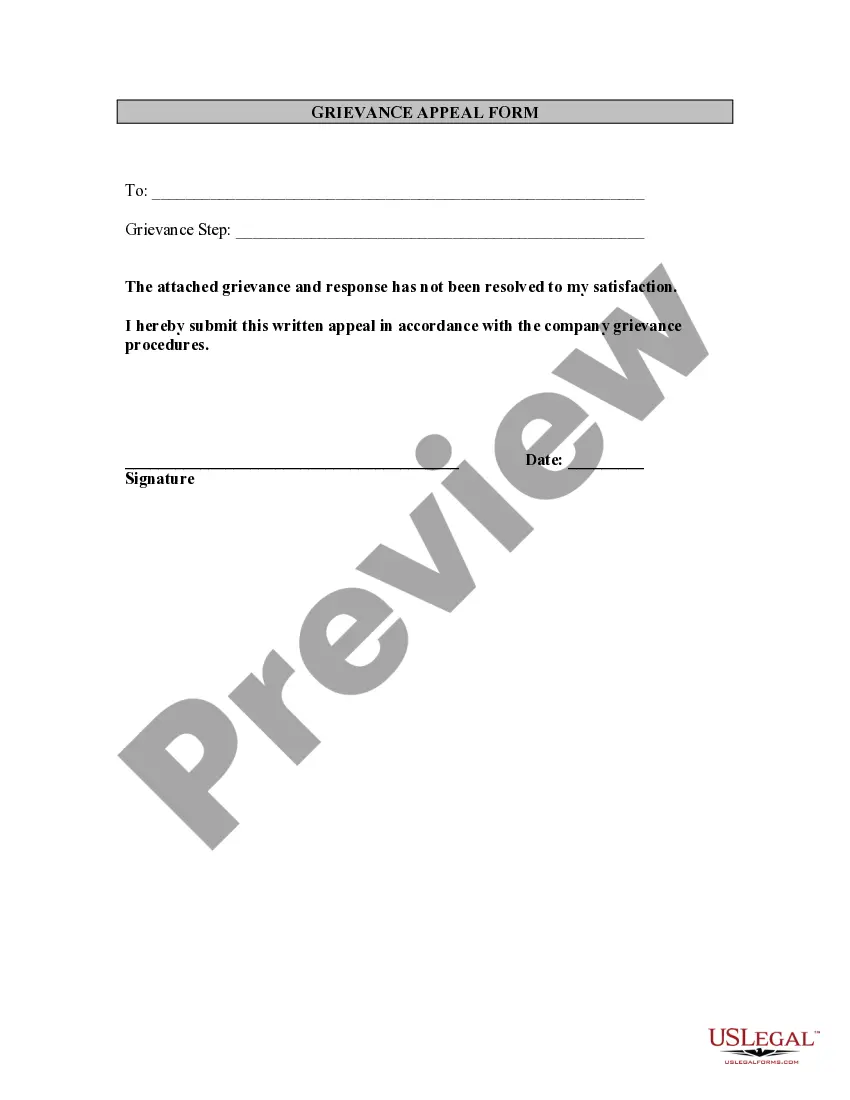
Pennsylvania Employee Grievance Appeal Form
Description
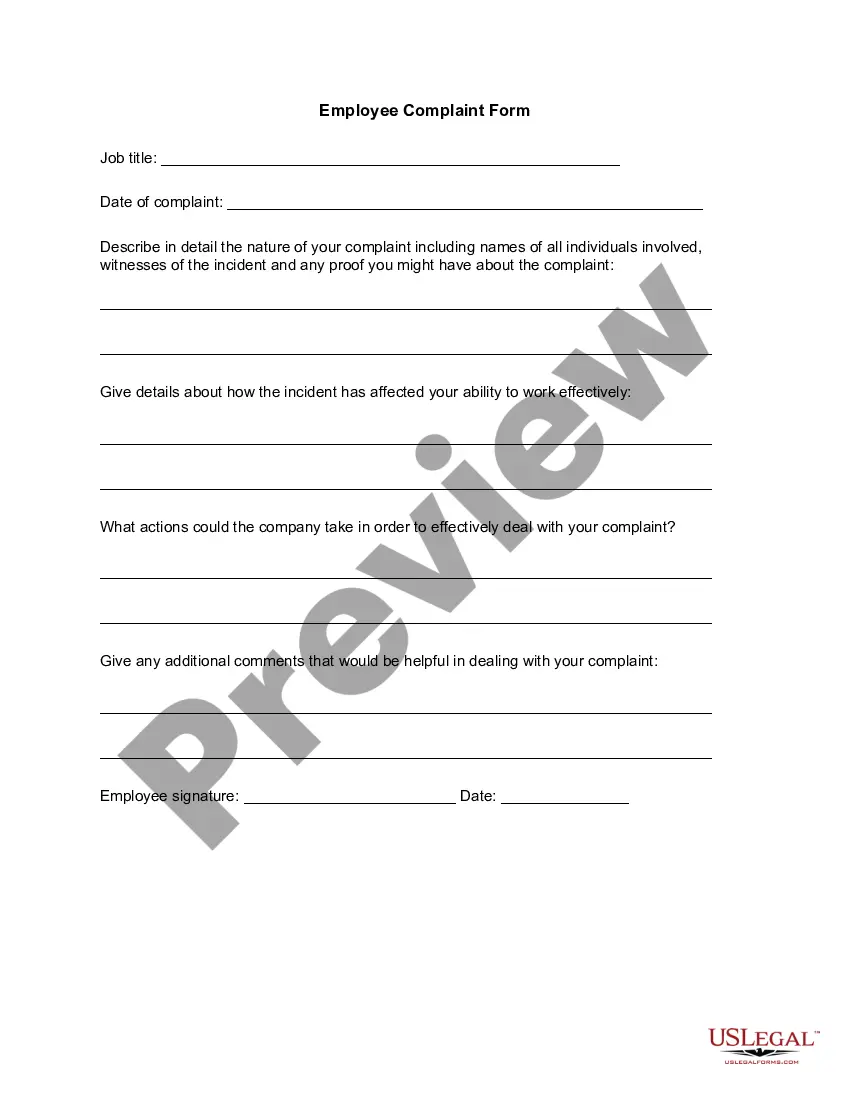
How to fill out Employee Grievance Appeal Form?
