Virginia Election Form for Continuation of Benefits - COBRA
Description
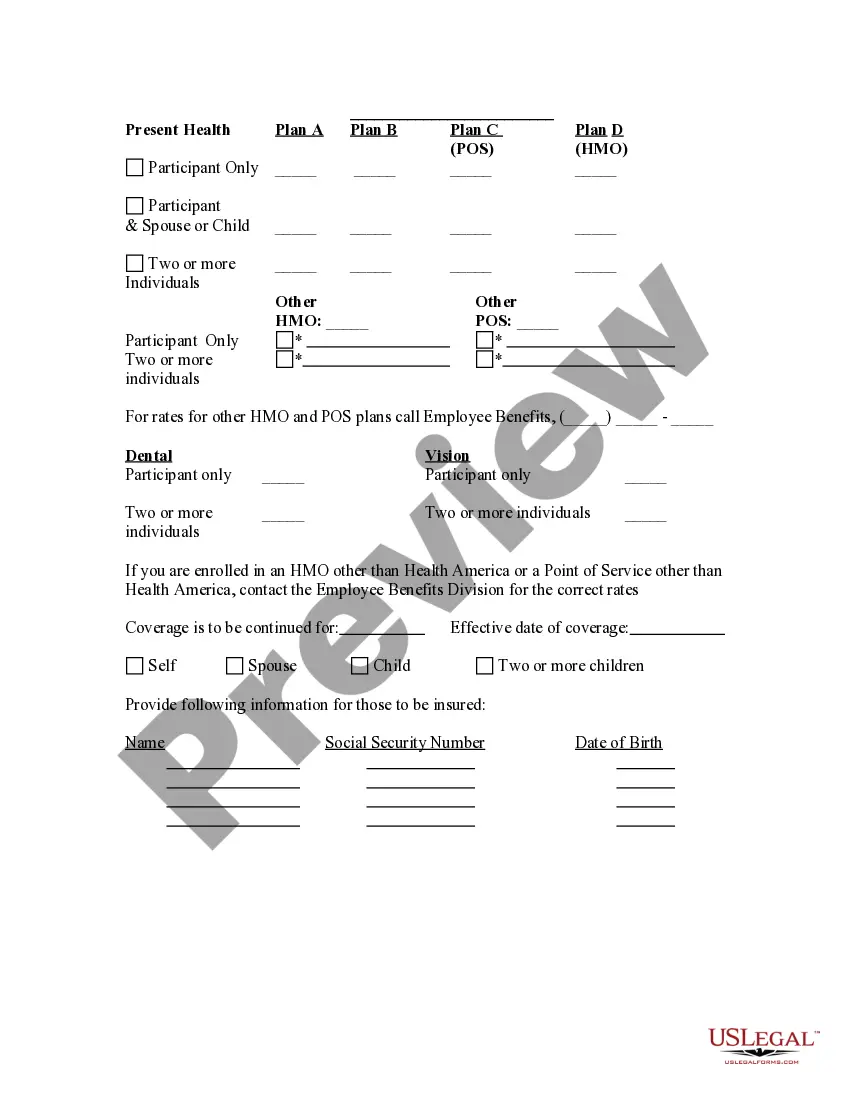
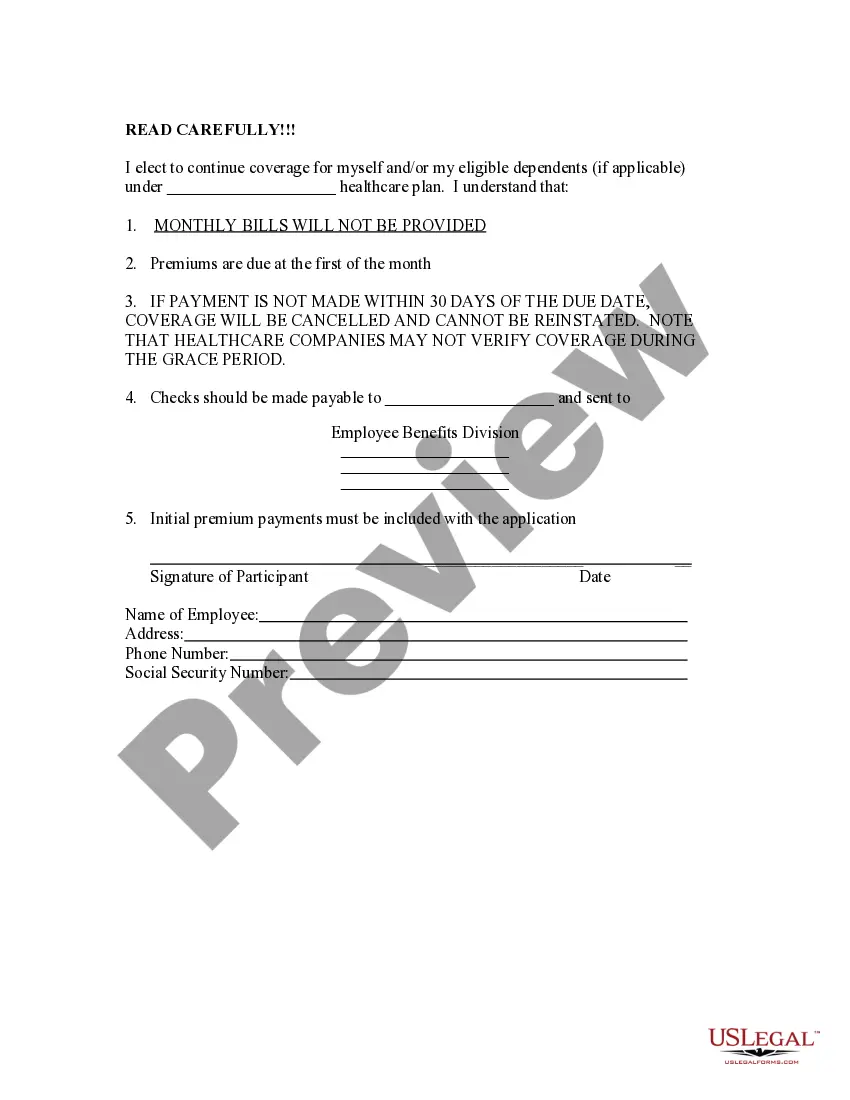
How to fill out Election Form For Continuation Of Benefits - COBRA?
