Ohio Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights
Description
How to fill out Certificate Of Group Health Plan Coverage With Statement Of HIPAA Portability Rights?
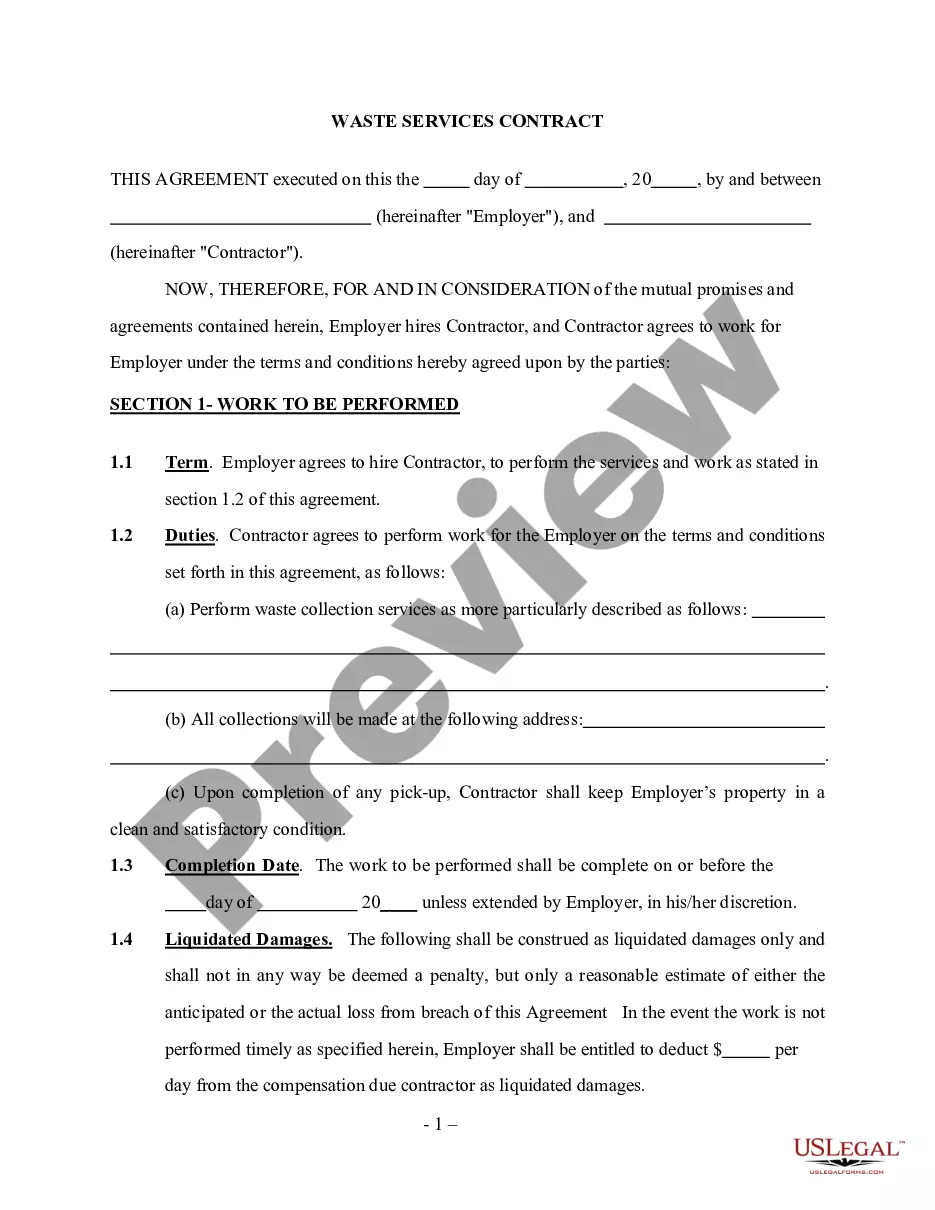
Are you presently within a position that you need to have files for possibly enterprise or individual functions virtually every working day? There are tons of legitimate file layouts available online, but finding versions you can trust isn`t effortless. US Legal Forms offers thousands of type layouts, like the Ohio Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights, which are published in order to meet federal and state needs.
If you are presently acquainted with US Legal Forms website and get a merchant account, simply log in. Next, you can obtain the Ohio Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights format.
Unless you have an account and would like to start using US Legal Forms, adopt these measures:
- Obtain the type you need and ensure it is for the proper city/region.