Are you presently in a position where you require documents for either business or personal purposes almost all the time.
There are numerous legal document templates available online, but finding reliable ones is challenging.
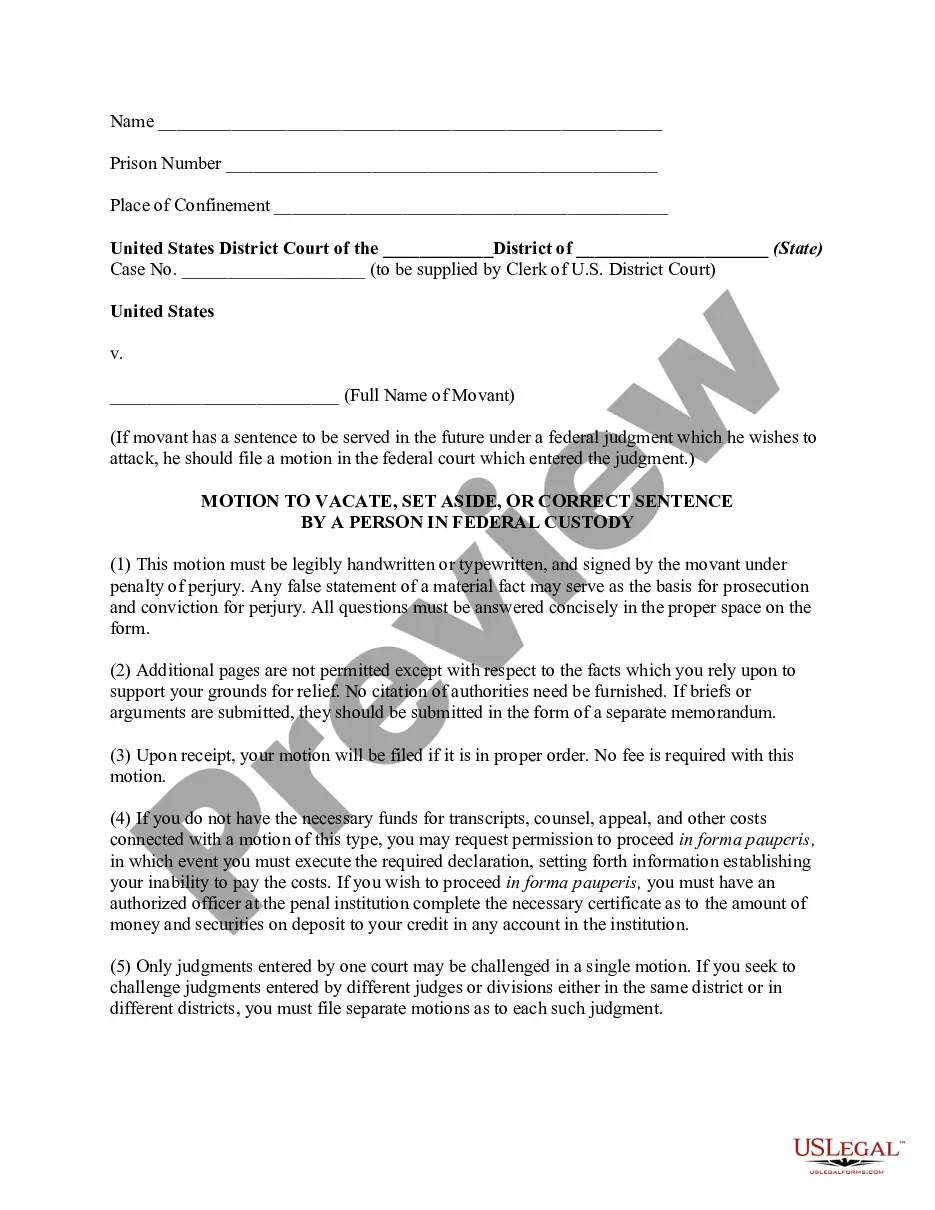
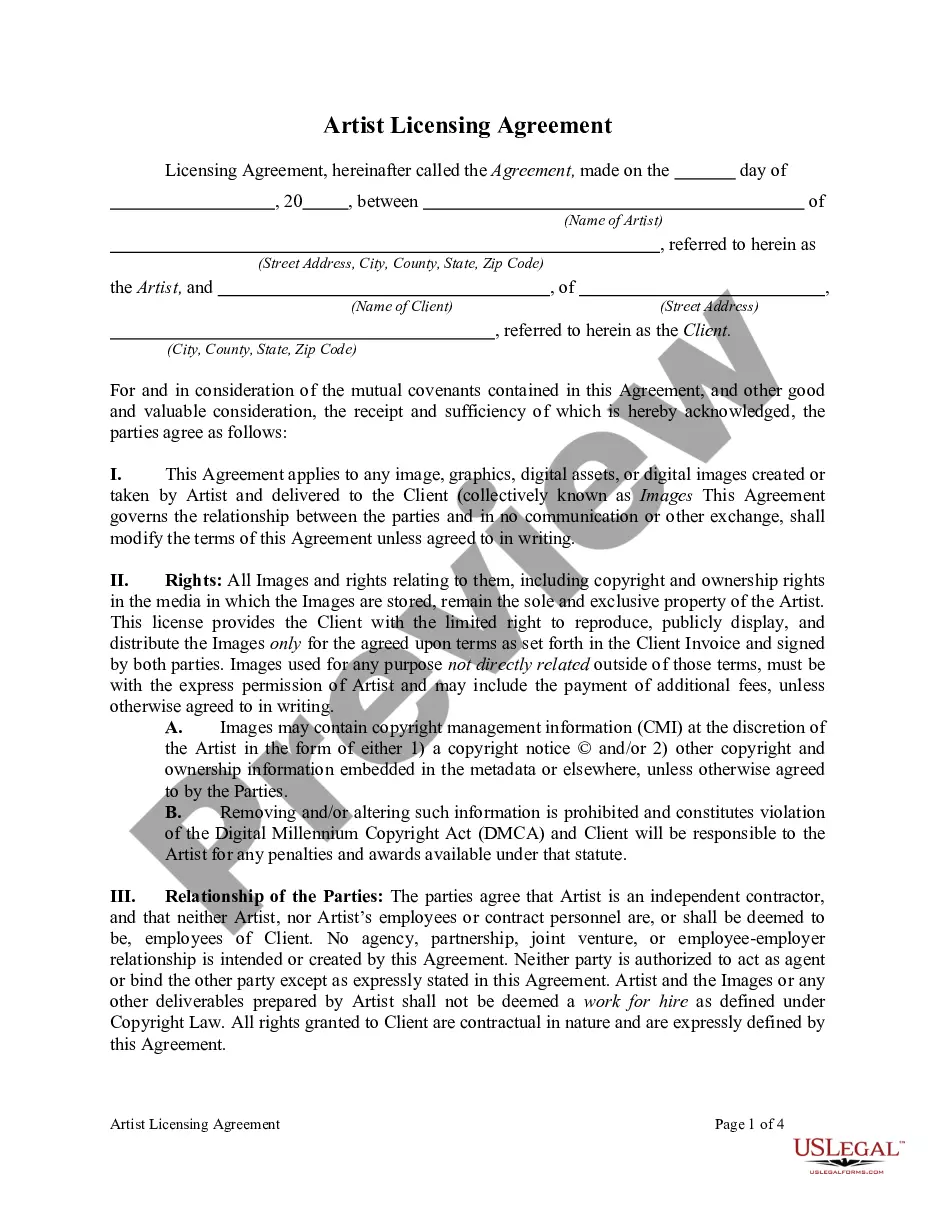
