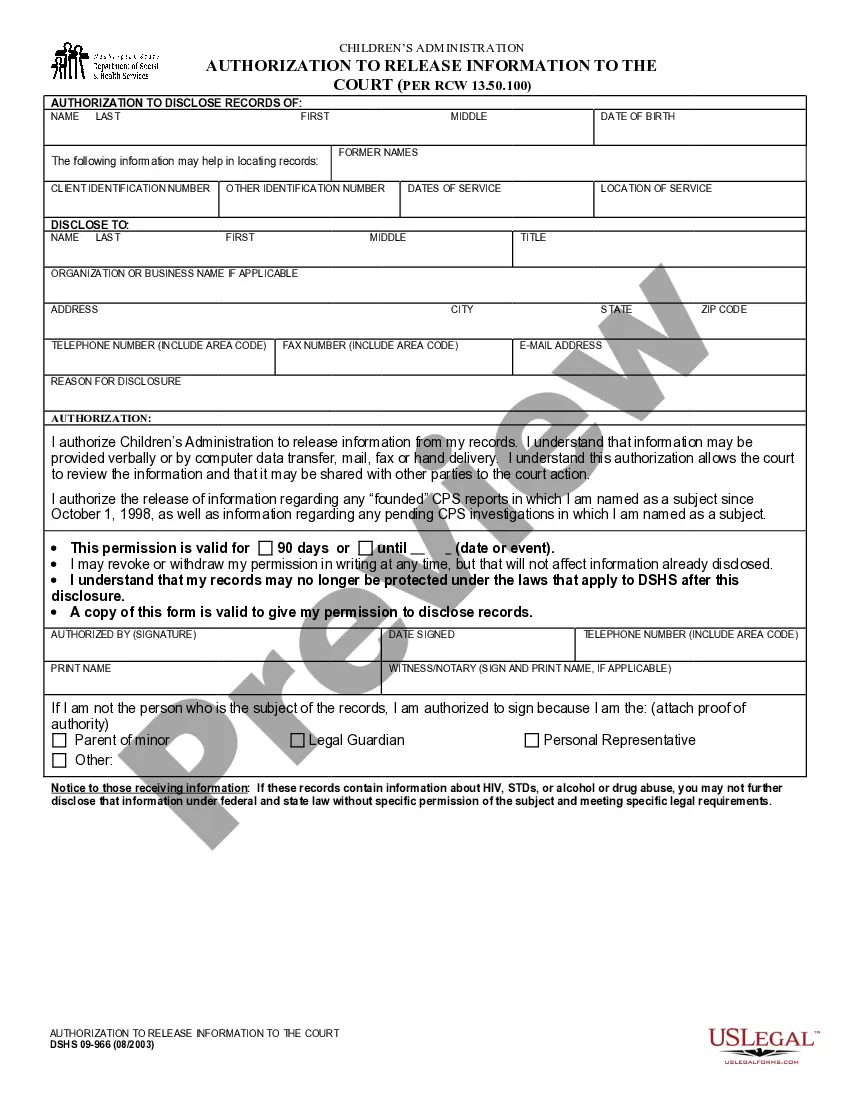
The Ohio Request For Prior Authorization of Non-Preferred Medication Form is a document used by healthcare providers in the state of Ohio to request authorization for the use of a non-preferred medication in the treatment of a patient. The form includes sections for the patient's medical history and diagnosis, as well as a detailed description of the proposed treatment plan with the non-preferred medication. The form also requires the prescriber to provide supporting documentation, such as laboratory results, to support the request. The Ohio Department of Medicaid reviews the completed form and makes a determination regarding the authorization of the requested medication. The Ohio Request For Prior Authorization of Non-Preferred Medication Form is available in two different forms: the Standard Form and the Specialty Form. The Standard Form is used for most non-preferred medications, while the Specialty Form is used for certain specialty medications that require additional information.
Ohio Request For Prior Authorization of Non-Preferred Medication Form
Description
How to fill out Ohio Request For Prior Authorization Of Non-Preferred Medication Form?
US Legal Forms is the most simple and profitable way to find suitable legal templates. It’s the most extensive online library of business and individual legal paperwork drafted and checked by legal professionals. Here, you can find printable and fillable templates that comply with national and local regulations - just like your Ohio Request For Prior Authorization of Non-Preferred Medication Form.
Getting your template takes only a few simple steps. Users that already have an account with a valid subscription only need to log in to the website and download the document on their device. Afterwards, they can find it in their profile in the My Forms tab.
And here’s how you can obtain a properly drafted Ohio Request For Prior Authorization of Non-Preferred Medication Form if you are using US Legal Forms for the first time:
- Read the form description or preview the document to ensure you’ve found the one corresponding to your requirements, or find another one using the search tab above.
- Click Buy now when you’re certain about its compatibility with all the requirements, and select the subscription plan you prefer most.
- Create an account with our service, log in, and pay for your subscription using PayPal or you credit card.
- Decide on the preferred file format for your Ohio Request For Prior Authorization of Non-Preferred Medication Form and save it on your device with the appropriate button.
Once you save a template, you can reaccess it whenever you want - simply find it in your profile, re-download it for printing and manual completion or upload it to an online editor to fill it out and sign more proficiently.
