Maine COBRA Continuation Coverage Election Form
Description
How to fill out COBRA Continuation Coverage Election Form?
Selecting the most suitable authorized document template can be a challenge.
Of course, there are numerous templates available online, but how can you find the legal form you require.
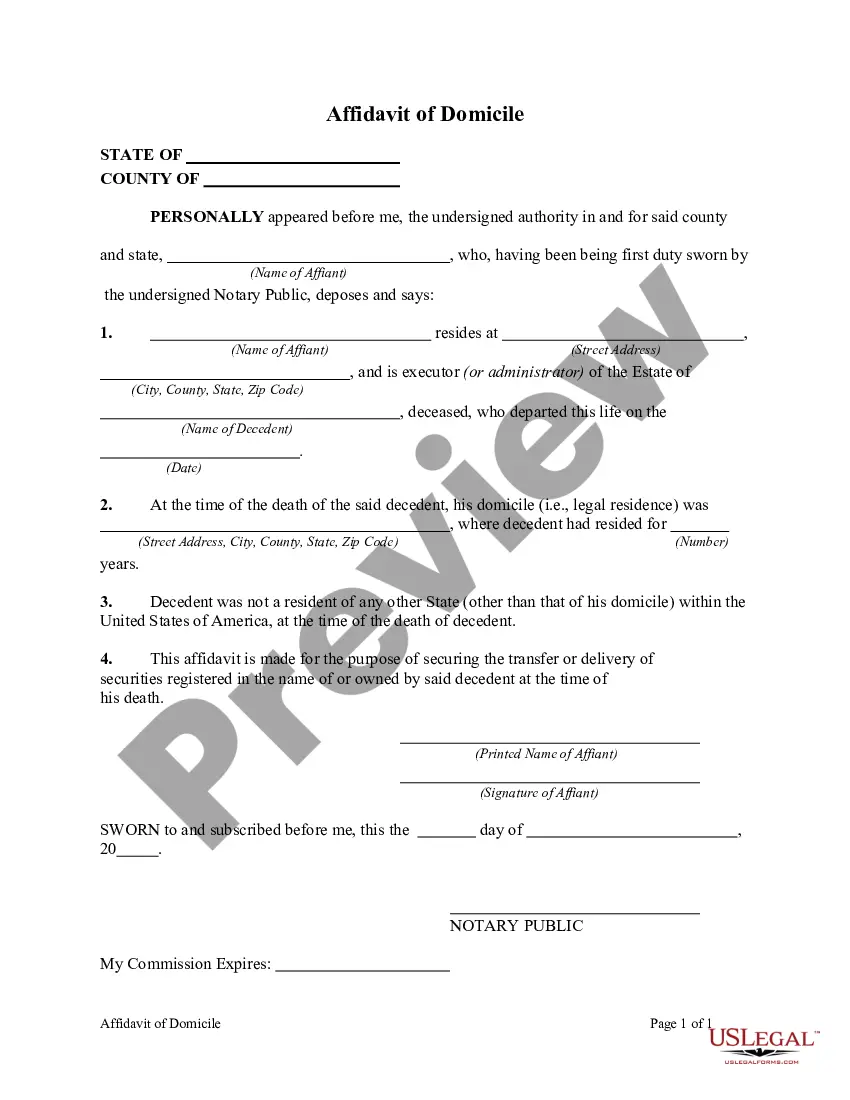
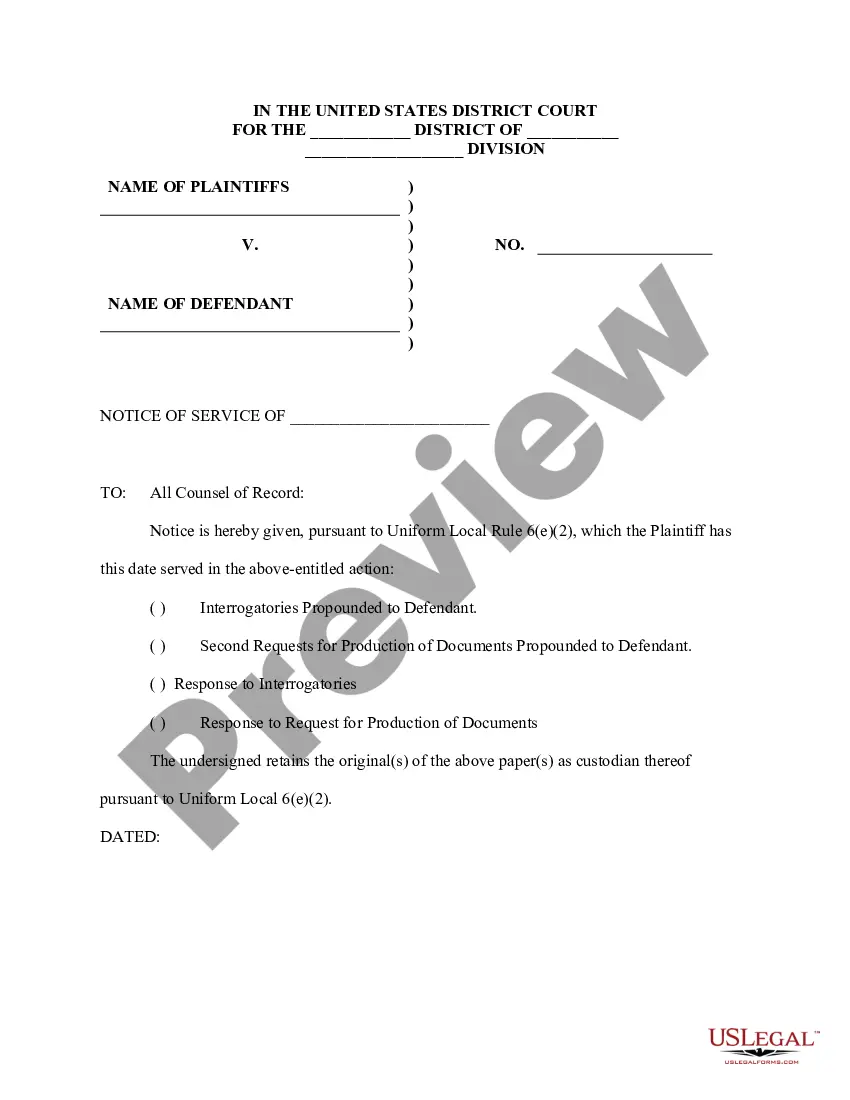
Make use of the US Legal Forms website. The platform offers a vast array of templates, including the Maine COBRA Continuation Coverage Election Form, which can be utilized for both business and personal needs.
You can browse the form using the Review button and read the form description to ensure it meets your requirements.
- All of the forms are reviewed by experts and meet state and federal standards.
- If you are already a registered user, Log In to your account and click the Download button to obtain the Maine COBRA Continuation Coverage Election Form.
- Leverage your account to search for the legal forms you have previously acquired.
- Visit the My documents section of your account to retrieve another copy of the document you need.
- For those new to US Legal Forms, here are some simple steps to follow.
- First, make sure you have selected the correct form for your city/state.