US Legal Forms offers thousands of form templates, including the Pennsylvania Employee Grievance Appeal Form, which are designed to comply with federal and state regulations.
Once you find the correct form, click Purchase now.
Select your desired pricing plan, complete the necessary information to set up your payment, and pay for the transaction using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and possess an account, simply Log In.
- Next, you can download the Pennsylvania Employee Grievance Appeal Form template.
- If you don’t have an account and want to start using US Legal Forms, follow these instructions.
- Acquire the form you need and ensure it is for the correct city/state.
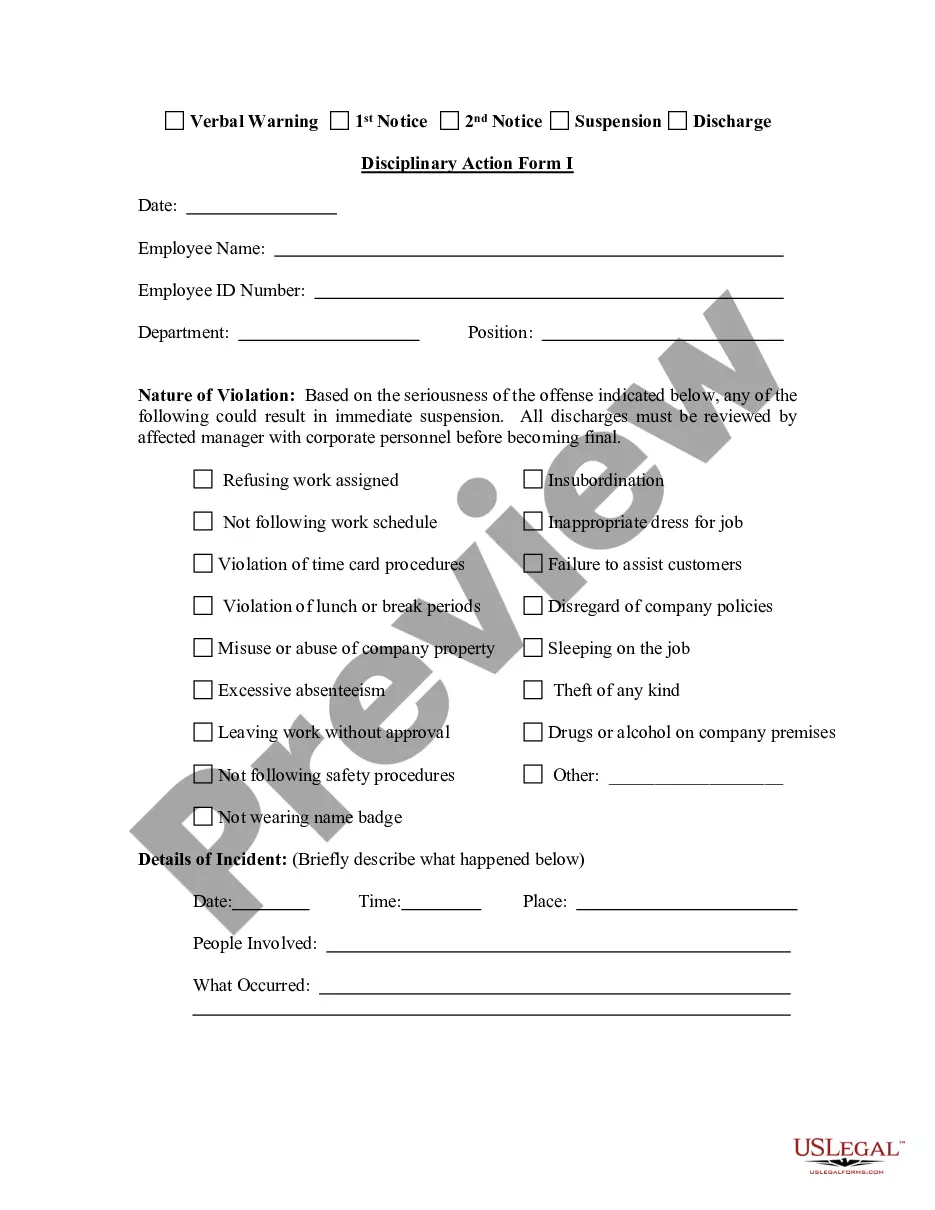
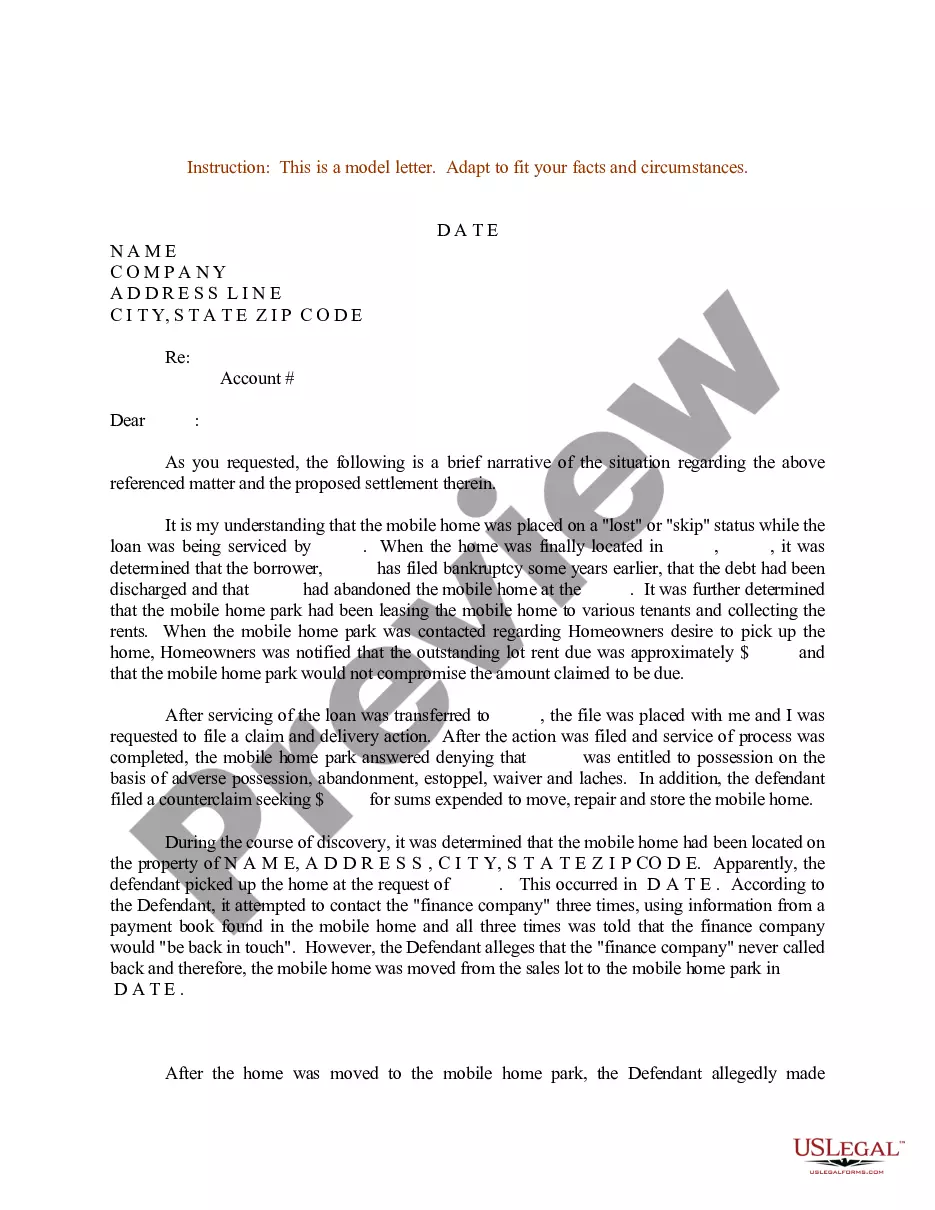
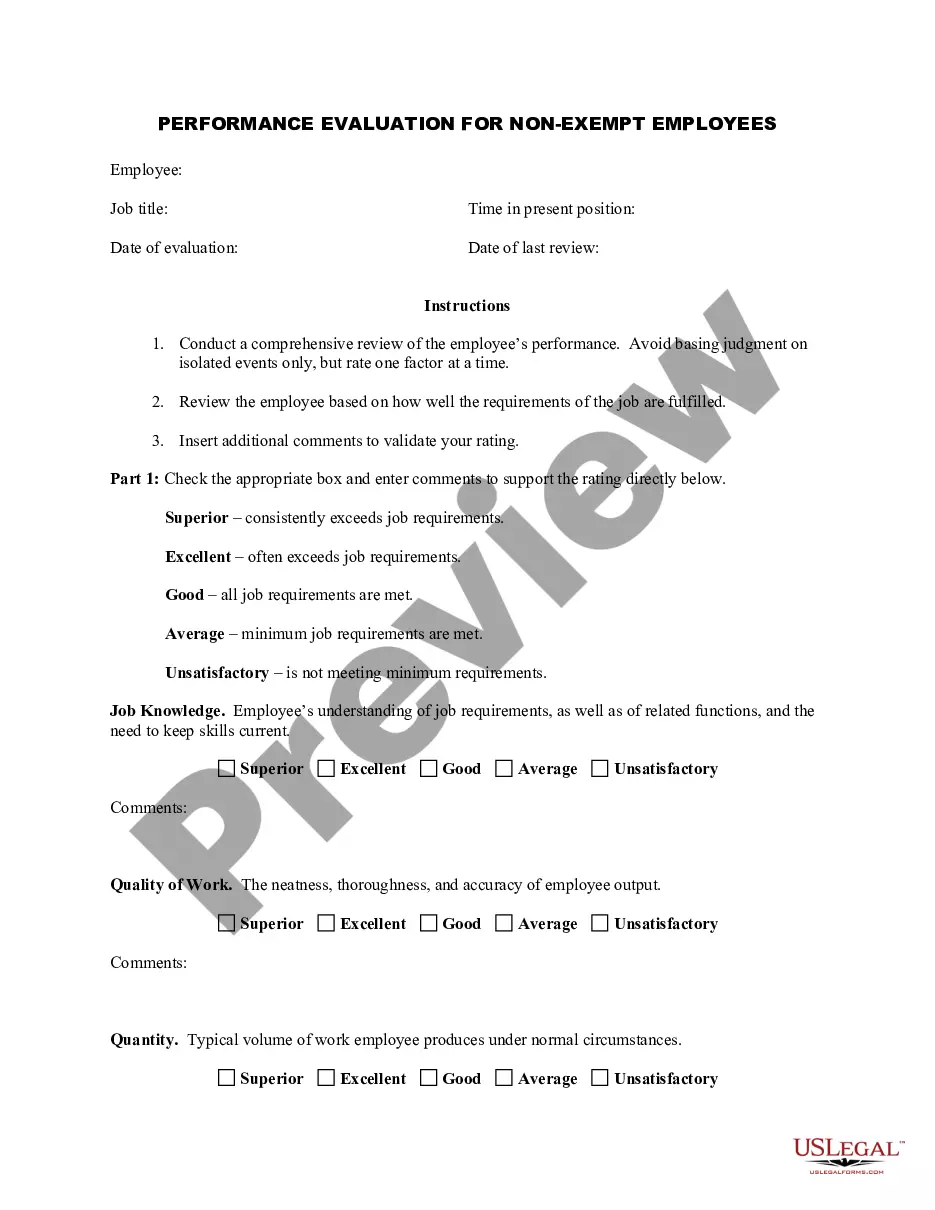
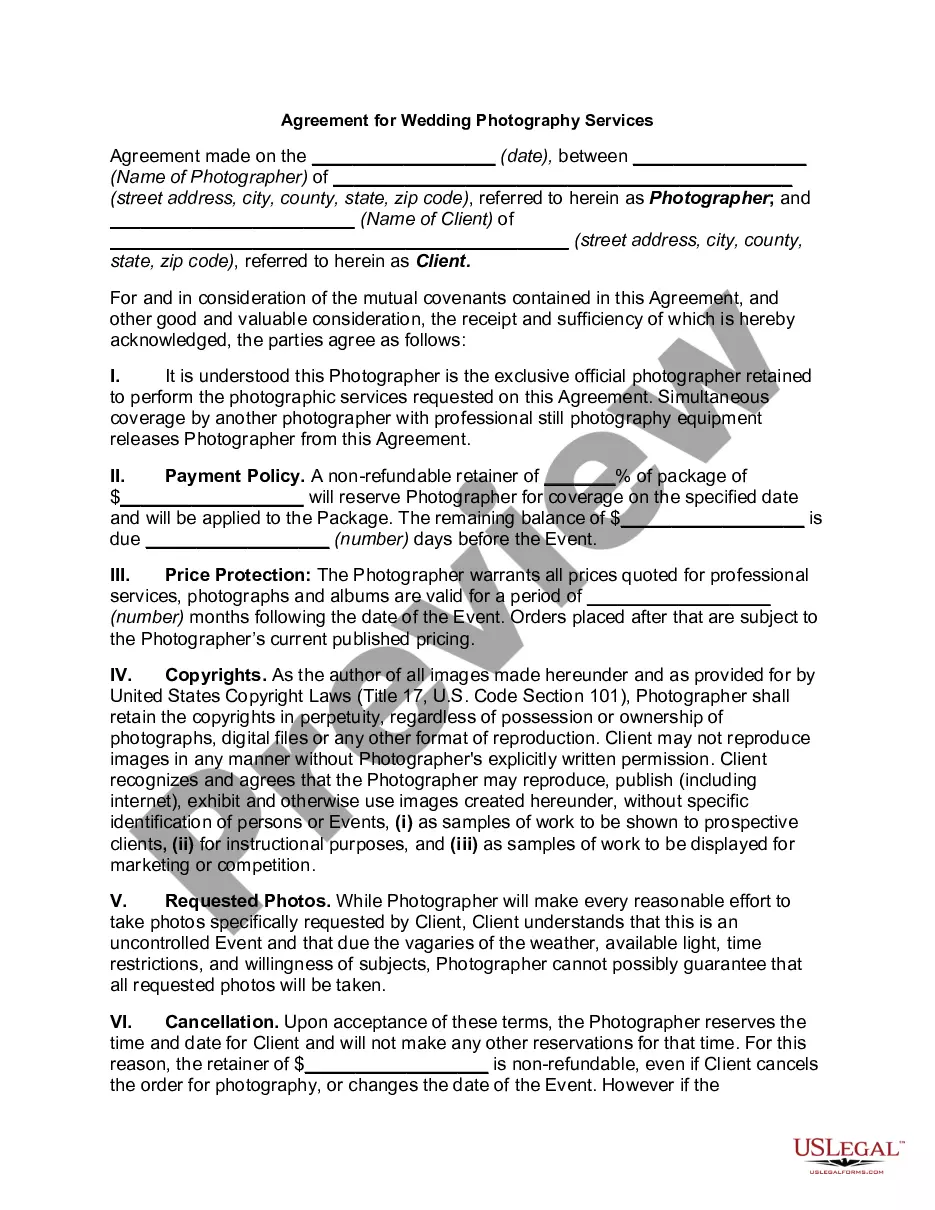
- Utilize the Review button to examine the form.
