Maryland Sample Letter regarding Bill
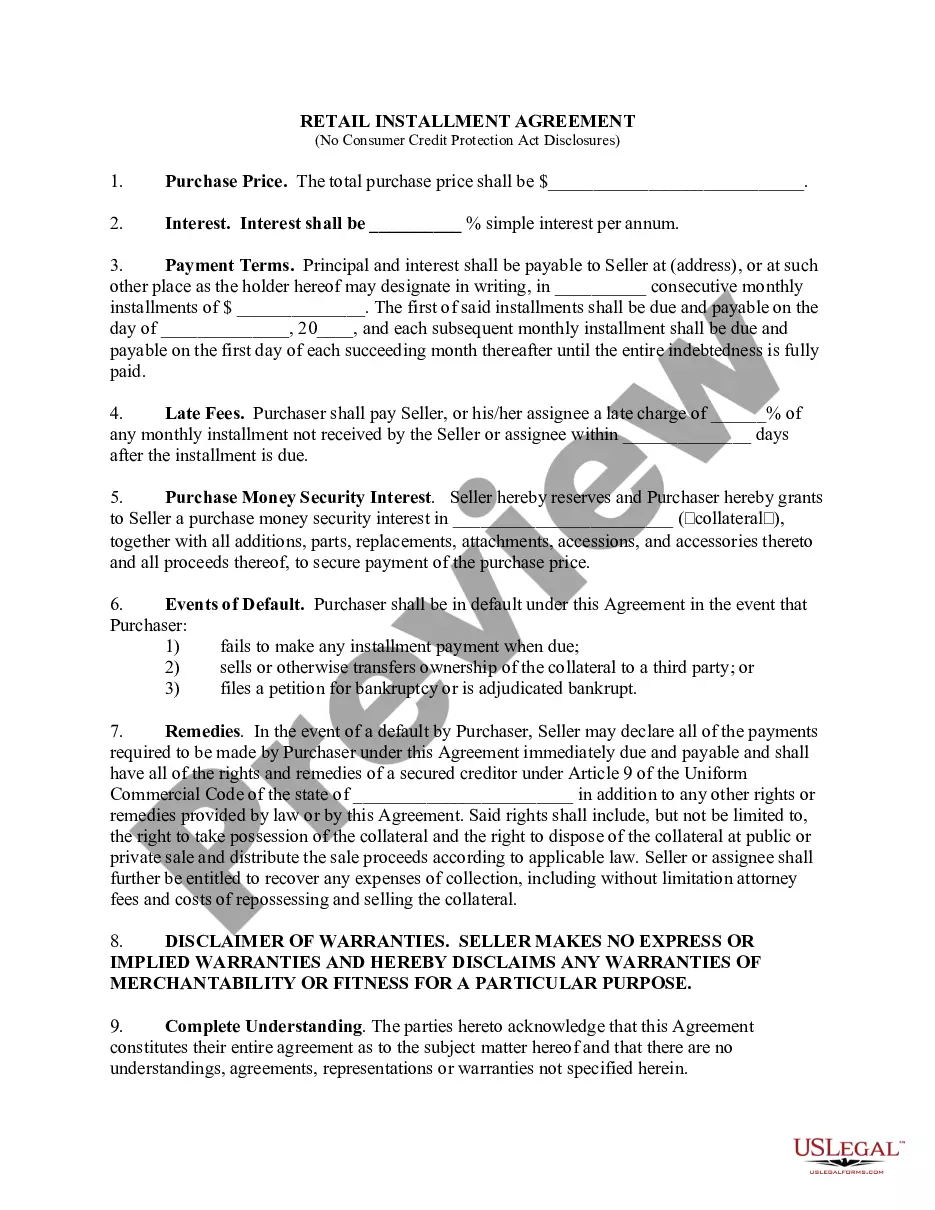
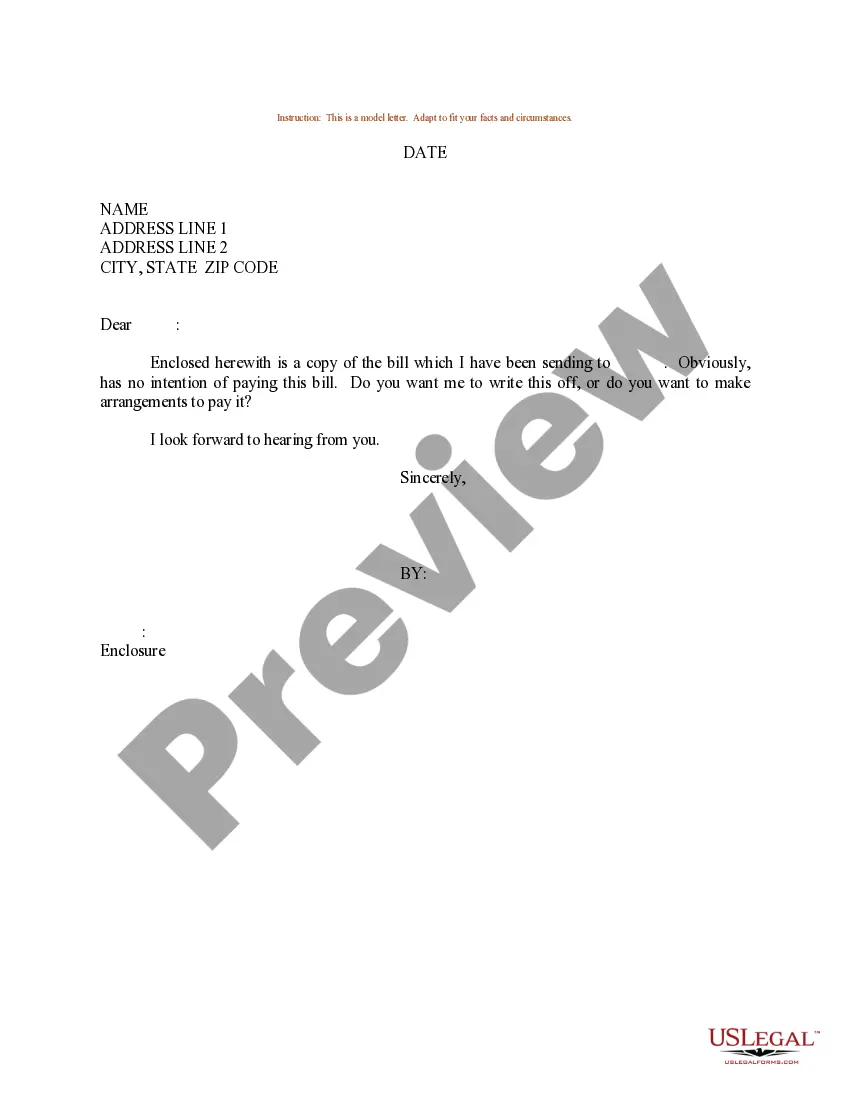
Description
How to fill out Sample Letter Regarding Bill?
Are you in a situation where you will require documentation for potentially commercial or personal purposes almost every day.
There is an assortment of legal document templates accessible online, but finding ones you can rely on is not easy.
