New York Notice of Qualifying Event from Employer to Plan Administrator
Description
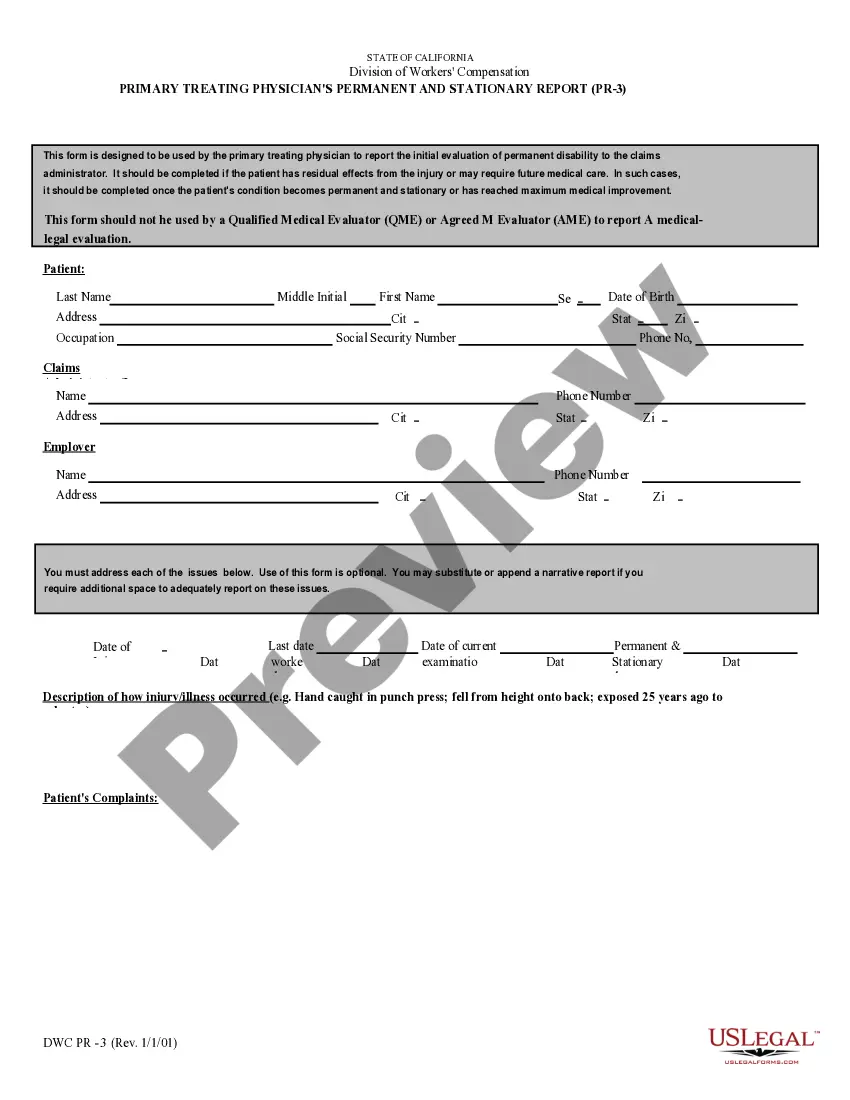
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
You could spend numerous hours online attempting to locate the valid document template that satisfies the state and federal requirements you will need.
US Legal Forms provides a vast array of valid forms that are reviewed by experts.
You can directly download or print the New York Notice of Qualifying Event from Employer to Plan Administrator using your service.
In order to find another variation of the form, utilize the Lookup section to search for the template that aligns with your needs and preferences.
- If you already have a US Legal Forms account, you may Log In and click on the Obtain button.
- After that, you can complete, edit, print, or sign the New York Notice of Qualifying Event from Employer to Plan Administrator.
- Every valid document template you acquire remains your property indefinitely.
- To retrieve another copy of the purchased form, navigate to the My documents tab and click the corresponding button.
- If this is your first time using the US Legal Forms site, follow the simple instructions provided below.
- First and foremost, ensure that you have selected the correct document template for the region/area of your choice.
- Read the form description to confirm that you have chosen the appropriate form.