Benefit from US Legal Forms, your reliable assistant in obtaining the corresponding formal documentation. Try it out!
Form popularity
FAQ
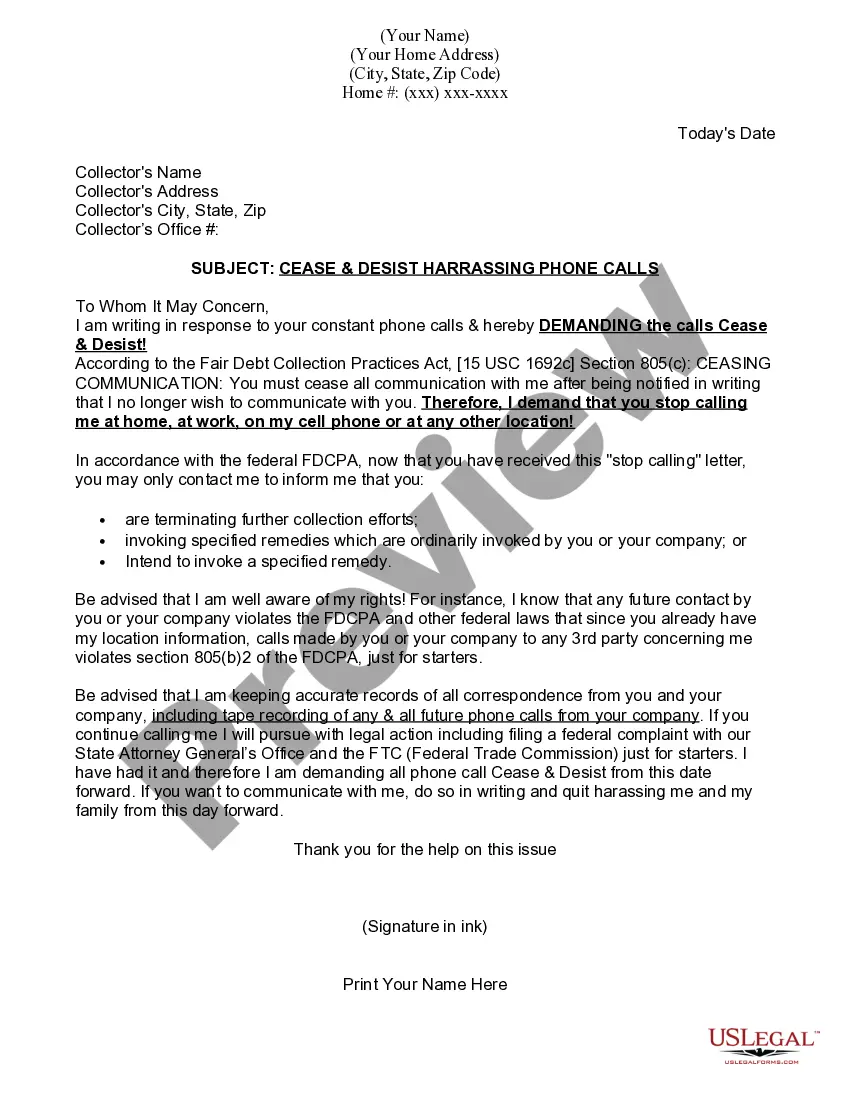
Drug prior authorization is an approval process to ensure that certain medications being prescribed are covered under your benefits plan. You can use the online tool, My drug plan, to look up a drug and find out whether it is covered under your benefits plan or if prior authorization is needed.
This is to ensure that the medication is appropriate for your treatment. It also helps to make sure it's the most cost-effective option. When prior authorization is granted, it is typically for a specific length of time. You will need to request prior authorization again if you need a refill after the timeframe passes.
What is prior authorization? This means we need to review some medications before your plan will cover them. We want to know if the medication is medically necessary and appropriate for your situation. If you don't get prior authorization, a medication may cost you more, or we may not cover it.
Prior Authorizations Under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. Prior authorization is usually required if you need a complex treatment or prescription. Coverage will not happen without it.
The following agents are PREFERRED stimulants (prior authorization not required for any patients age 6 years or older): Amphetamine/dextroamphetamine ER capsules (generics to Adderall XR) Dexmethylphenidate ER capsules (generics to Focalin XR) Dextroamphetamine ER capsules (generics to Dexedrine Spansules)
The prior authorization process begins when a service prescribed by a patient's physician is not covered by their health insurance plan. Communication between the physician's office and the insurance company is necessary to handle the prior authorization.
Drugs That May Require Prior Authorization Drug ClassDrugs in ClassAndrogens-Anabolic SteroidsAndrol-50, Danazol, Nandrolone, OxandrinAnticoagulantsEliquis, Pradaxa, XareltoAntipsoriatic AgentsOtezla, Stelara, Taltz, TremfyaApokyn, KynmobiApokyn, Kynmobi240 more rows
How Does Prior Authorization Work? Call your physician and ensure they have received a call from the pharmacy. Ask the physician (or his staff) how long it will take them to fill out the necessary forms. Call your insurance company and see if they need you to fill out any forms.