- Check the summary to confirm that you have chosen the right form.
- If the form does not meet your expectations, use the Search field to find the form that fits your needs.
Form popularity
FAQ
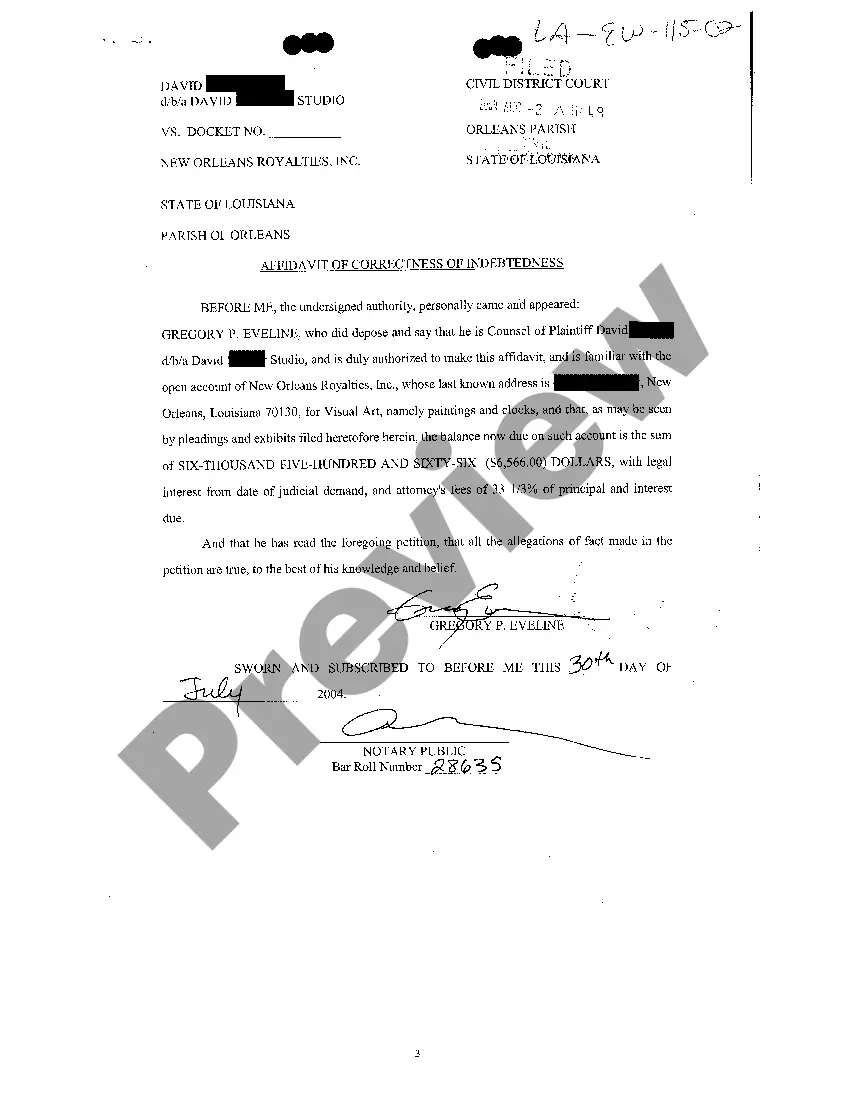
Grievance: Concerns that do not involve an initial determination (i.e. Accessibility/Timeliness of appointments, Quality of Service, MA Staff, etc.) Appeal: Written disputes or concerns about initial determinations; primarily concerns related to denial of services or payment for services.
To consider a communication as escalation of grievance, the subscriber should clearly mention that he/she has raised the grievance with the concerned intermediary and the intermediary has not resolved the grievance within the stipulated time or the grievant is not satisfied with the resolution of the grievance given by
Mail your request: To submit a Clinical Provider Appeal, use the following contact information. Fax your request for all member appeals or grievances to 1-833-841-8075. All Medicaid Providers, use 1-833-841-8075.
The Appeals & Grievance Coordinator is responsible for the day to day functions of the tracking and trending of all grievances, appeals, and complaints received within the Member Services Department. The coordinator will act as the primary investigator and contact person for member and provider grievances and appeals.
