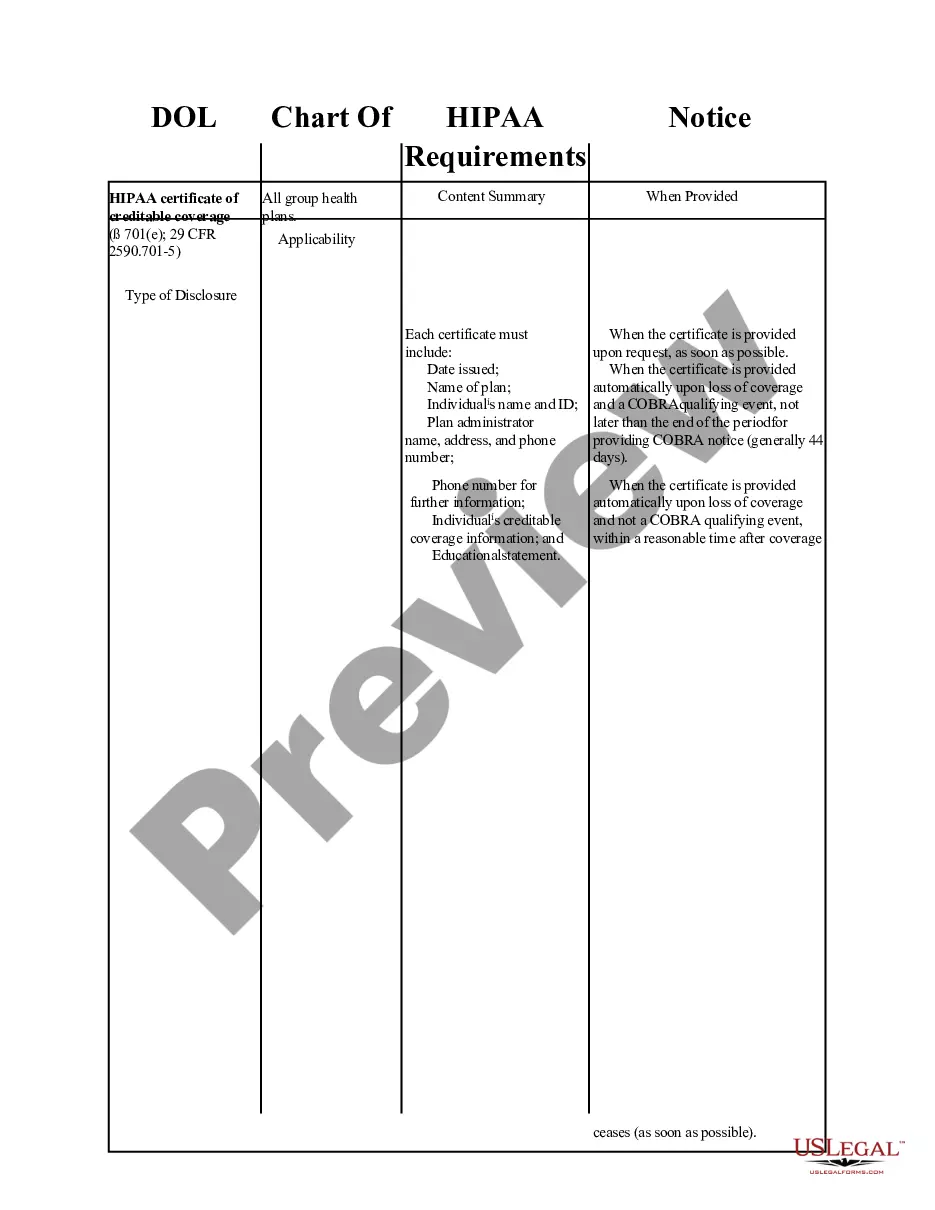
Washington DOL Chart of HIPAA Notice Requirements
Description
How to fill out DOL Chart Of HIPAA Notice Requirements?
Selecting the appropriate licensed document format can be challenging. Certainly, there are numerous designs available online, but how do you get the licensed form you need.
Utilize the US Legal Forms platform. This service offers a wide array of templates, such as the Washington DOL Chart of HIPAA Notice Requirements, suitable for both business and personal purposes.
All forms are reviewed by experts and comply with state and federal regulations.
