Minnesota Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
Selecting the correct legal document template can be a challenge.
There are numerous templates available online, but how can you find the legal form you need.
Utilize the US Legal Forms website. This service offers thousands of templates, including the Minnesota Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, suitable for business and personal needs. All forms are vetted by professionals and meet both state and federal requirements.
Once you are convinced that the form is appropriate, click the Buy now button to acquire the form. Choose your preferred pricing plan and fill in the necessary information. Create your account and complete the order using your PayPal account or credit card. Select the file format and download the legal document template to your device. Complete, modify, print, and sign the received Minnesota Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. US Legal Forms is the largest repository of legal templates where you can access a variety of document formats. Utilize the service to obtain professionally crafted documents that meet state requirements.
- If you are already a member, Log In to your account and select the Download button to retrieve the Minnesota Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
- Use your account to search through the legal forms you have previously purchased.
- Visit the My documents section of your account to download another copy of the document you need.
- If you are a new user of US Legal Forms, here are some simple steps to follow.
- First, confirm you have selected the correct form for your area. You can browse the template using the Preview feature and review the form details to ensure it is suitable for you.
- If the form does not meet your requirements, use the Search box to find the appropriate form.
Form popularity
FAQ
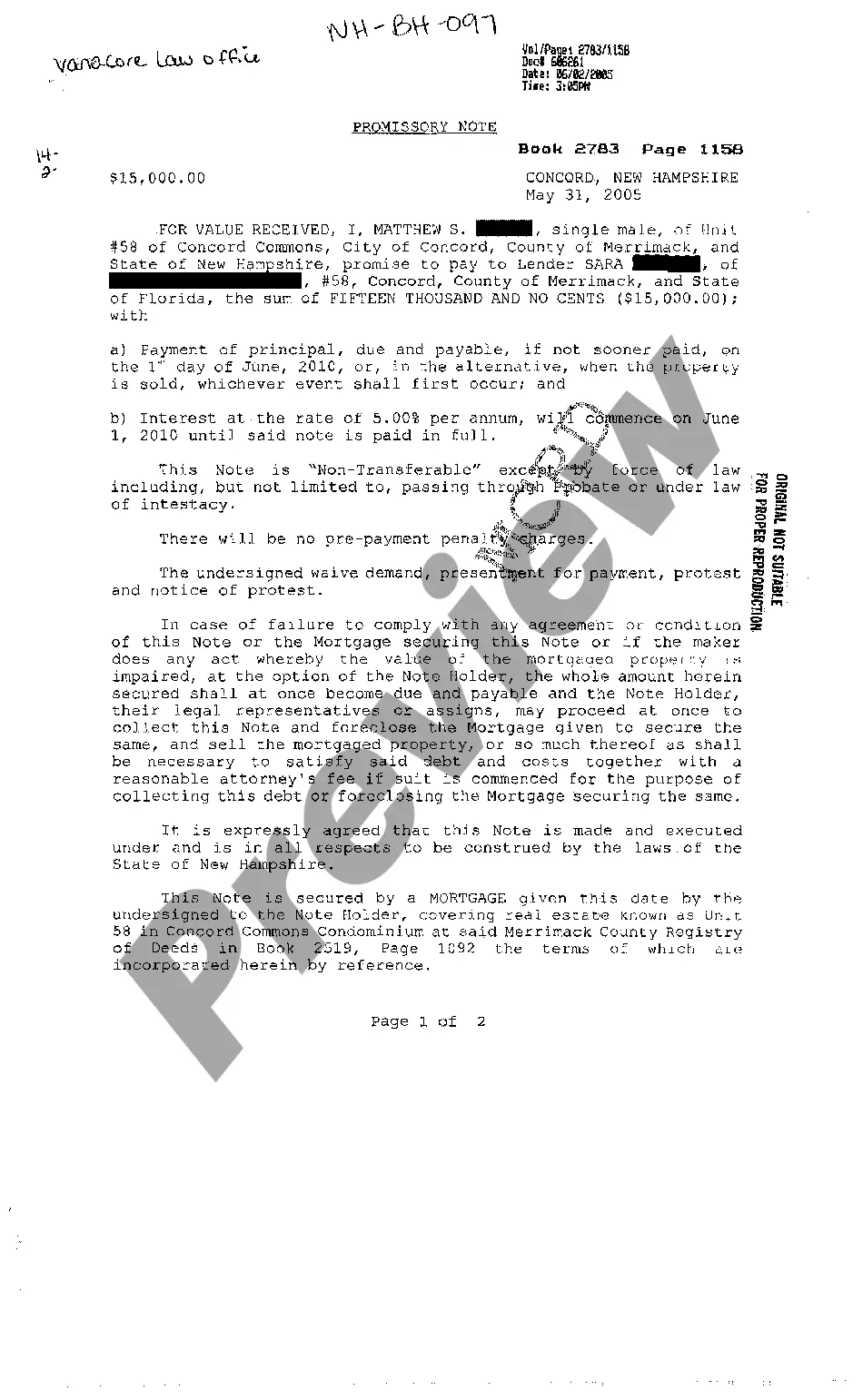
The statute 62A.17 in Minnesota provides guidelines regarding the notification process that employers must follow when terminating continuation coverage. Specifically, it requires employers to send a Minnesota Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. This notice informs employees about the cessation of their health coverage options and the reasons behind it. Understanding this statute can empower you as an employee or employer to ensure compliance and protect your rights.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
A terminated employee's paycheck must be paid within 24 hours of the employee's demand for wages (see Minnesota Statutes 181.13). If an employee quits, wages are due on the next pay period that is more than five days after quitting.
When we quit or are terminated, we are generally not entitled to PTO as a payout when we leave the company. In other words, there is no Minnesota law requiring an employer to pay out PTO time when we leave employment.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.
The length of continuation depends on the qualifying event. Legal separation or divorce - dependent children can continue up to 36 months under federal law. Under Minnesota law, they can continue until they become covered under another group plan, or until they no longer qualify as dependents under state law.
If you are enrolled on your parent's coverage and turn 26, you are eligible to continue Medical and Dental benefits on COBRA for 36 months. Your first day of COBRA coverage will be the first of the month following the date you turn 26.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.