Have you ever found yourself in a situation where you needed documentation for either business or personal reasons almost all the time.
There are numerous legal document templates accessible online, but locating ones you can rely on is quite challenging.
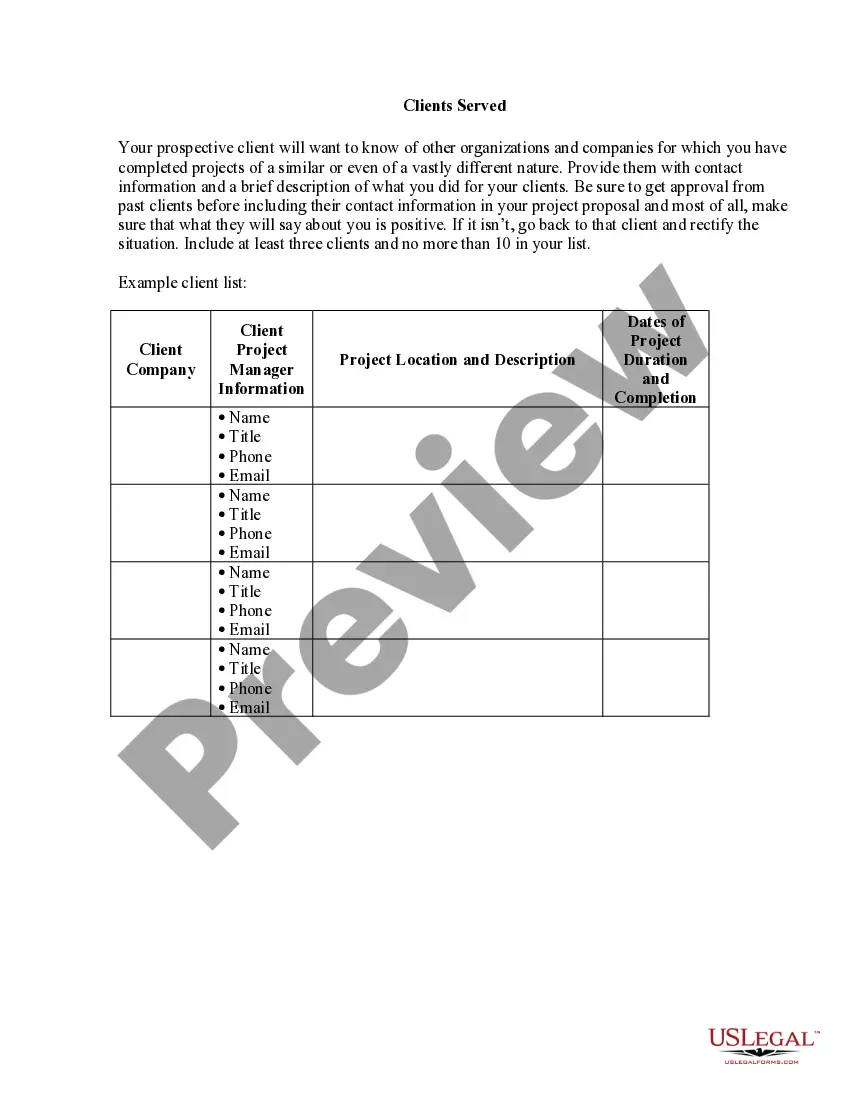
US Legal Forms offers thousands of template documents, including the Virginia Election Form for Continuation of Benefits - COBRA, that are designed to comply with state and federal regulations.
Once you have identified the right document, simply click Purchase now.
Choose the pricing plan you prefer, fill in the necessary information to create your account, and purchase your order using PayPal or a Visa or Mastercard.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Then, you will be able to download the Virginia Election Form for Continuation of Benefits - COBRA template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Select the document you require and ensure it is for your correct city/state.
- Utilize the Preview button to review the form.
- Examine the description to verify that you have selected the correct document.
- If the document is not what you are looking for, use the Search box to find the form that meets your needs.
Form popularity
FAQ
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
How Long Does COBRA Last After You Quit? You may remain on your former employer's COBRA insurance plan for up to 18 months. Depending on your circumstances you or your qualified dependents may be eligible for up to 36 months of continuing coverage.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The maximum period of Extended Coverage/COBRA available to qualified beneficiaries is based on the qualifying event. In the case of a loss of coverage due to end of employment or reduction in hours of employment, coverage generally may be continued for up to a total of 18 months.