Once you are confident the form is accurate, click the Get now button to obtain the document. Choose the pricing plan you prefer and enter the necessary information. Create your account and complete the transaction using your PayPal account or credit card. Select the document format and download the legal document format to your device. Finally, complete, modify, print, and sign the acquired Washington DOL Chart of HIPAA Notice Requirements. US Legal Forms is the largest repository of legal documents where you can explore a variety of document formats. Take advantage of the service to download professionally crafted papers that meet state requirements.
- If you are already registered, Log In to your account and click the Download button to access the Washington DOL Chart of HIPAA Notice Requirements.
- Use your account to review the legal documents you have previously obtained.
- Visit the My documents section of your account to retrieve another copy of the document you need.
- If you are a new user of US Legal Forms, here are some simple steps to follow.
- First, ensure you have selected the correct form for your city/region. You can review the form using the Review button and read the form details to confirm it is suitable for you.
- If the form does not fulfill your requirements, use the Search field to find the correct document.
Form popularity
FAQ
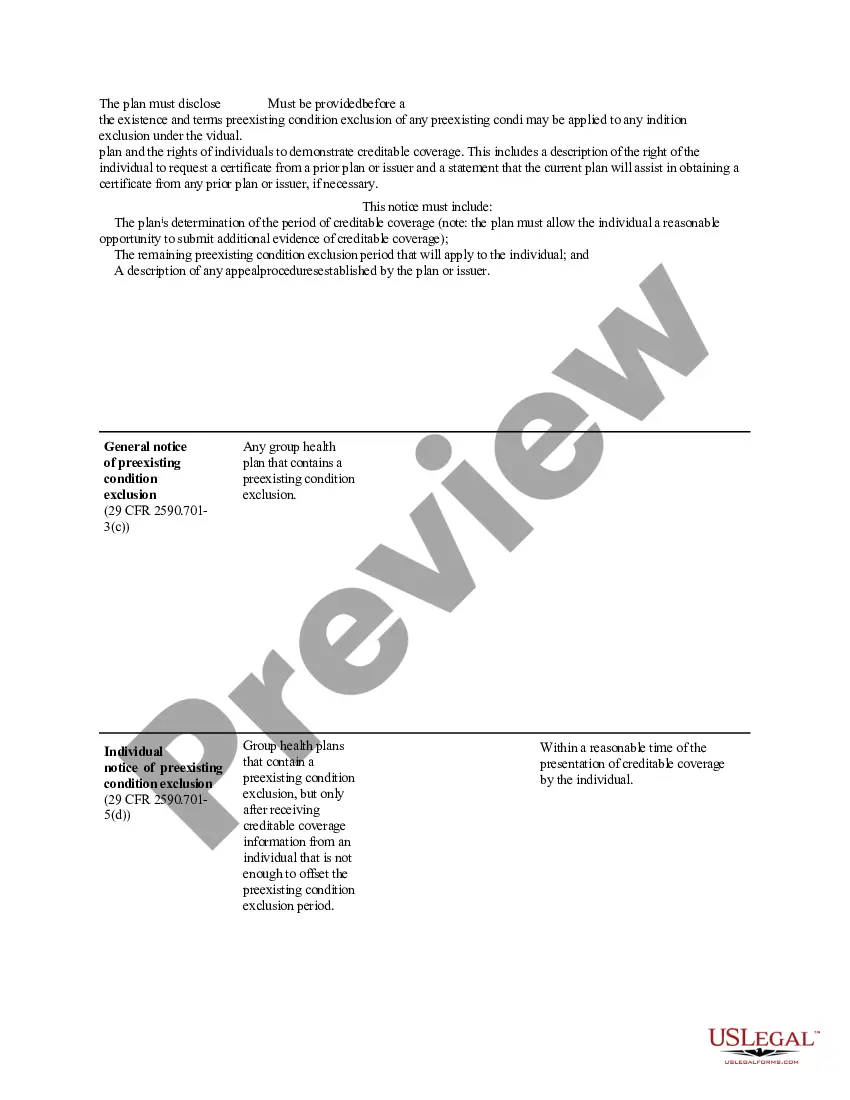
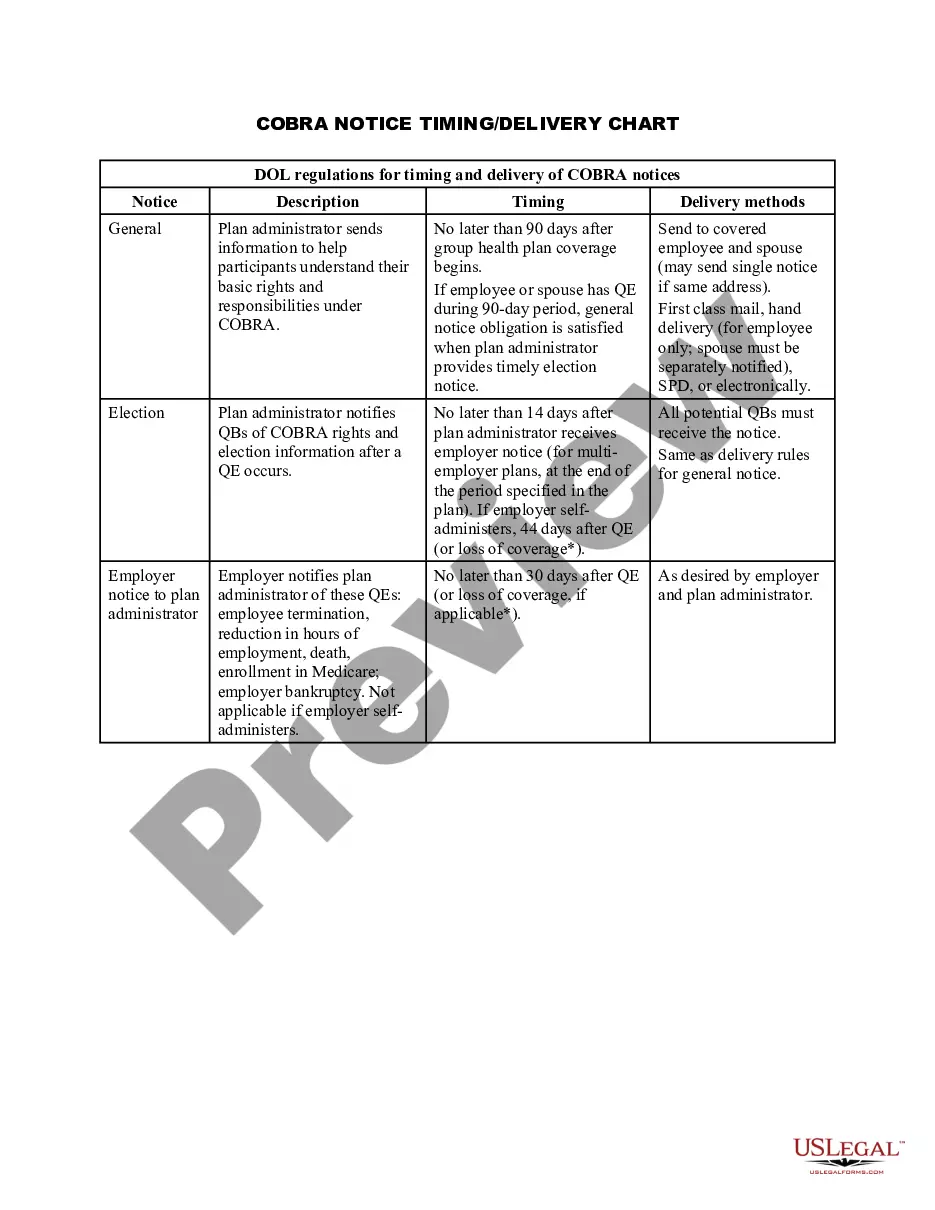
HIPAA'S Effect on COBRA While HIPAA and COBRA are separate laws, HIPAA does affect COBRA continuation coverage. Effective January 1, 1997, HIPAA made changes to COBRA continuation coverage in the areas of disability extension, definition of qualified beneficiary, and the duration of COBRA continuation coverage.
HIPAA'S Effect on COBRA While HIPAA and COBRA are separate laws, HIPAA does affect COBRA continuation coverage. Effective January 1, 1997, HIPAA made changes to COBRA continuation coverage in the areas of disability extension, definition of qualified beneficiary, and the duration of COBRA continuation coverage.
