Nevada Model COBRA Continuation Coverage Election Notice
Description
How to fill out Model COBRA Continuation Coverage Election Notice?
Selecting the optimal legal document template can be challenging. Naturally, there is a multitude of templates accessible online, but how will you locate the legal form you require? Utilize the US Legal Forms website. The service offers a plethora of templates, including the Nevada Model COBRA Continuation Coverage Election Notice, which can be utilized for business and personal purposes. All of the forms are reviewed by experts and comply with state and federal regulations.
If you are already registered, Log In to your account and then click the Download button to acquire the Nevada Model COBRA Continuation Coverage Election Notice. Use your account to search through the legal documents you have purchased previously. Navigate to the My documents section of your account and obtain another copy of the documents you need.
If you are a new user of US Legal Forms, here are basic steps you should follow: First, ensure you have selected the correct form for your city/state. You can review the form using the Preview button and read the form description to confirm it is appropriate for you. If the form does not meet your needs, utilize the Search box to find the correct form.
- Once you are confident the form is suitable, click the Buy Now button to obtain the document.
- Select the pricing plan you desire and input the required details.
- Create your account and complete the order using your PayPal account or credit card.
- Choose the file format and download the legal document template to your device.
- Fill out, edit, print, and sign the received Nevada Model COBRA Continuation Coverage Election Notice.
- US Legal Forms is the largest collection of legal forms from which you can find a variety of document templates. Utilize the service to obtain expertly crafted documents that comply with state regulations.
Form popularity
FAQ
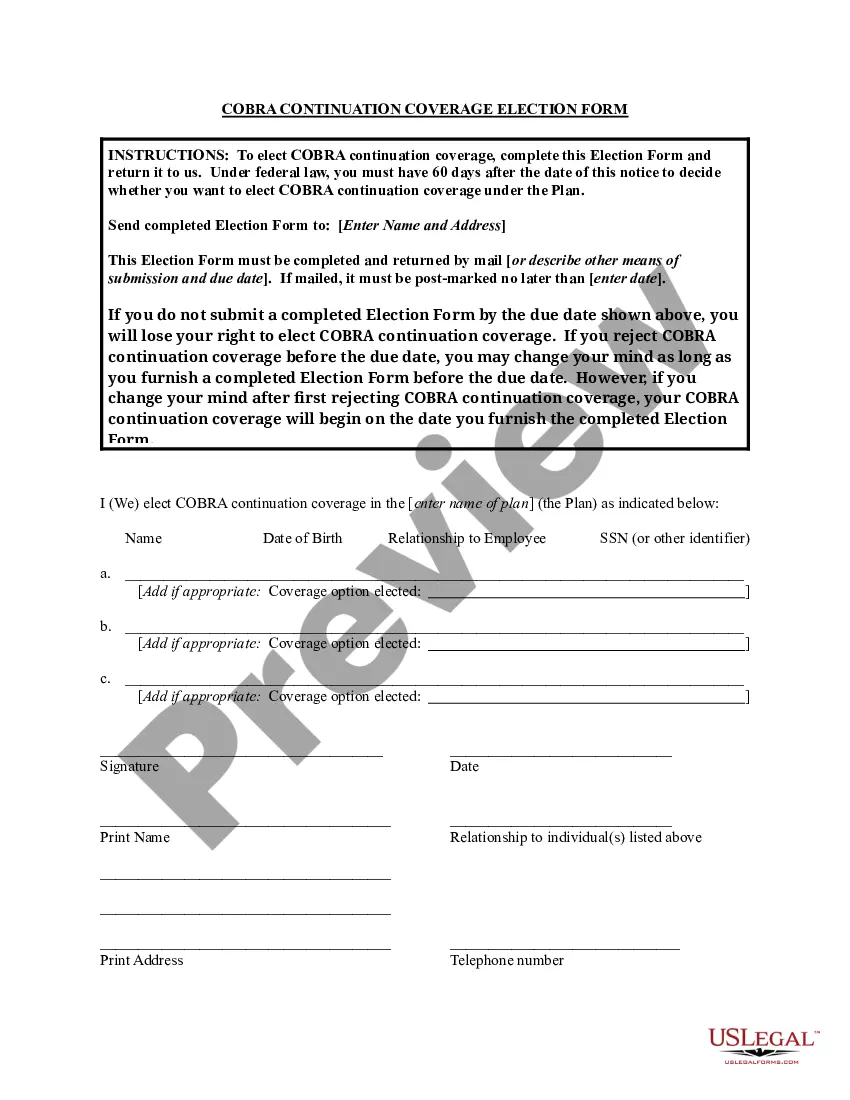
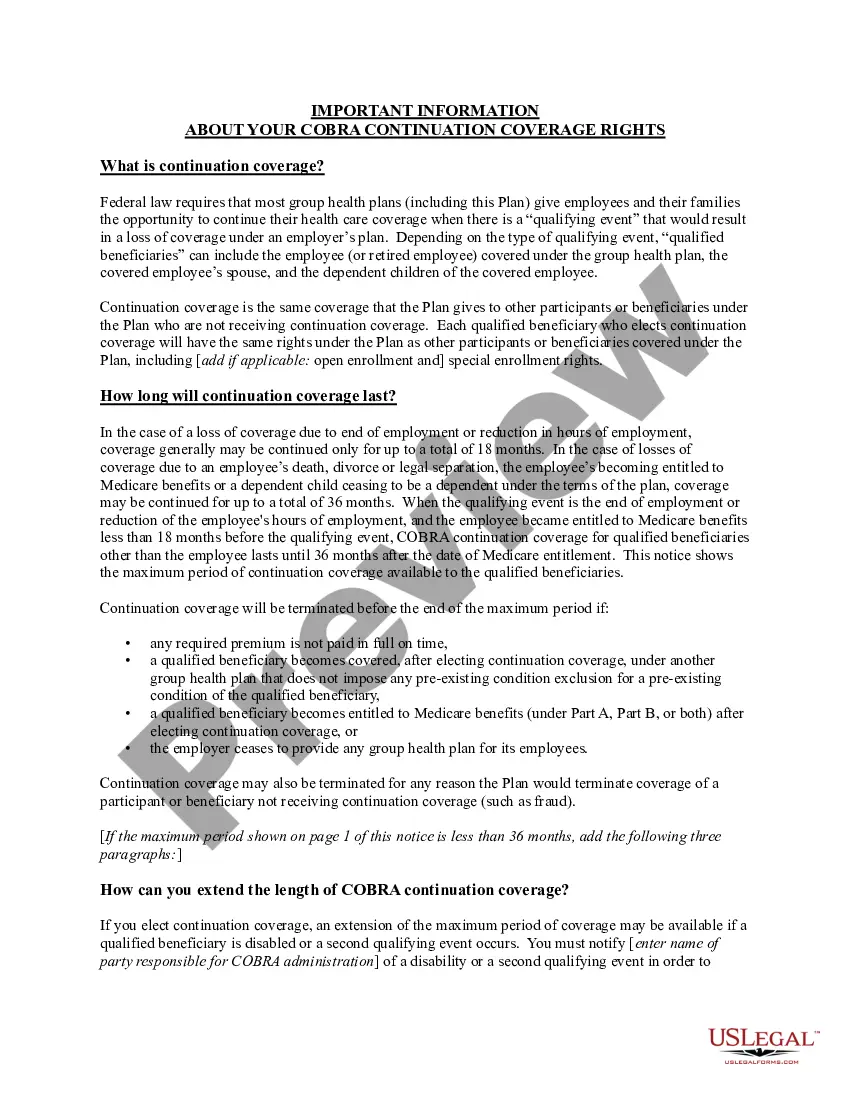
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