- Take advantage of the Preview key to check the shape.
- See the outline to actually have chosen the proper type.
- If the type isn`t what you are seeking, make use of the Look for industry to discover the type that meets your requirements and needs.
- When you find the proper type, simply click Buy now.
- Select the rates program you want, fill out the specified info to make your money, and buy your order with your PayPal or Visa or Mastercard.
- Select a practical data file format and obtain your duplicate.
Get every one of the file layouts you possess purchased in the My Forms menus. You may get a further duplicate of Ohio Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights any time, if necessary. Just go through the essential type to obtain or printing the file format.
Use US Legal Forms, probably the most substantial variety of legitimate kinds, to save efforts and prevent mistakes. The assistance offers appropriately manufactured legitimate file layouts which can be used for an array of functions. Create a merchant account on US Legal Forms and begin producing your daily life easier.
Form popularity
FAQ
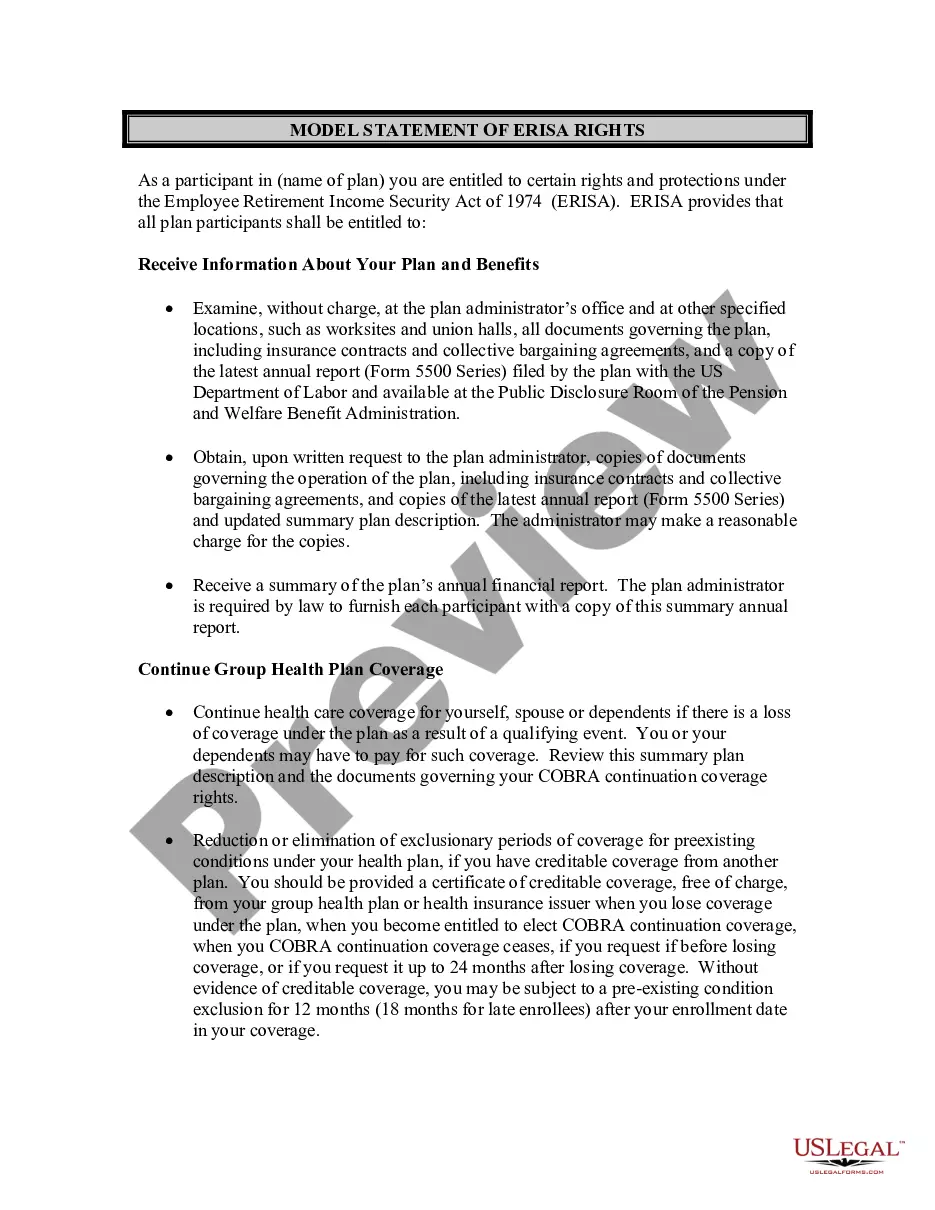
As a recap, all plans that self-insure, have fewer than 50 participants and are internally administered, are exempt from the privacy rule.
