizing resources like uslegalforms, you can obtain clear guidance on your COBRA options.
In California, employers must send the Riverside California Model General Notice of COBRA Continuation Coverage Rights within 44 days of the qualifying event. This notice informs you of your rights to continued health coverage under COBRA. Timely notification is crucial for ensuring that you can make informed decisions about your healthcare options. If you have not received your notice within this timeframe, it is advisable to contact your employer.
Paying for Coverage The cost to the plan is both the portion paid by employees and any portion paid by the employer before the qualifying event. The COBRA premium can equal 100 percent of that combined amount plus a 2 percent administrative fee.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
State continuation coverage refers to state laws that enable employees to extend their employer-sponsored group health insurance even if they are not eligible for an extension through COBRA. While COBRA law applies throughout the U.S., it is only applicable to employers with 20 or more employees.
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,