Form popularity
FAQ
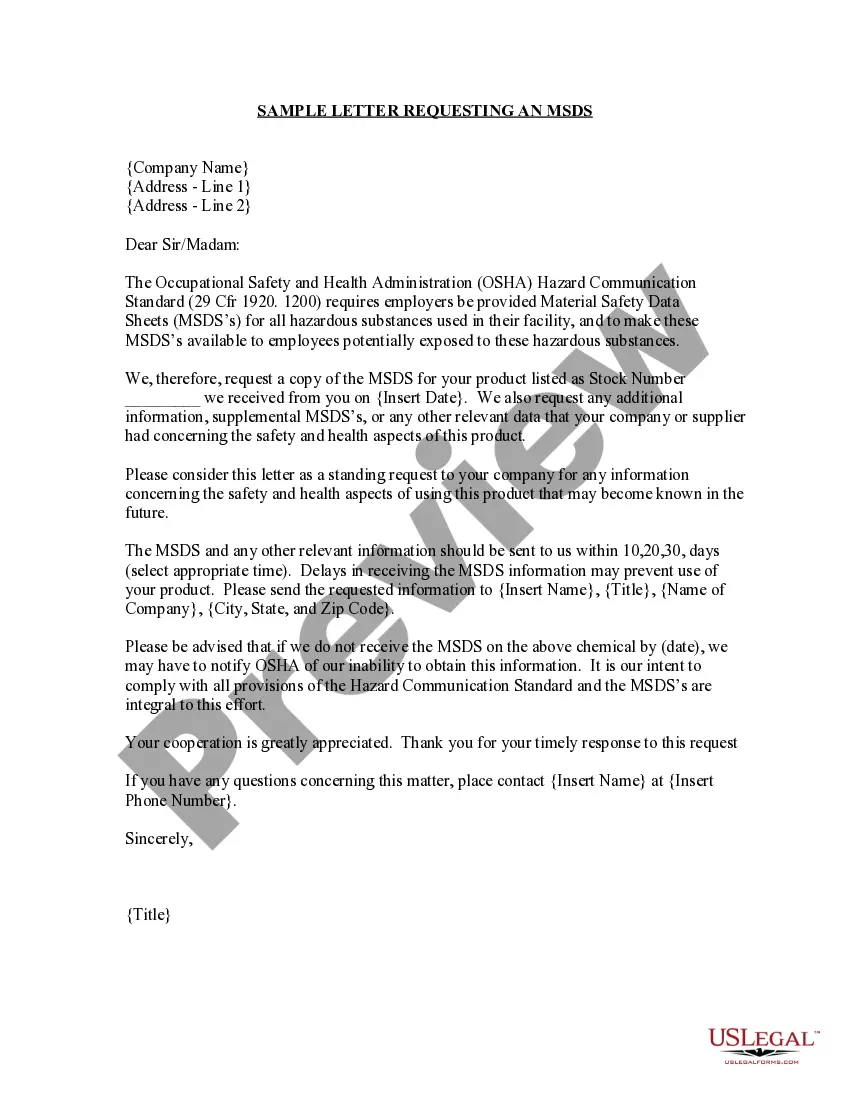
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
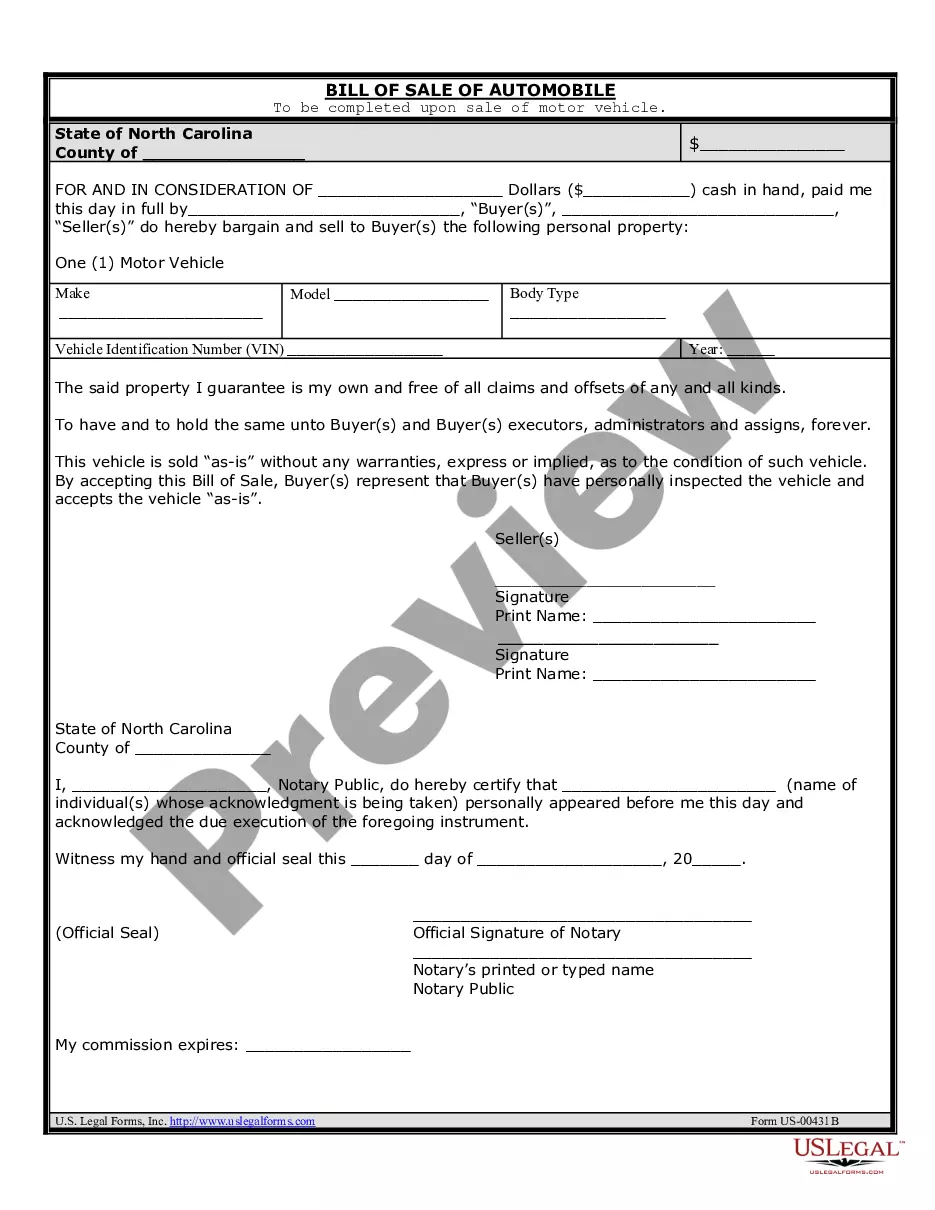
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
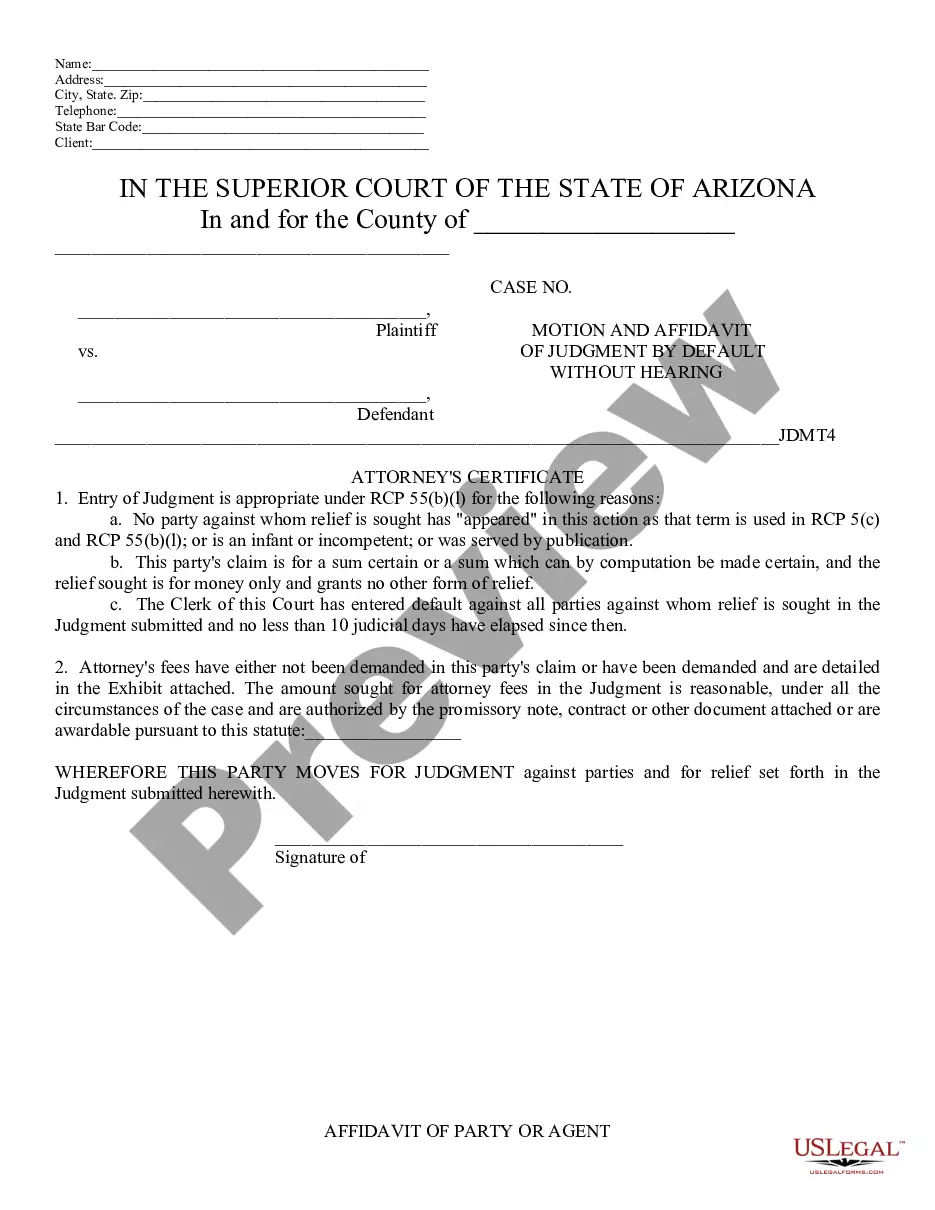
DOL ERISA Penalties An employer is liable up to an additional $110 per day per participant if they fail to provide initial COBRA notices. ERISA can also hold any fiduciary personally liable for non-compliance.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
Employers do not have to offer COBRA coverage to: Employees who are not yet eligible for a group health plan. Eligible employees who declined to participate in a group health plan. Individuals who are enrolled for benefits under Medicare.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
There is no state law requiring employers to offer group healthcare insurance to their employees, but most employers do provide this benefit. However, if health insurance is offered, New York's insurance laws require policies to cover certain specified services (mandated benefits).
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under