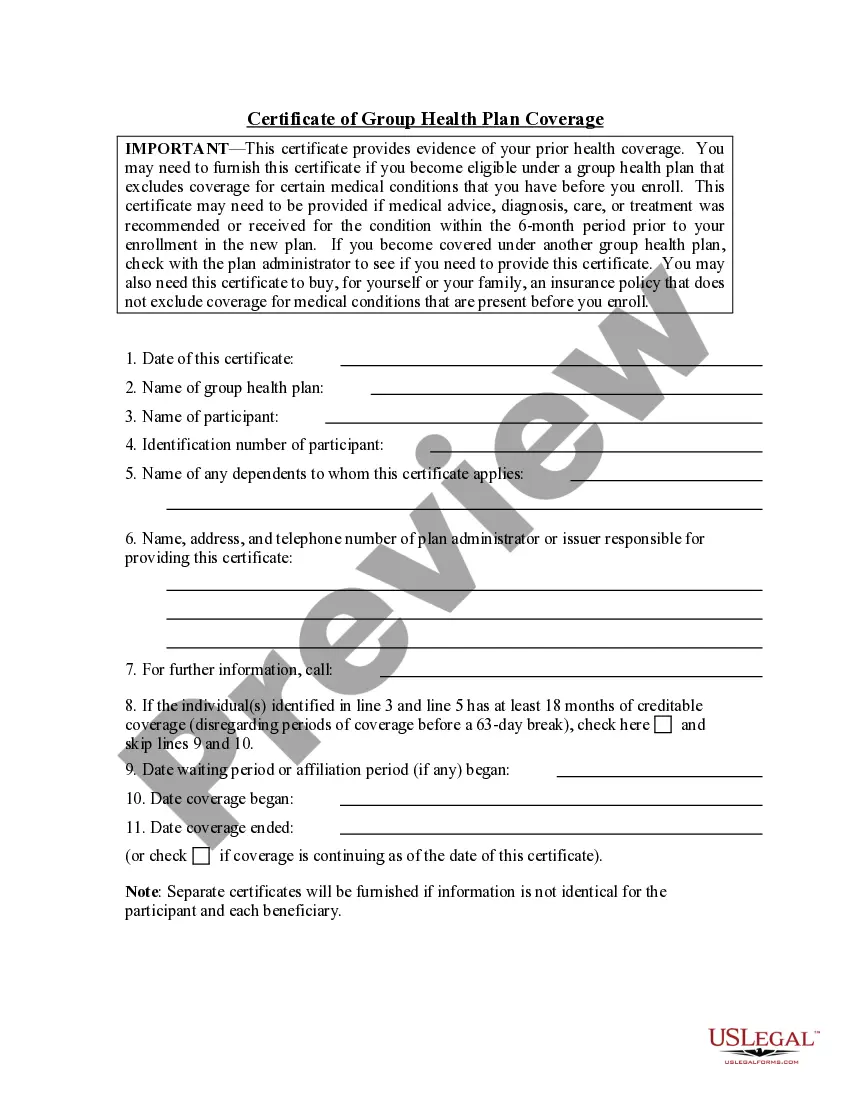
This is a letter that says how long you have been covered and provides proof that you have had at least 18 months of coverage. If you are unable to provide a Certificate of Creditable Coverage, you can talk to the health plan about other ways you can prove that you had a least 18 months of coverage.
