Minnesota Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
Finding the suitable official document template can be a challenge.
Naturally, there are numerous templates available online, but how do you locate the official form you need.
Leverage the US Legal Forms website. The service offers thousands of templates, including the Minnesota Notice of Qualifying Event from Employer to Plan Administrator, suitable for business and personal needs.
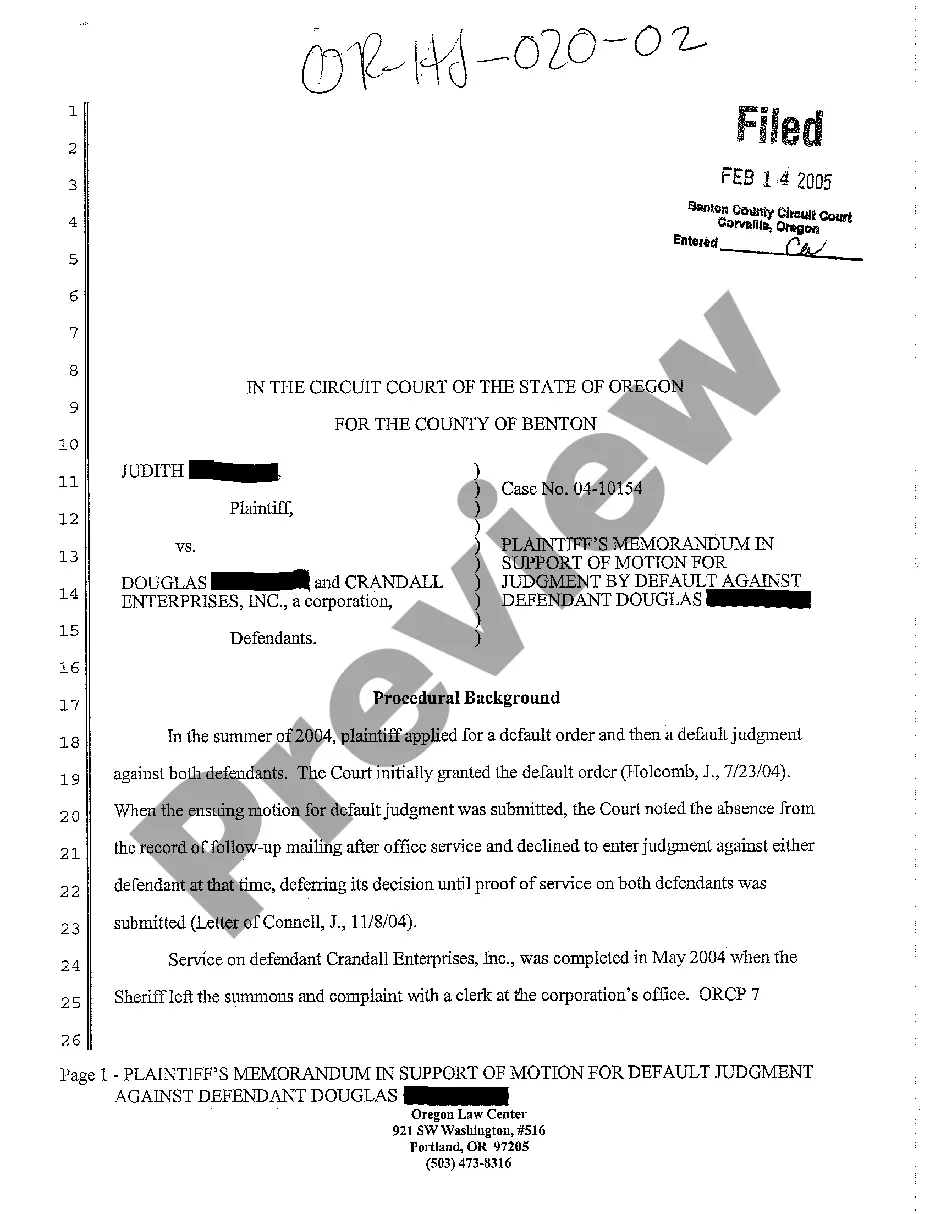
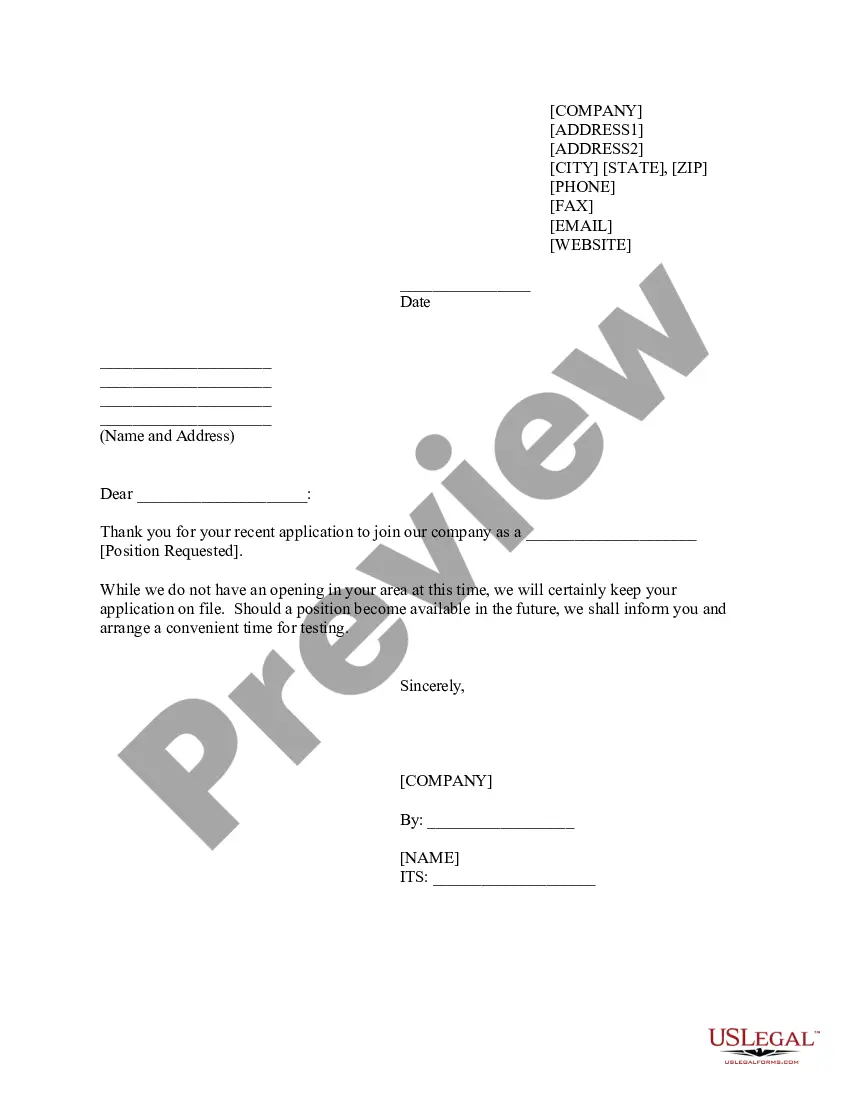
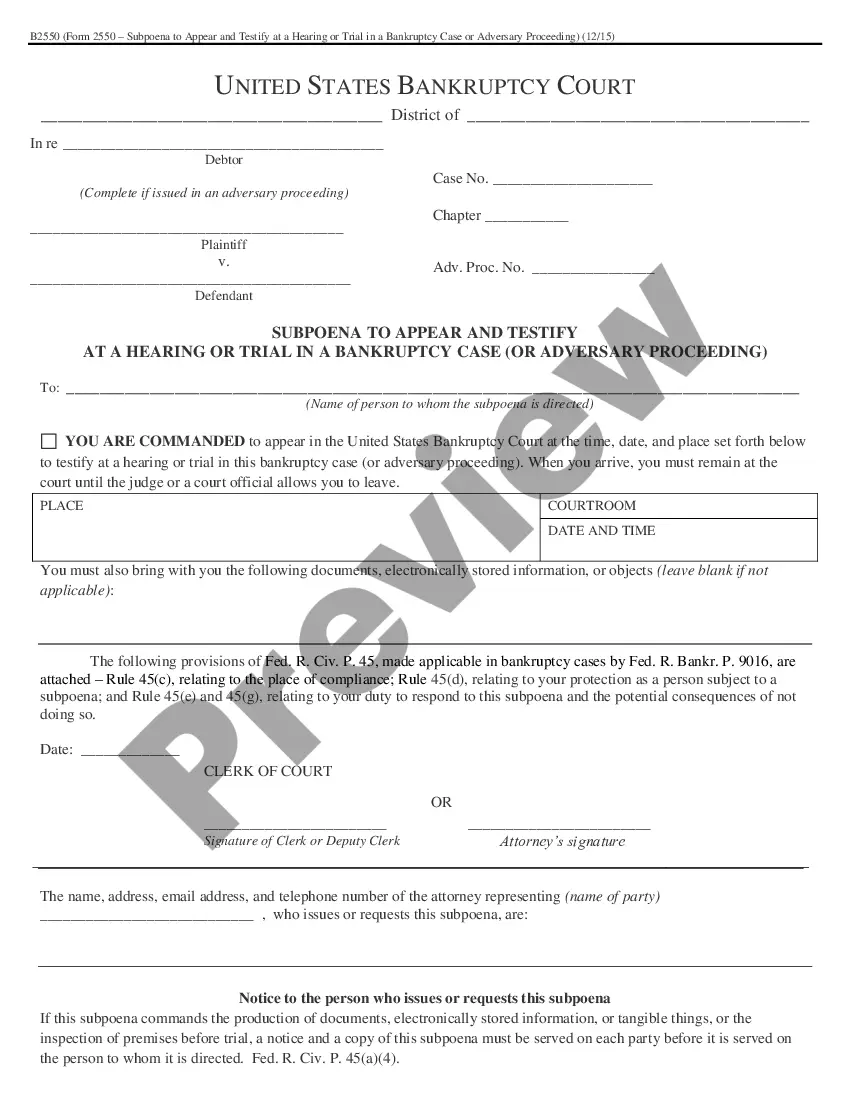
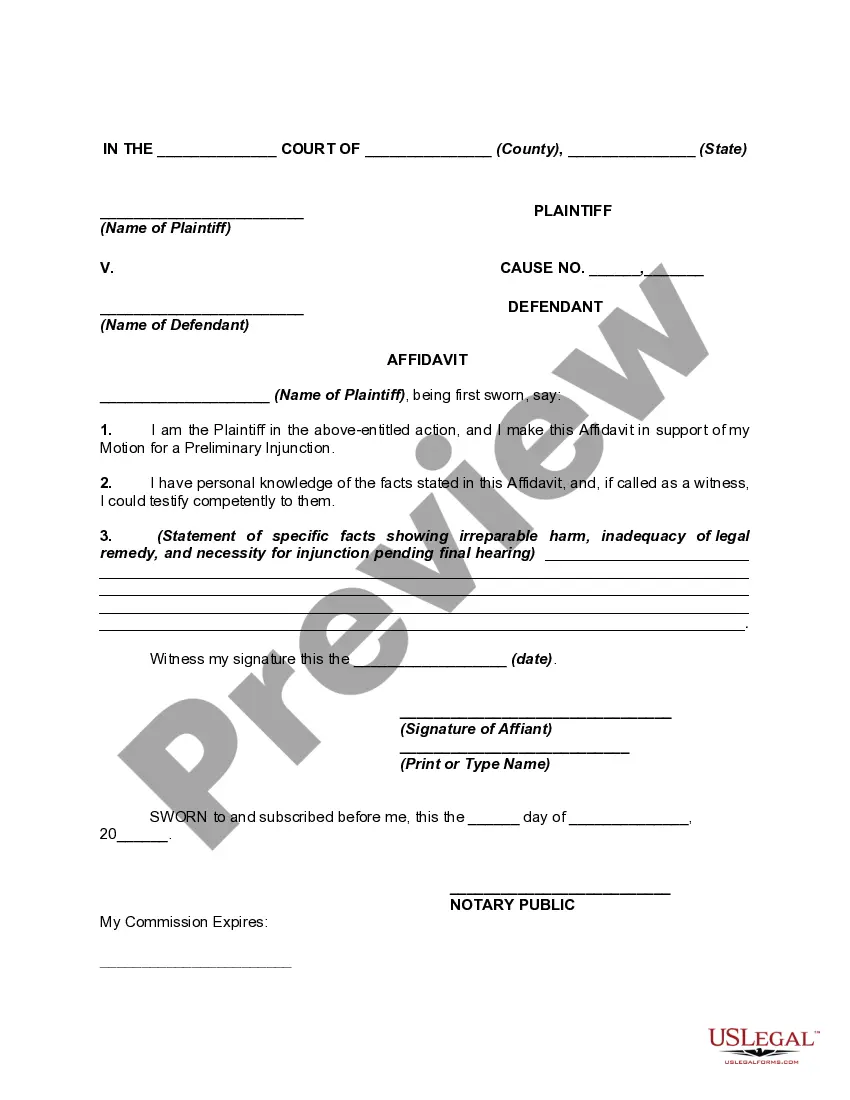
You can view the form using the Review button and read the form description to confirm its suitability for your needs.
- All the forms are reviewed by professionals and comply with state and federal regulations.
- If you are already registered, Log In to your account and click on the Download button to obtain the Minnesota Notice of Qualifying Event from Employer to Plan Administrator.
- Use your account to search for the legal documents you have previously purchased.
- Visit the My documents section of your account and download another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple instructions you can follow.
- First, ensure you have chosen the correct form for your locality.
Form popularity
FAQ
When an agent discusses long-term care insurance in Minnesota, they are required to provide prospective clients with an outline of coverage. This document details the benefits and terms of the policy, helping consumers make informed decisions. Knowing how this works is essential so that you can respond to any Minnesota Notice of Qualifying Event from Employer to Plan Administrator effectively.
Consumers may also extend COBRA coverage longer than the initial 18-month period with a second qualifying event (e.g., divorce or death), up to an additional 18 months, for a total of 36 months.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
If you are enrolled on your parent's coverage and turn 26, you are eligible to continue Medical and Dental benefits on COBRA for 36 months. Your first day of COBRA coverage will be the first of the month following the date you turn 26.
If you are enrolled on your parent's coverage and turn 26, you are eligible to continue Medical and Dental benefits on COBRA for 36 months. Your first day of COBRA coverage will be the first of the month following the date you turn 26.
How Long Does COBRA Last After You Quit? You may remain on your former employer's COBRA insurance plan for up to 18 months. Depending on your circumstances you or your qualified dependents may be eligible for up to 36 months of continuing coverage.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too.