Tennessee Summary of Rights and Obligations under COBRA
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
US Legal Forms - one of the largest collections of legal documents in the United States - provides a vast assortment of legal templates you can download or print.
By using the website, you can access thousands of forms for business and personal purposes, organized by categories, states, or keywords. You can find the latest versions of forms like the Tennessee Summary of Rights and Obligations under COBRA in just a few minutes.
If you already have a monthly subscription, Log In and download the Tennessee Summary of Rights and Obligations under COBRA from your US Legal Forms library. The Download button will appear on each form you view. You have access to all previously obtained forms in the My documents section of your account.
Make changes. Complete, edit, print, and sign the downloaded Tennessee Summary of Rights and Obligations under COBRA.
Each template you add to your account has no expiration date and is yours indefinitely. So, if you want to download or print another copy, just return to the My documents section and click on the form you need. Access the Tennessee Summary of Rights and Obligations under COBRA with US Legal Forms, the most extensive library of legal document templates. Utilize thousands of professional and state-specific templates that meet your business or personal requirements.
- If you are using US Legal Forms for the first time, here are some simple tips to get you started.
- Confirm you have chosen the correct form for your city/county. Click the Review button to evaluate the form's content. Check the form description to ensure you've selected the right document.
- If the form does not meet your requirements, utilize the Search field at the top of the screen to find the one that does.
- Once you are satisfied with the form, affirm your choice by clicking the Buy now button. Next, select your preferred pricing plan and provide your details to register for an account.
- Process the payment. Use your Visa or Mastercard or PayPal account to complete the transaction.
- Select the file format and download the form onto your device.
Form popularity
FAQ
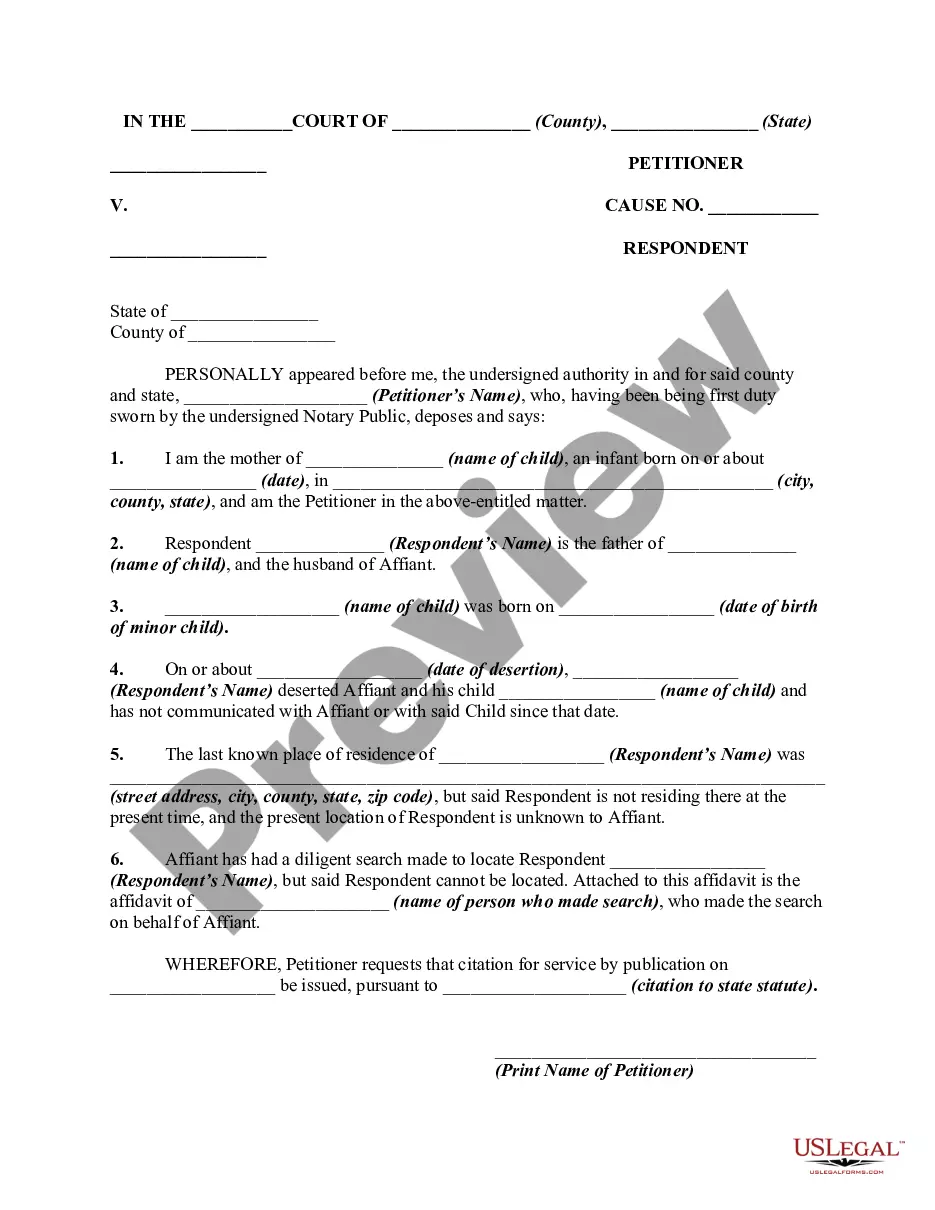
COBRA insurance in Tennessee provides individuals and their families with the option to continue health coverage after losing their job. Under the Tennessee Summary of Rights and Obligations under COBRA, eligible individuals can elect to maintain their group health insurance for a limited time, typically 18 months, following qualifying events such as job loss or reduced work hours. It is important to notify your employer promptly to ensure you receive your COBRA benefits in a timely manner. For those looking to understand their rights better, uslegalforms offers resources to guide you through the process effectively.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
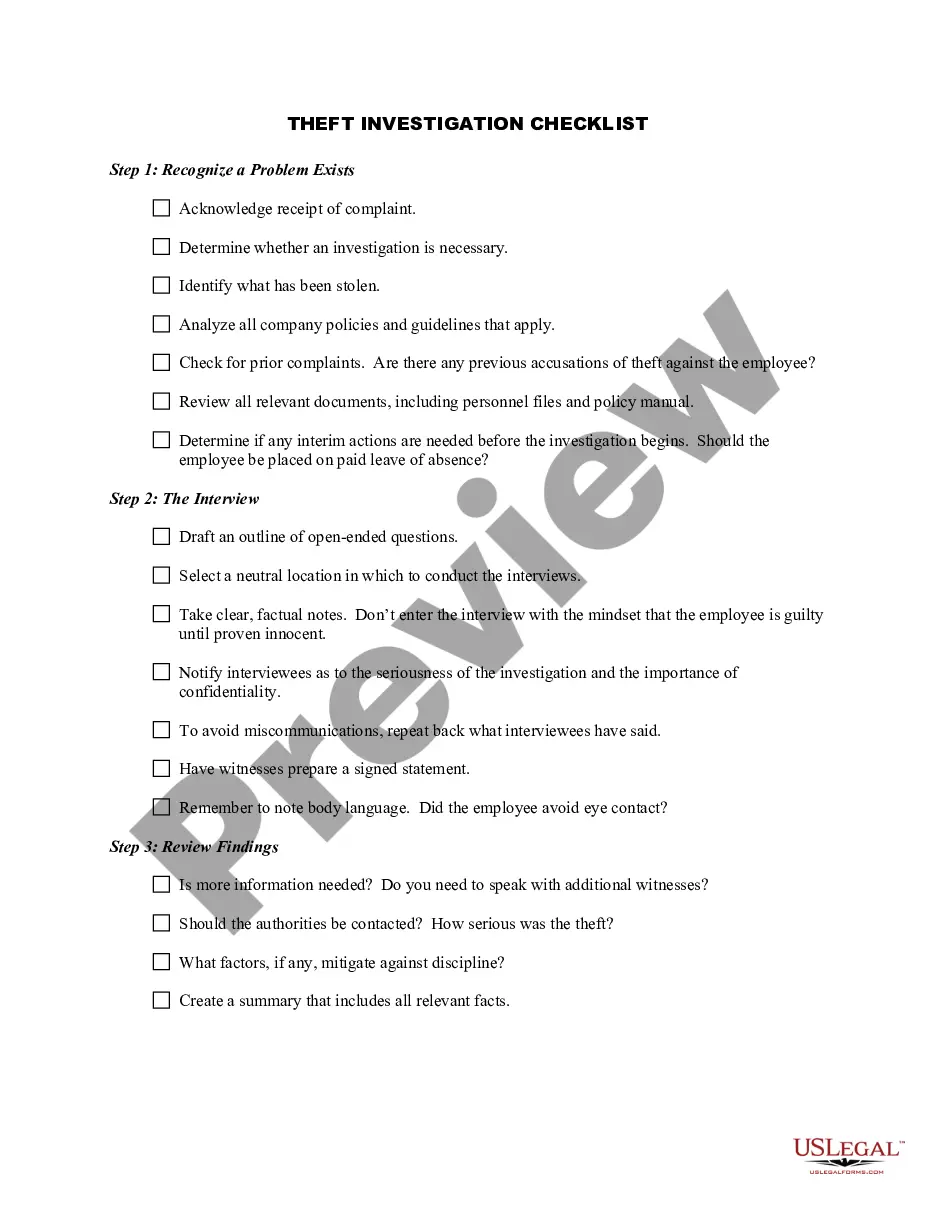
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Through COBRA, individuals pay the entire monthly premium plus a two percent administrative fee, and may be able to remain insured with their health plan for up to 18, 29, or 36 months. All COBRA benefit questions should be directed to Benefits Administration at 615.741.
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.