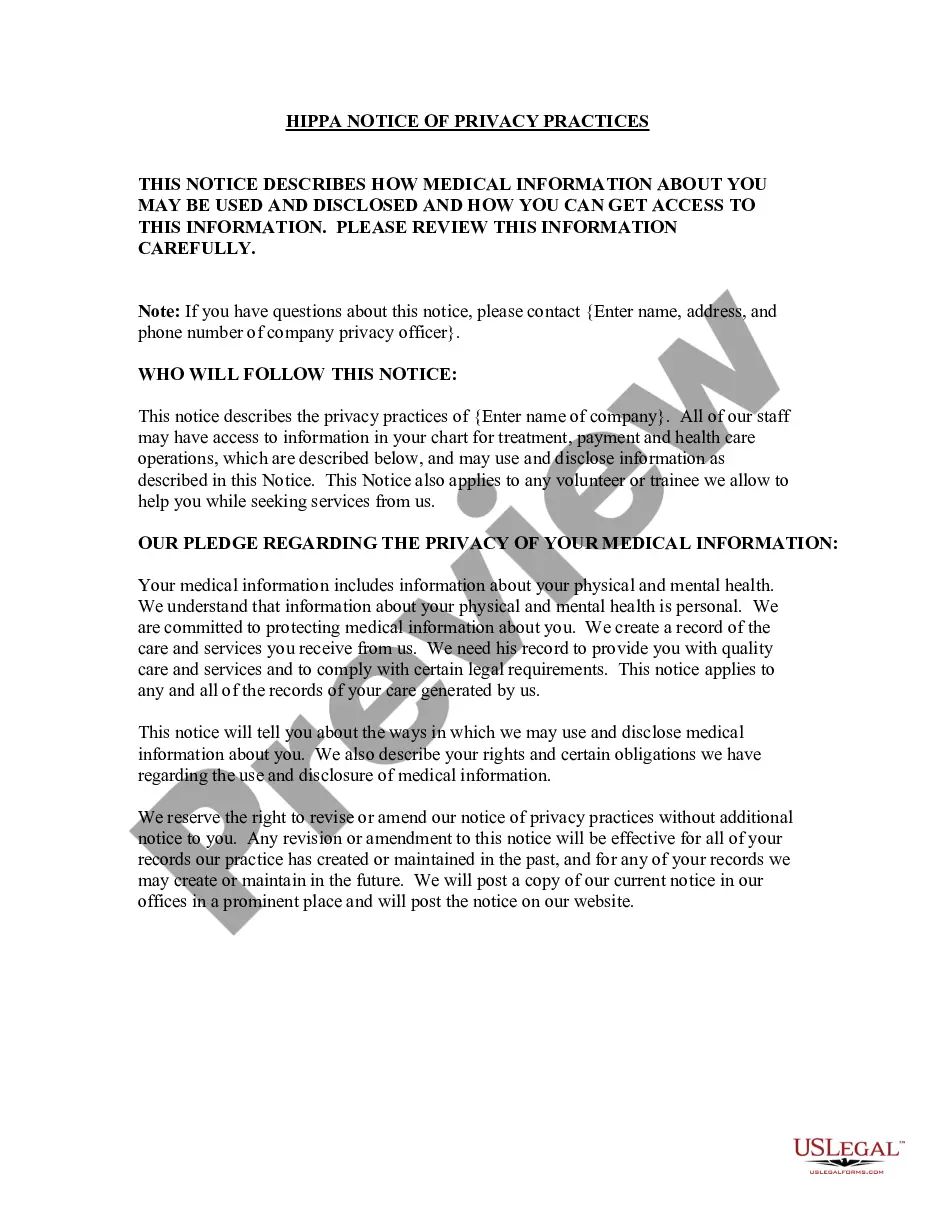
What is a Non-Covered Entity Under HIPAA? As mentioned above, a non-covered entity is an entity that is not subject to the requirements of the HIPAA Privacy Rule. There are two types of non-covered entities under HIPAA: business associates and hybrid entities.
The HIPAA certificate, also known as certificate of creditable coverage, documents the health coverage you had before you lost coverage. If you had less than 18 months of continuous coverage, the certificate includes the dates any waiting period began and when coverage began and ended.
The definition of ?group health plan? is adopted from the statutory definition at section 1171(5)(A), and excludes from the rule as ?health plans? only the few insured or self-insured ERISA plans that have less than 50 participants and are self administered.
ANSWER: A health plan with fewer than 50 participants that is administered by the sponsoring employer is excluded from the definition of a ?group health plan? under HIPAA's administrative simplification provisions, which include the privacy and security requirements.
HIPAA's "portability" protection means that once a person obtains creditable health plan coverage, he or she can use evidence of that coverage to reduce or eliminate any preexisting medical condition exclusion period that might otherwise be imposed when moving to another health plan.
Exceptions to the HIPAA Privacy Rule Limitations apply to uses and disclosures for the purpose of facilitating another party's activities. Exceptions are allowed for a covered entity to disclose PHI to: Any other provider (even a non-covered entity) to facilitate that provider's treatment activities.