Form popularity
FAQ
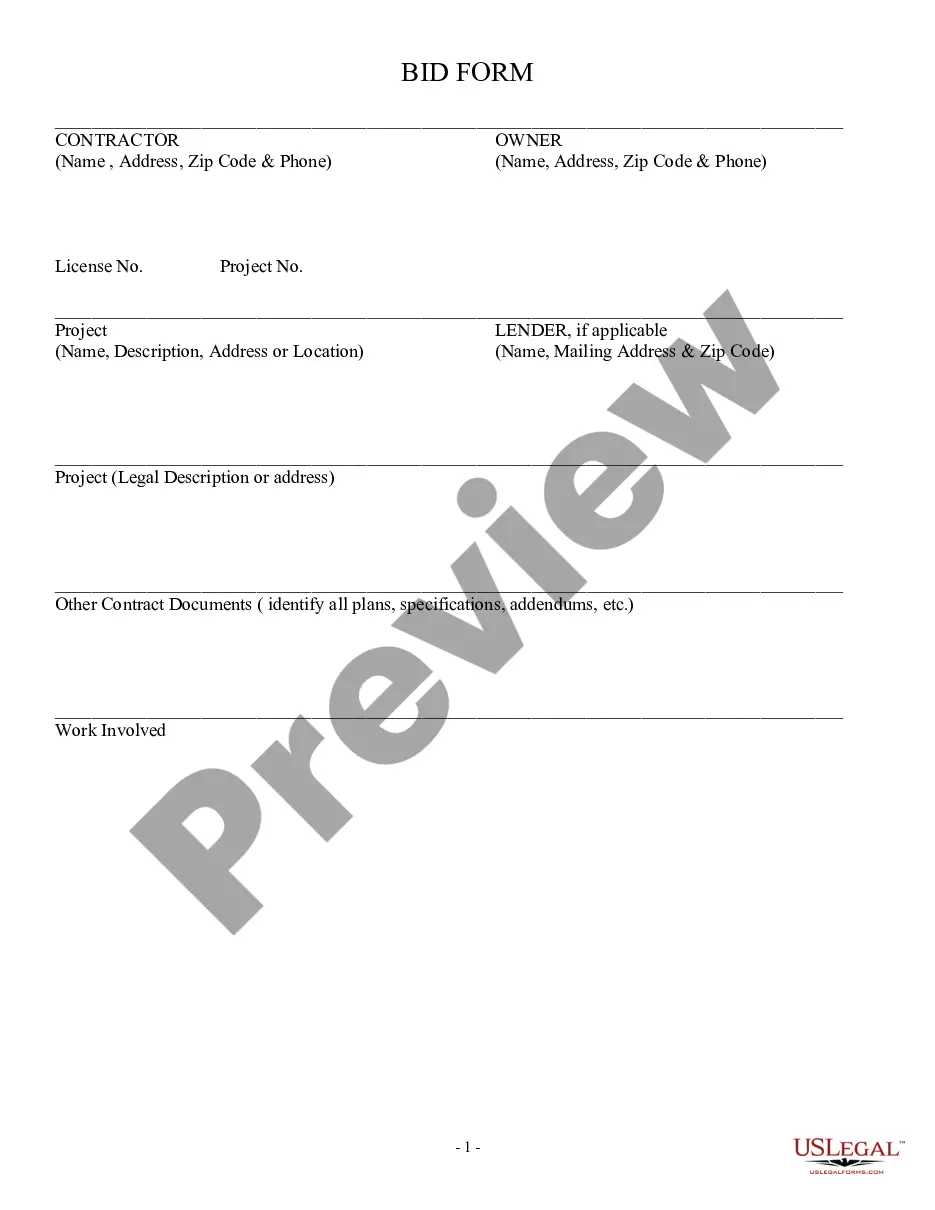
Under the Consolidated Omnibus Budget Reconciliation Act (COBRA), many employees and their families who would lose group health coverage because of serious life events are able to continue their coverage under the employer's group health plan, usually at their own expense, at least for limited periods of time.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
If you are entitled to an 18 month maximum period of continuation coverage, you may become eligible for an extension of the maximum time period in two circumstances. The first is when a qualified beneficiary is disabled; the second is when a second qualifying event occurs.
COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
State continuation coverage refers to state laws that allow people to extend their employer-sponsored health insurance even if they're not eligible for extension via COBRA. As a federal law, COBRA applies nationwide, but only to employers with 20 or more employees.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.