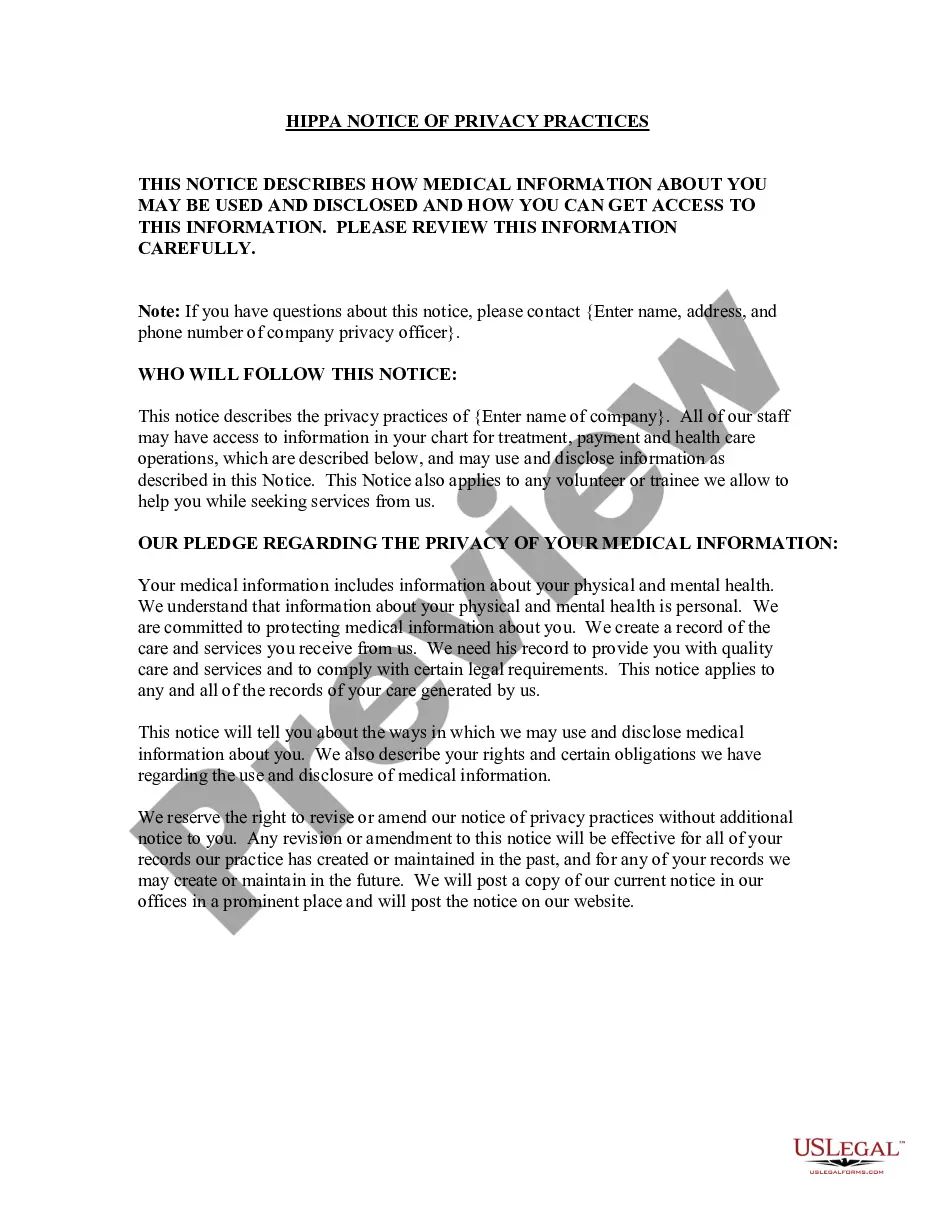
Title I, Health Insurance Access, Portability, and Renewability, Title II, Preventing Healthcare Fraud & Abuse, Administrative Simplification, & Medical Liability Reform, Title III, Tax-Related Health Provisions, Title IV, Application and Enforcement of Group Health Insurance Requirments, and Title V, Revenue Offsets.
Updated July 12, 2018. A certificate of Creditable Coverage (COCC) is a document provided by your previous insurance carrier that proves that your insurance has ended. This includes the name of the member to whom it applies as well as the coverage effective date and cancelation date.
Washington medical records laws state that only the patient may authorize disclosure of medical records to anyone other than health care providers, penal institution officials, or public health authorities.
Title III provides for certain deductions for medical insurance, and makes other changes to health insurance law.
Section 421(e) of HIPAA requires group health plans that are subject to COBRA to notify, by November 1, 1996, individuals who have elected COBRA continuation coverage of these changes.
COBRA continuation coverage gives Florida workers and families who lose their employer-sponsored health insurance benefits the right to choose to continue their group health plan for a limited period of time, under certain circumstances, such as job loss, a reduction in hours worked, divorce, and other qualifying
In most cases, COBRA provides for continuation of health plan coverage for up to 18 months following the work separation.
When you apply for a HIPAA plan, you should provide a Certificate of Creditable Coverage from your last health plan. This is a letter that says how long you have been covered and provides proof that you have had at least 18 months of coverage.