If you are entitled to elect COBRA coverage, you must be given an election period of at least 60 days (starting on the later of the date you are furnished the election notice or the date you would lose coverage) to choose whether or not to elect continuation coverage.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
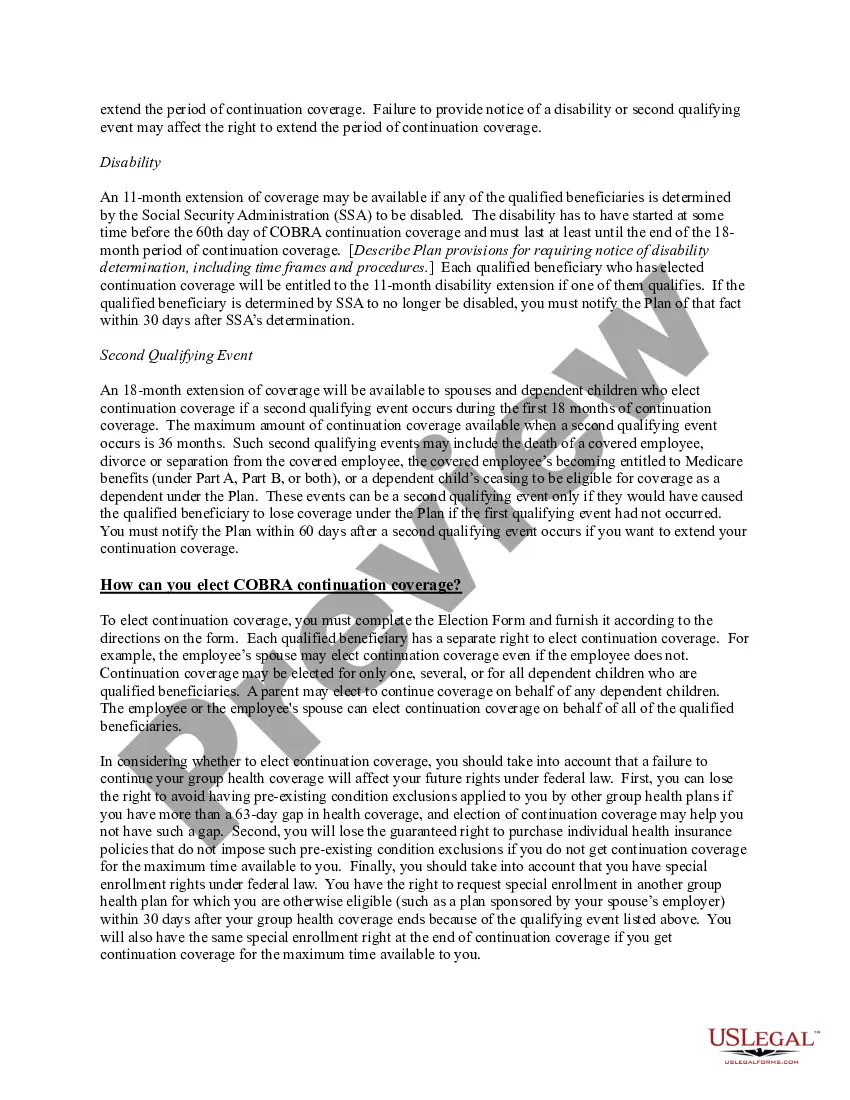
If a qualified beneficiary elected COBRA coverage outside of the normal 60-day COBRA election period (i.e., the qualified beneficiary took advantage of the tolling relief when electing COBRA coverage), the tolled period for making the initial premium payment begins on the date the COBRA notice was provided, and the
If you want to avoid paying the COBRA cost, go with a short-term plan if you're waiting for approval on another health plan. Choose a Marketplace or independent plan for broader coverage. Choose a high-deductible plan to keep your costs low.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Individual A receives the COBRA election notice on April 1, 2020 and elects COBRA continuation coverage on October 1, 2020, retroactive to April 1, 2020.