A grievance is an expression of dissatisfaction (other than an organization determination) with any aspect of the operations, activities, or behavior of a Medicare health plan, or its providers, regardless of whether remedial action is requested.
Highmark Blue Shield's claim processing system places a higher priority on claims filed electronically. Electronic claims will typically process in 7 to 14 calendar days, whereas paper claims will process in 21 to 27 calendar days.
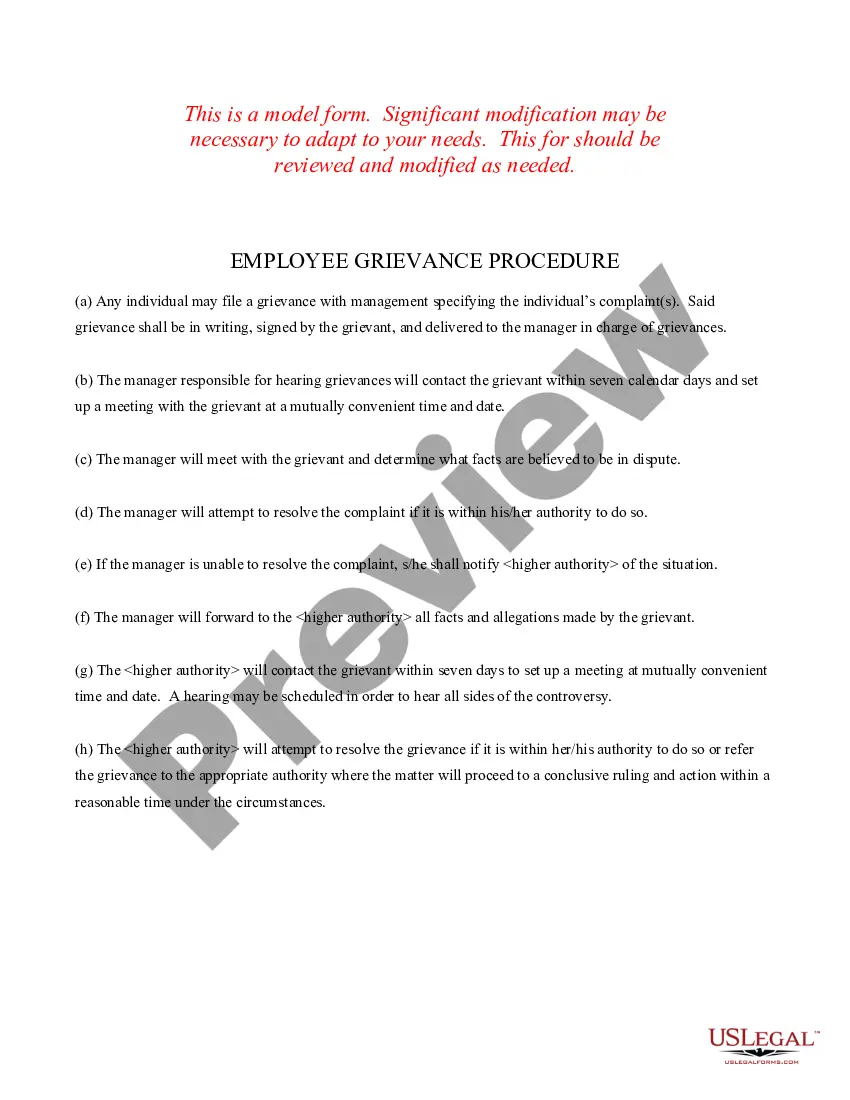
Providers must understand The Health Plan grievance system in order to assist members who wish to utilize a grievance system process....Specifically, The Health Plan adheres to the following grievance resolution process:Acknowledgement.Communication and Information.Resolution.Decision making.
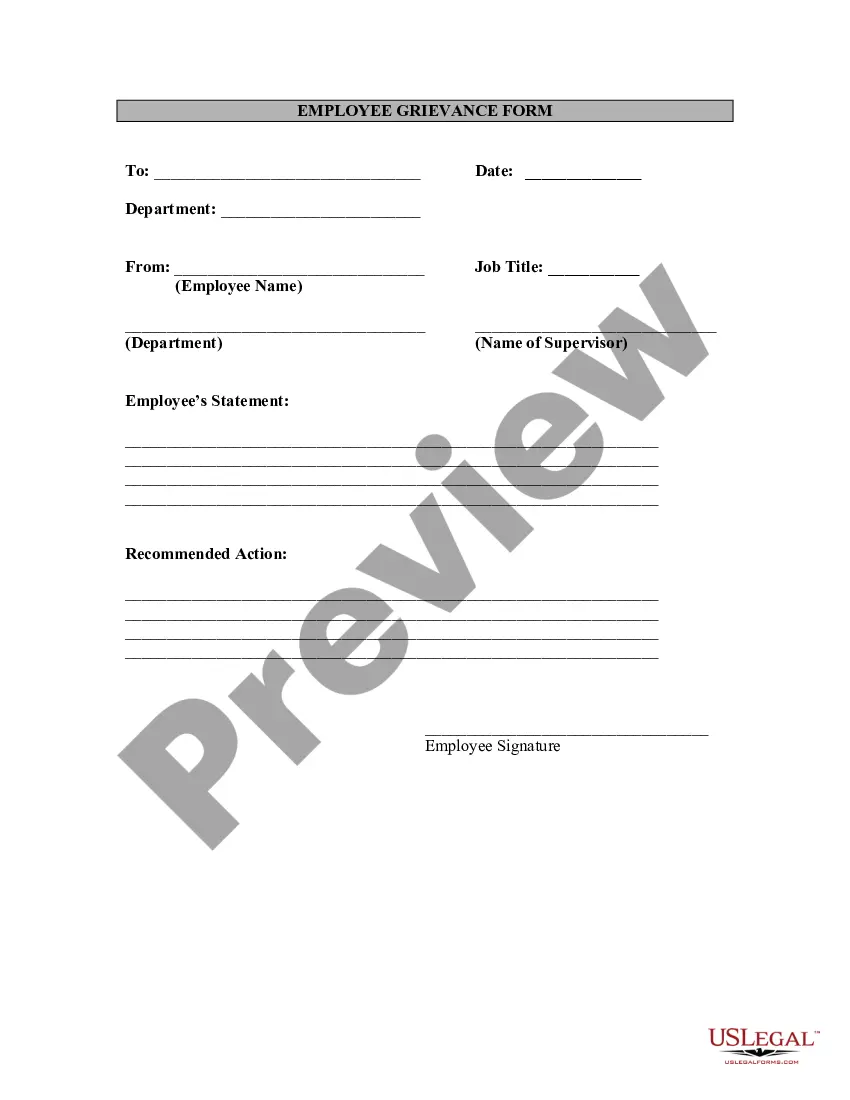
