Montana Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
Are you situated in an environment where you consistently require documents for either organization or particular applications nearly every workday.
There are numerous legitimate document templates accessible online, but finding ones you can trust is not easy.
US Legal Forms provides thousands of form templates, such as the Montana Introductory COBRA Letter, designed to comply with federal and state requirements.
When you find the appropriate form, click Acquire now.
Choose the pricing plan you prefer, fill in the required details to create your account, and finalize your order using your PayPal or Visa or Mastercard.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Montana Introductory COBRA Letter template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Select the form you need and ensure it is for the appropriate region.
- Utilize the Preview button to review the form.
- Check the description to verify that you have chosen the correct form.
- If the form does not match what you are looking for, use the Search field to find a document that meets your requirements.
Form popularity
FAQ
Draft a letter stating facts why the COBRA benefits must be reinstated. The letter must provide your full legal name, address, Social Security number and COBRA policy number. The letter should be in proper business format and is best if free from all spelling and grammatical errors.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
If you feel the non-commencement or termination of your benefits under the Federal COBRA regulations was in error, you have the right to file an appeal by writing a letter which explains why you believe the coverage should be reinstated.
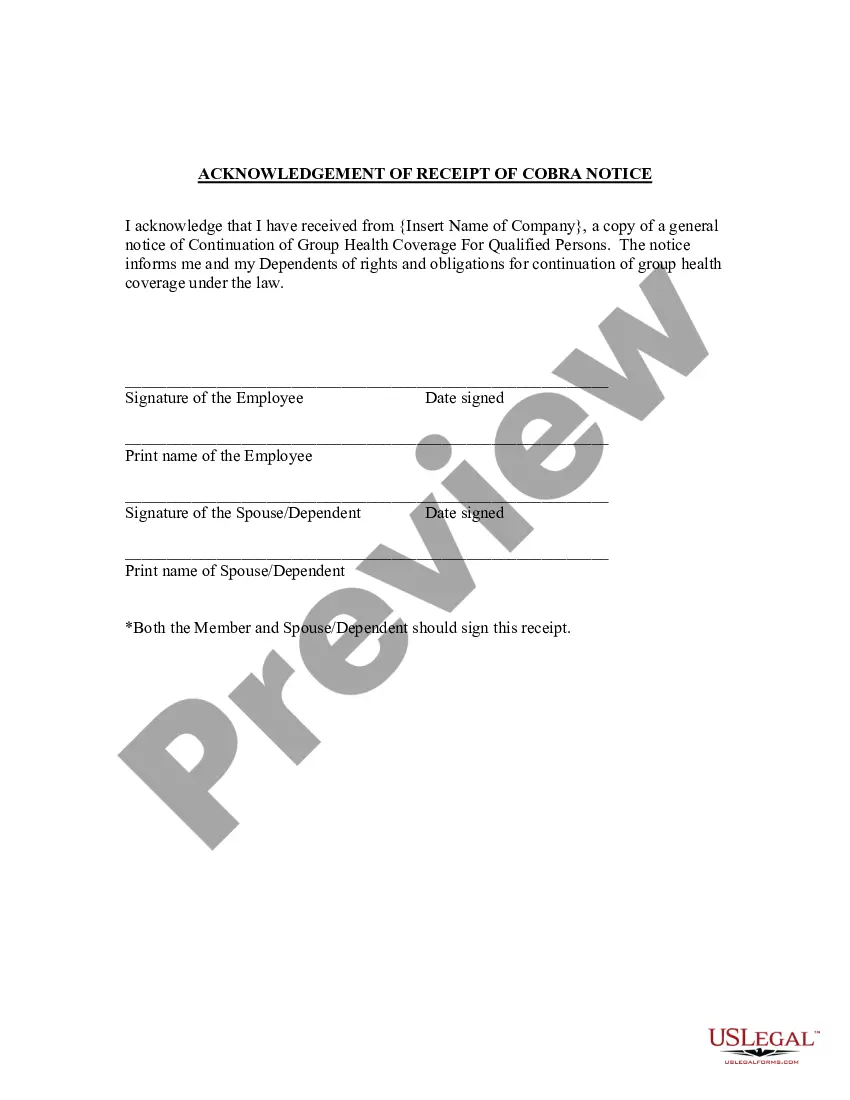
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
Once COBRA coverage is canceled, there is no option for reinstatement. Note that waiting until the end of the grace period to make payment may not allow enough time within the grace period to reconcile payment if your check is lost in the mail or is rejected by your bank.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
A COBRA letter is drafted by the plan administrator with a copy mailed to each qualified beneficiary before the coverage is terminated. The COBRA termination letter format must include the reason why the coverageis being terminated, the rights of the beneficiaries, and the specific date the coverage will end.