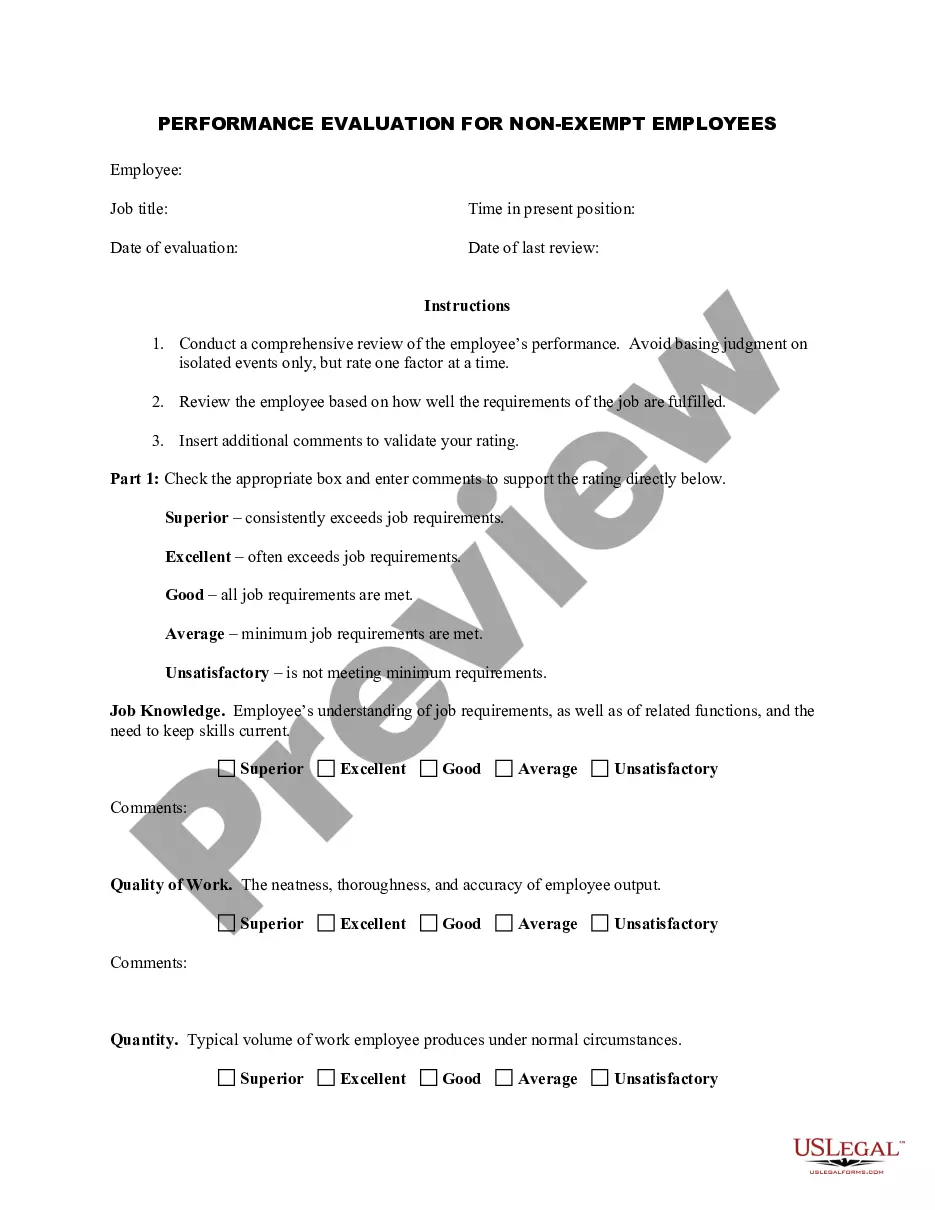
Appeal & Grievance FormThis form is for your use in making suggestions, filing a formal complaint, or appeal regarding any aspect of the care or service provided to you. Your health plan is required by law to respond to your complaints or appeals, and a detailed procedure exists for resolving these situations.
Formal Stage 2 Hearing The Chair should explain the process of the hearing and confirm that this is the final stage in the Grievance Policy. The hearing may be adjourned at the discretion of the Chair to enable further evidence to be produced by either party, or any other reason.
Per the timely filing policy, any claim not received within 365 days of the last date of service will be denied for untimeliness. This policy applies to all Highmark Blue Shield providers.