US Legal Forms provides thousands of form templates, such as the Maryland Sample Letter regarding Bill, which are crafted to comply with federal and state requirements.
Utilize US Legal Forms, one of the largest selections of legal forms, to save time and avoid errors.
The service provides professionally created legal document templates that you can use for various purposes. Create an account on US Legal Forms and start making your life a bit simpler.
- If you are already familiar with the US Legal Forms website and possess an account, just Log In.
- Then, you can download the Maryland Sample Letter regarding Bill template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the document you need and ensure it corresponds to the correct city/region.
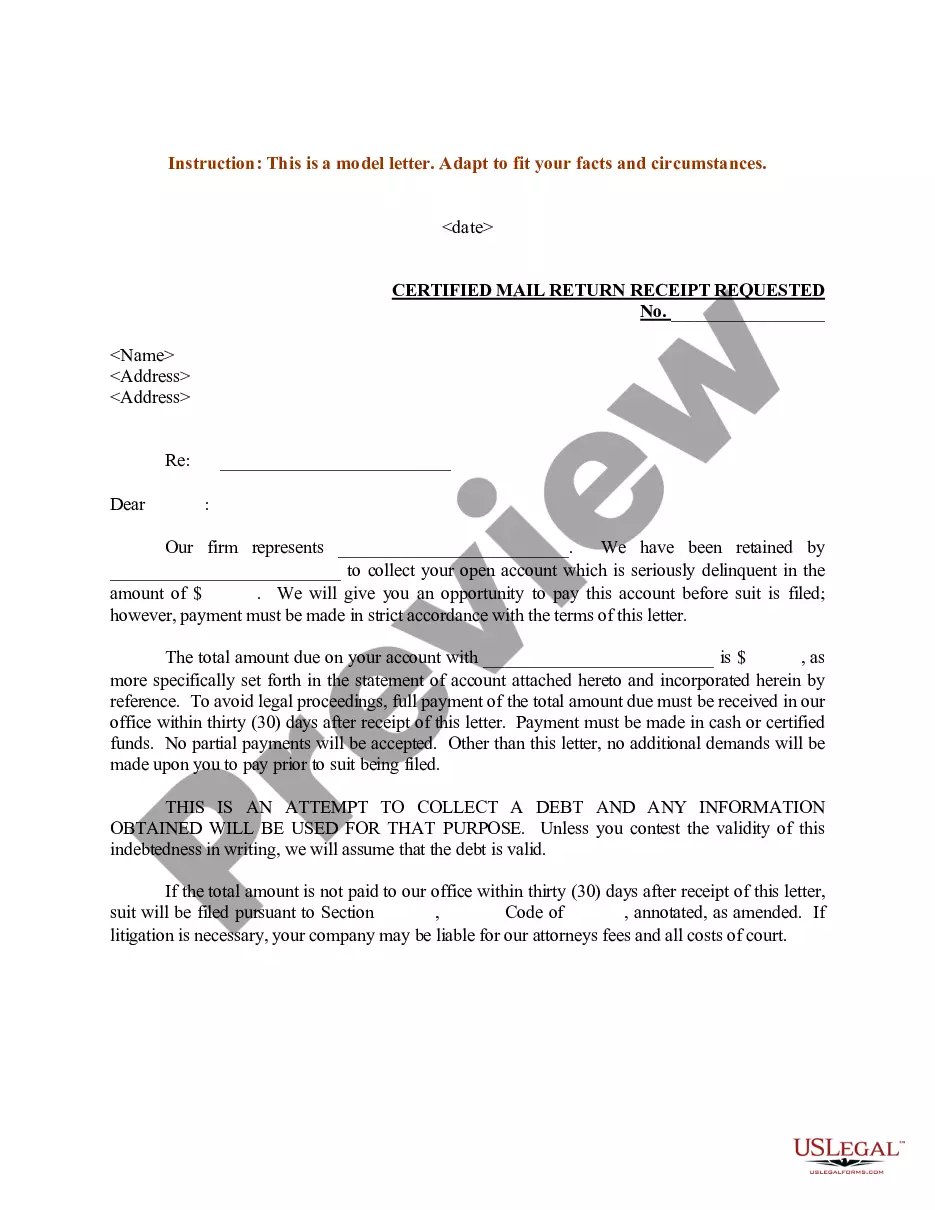
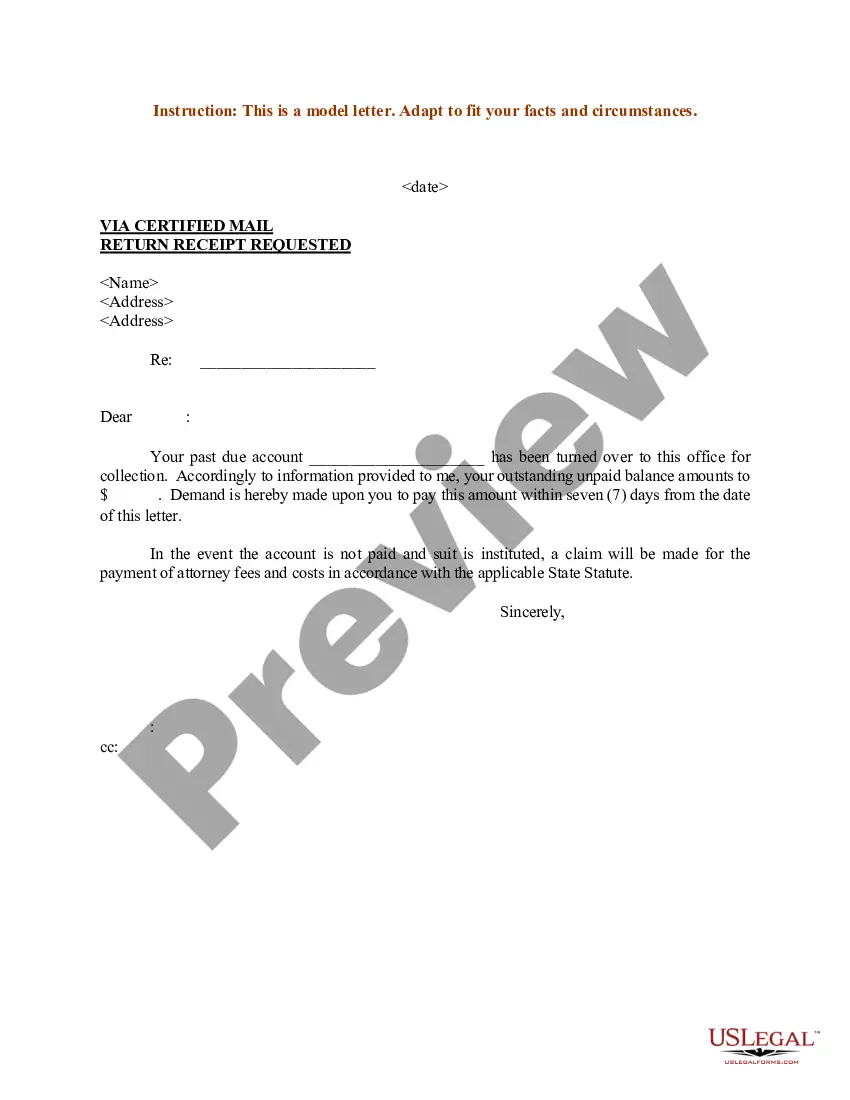
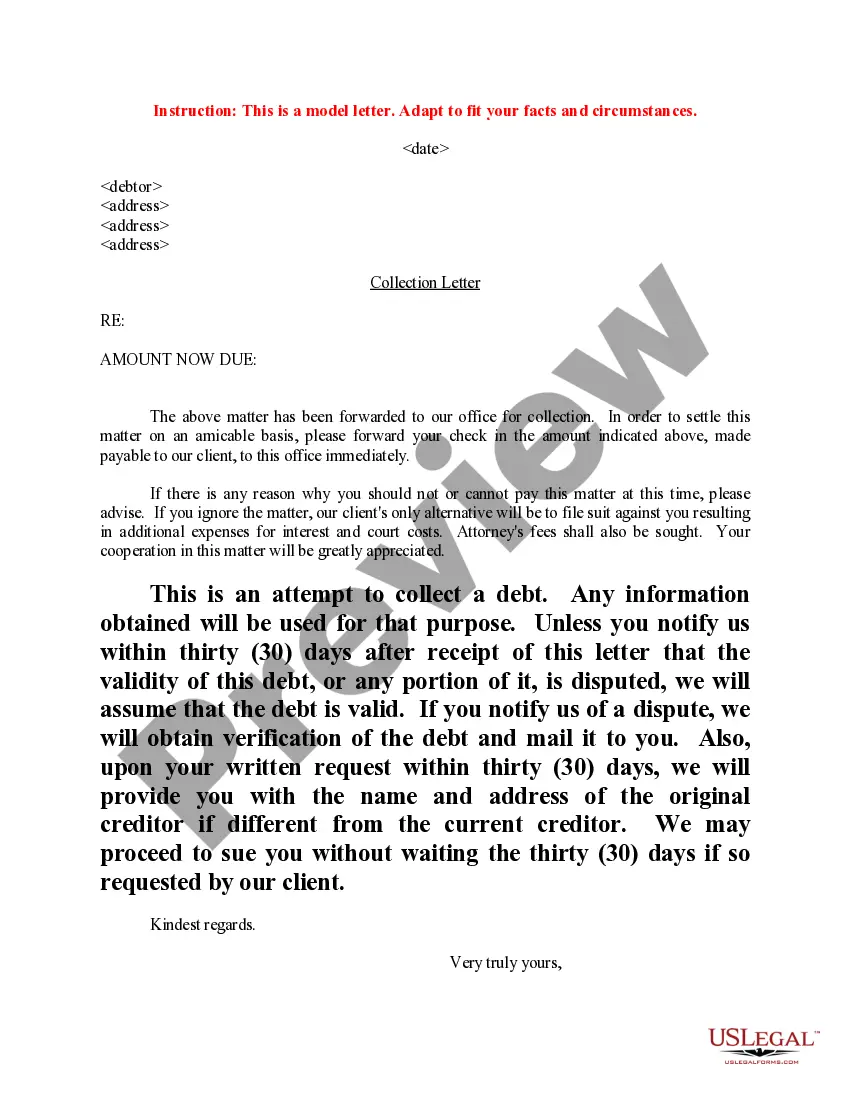
- Utilize the Review button to verify the document.
- Examine the details to make sure you have selected the right document.
- If the document is not what you are looking for, use the Search field to locate the document that fits your needs and requirements.
- Once you have the correct document, click Acquire now.
- Select the payment option you prefer, fill in the necessary details to create your account, and purchase the order using your PayPal or credit card.
- Choose a convenient file format and download your copy.
- Access all the document templates you have purchased in the My documents section.
- You can download another copy of the Maryland Sample Letter regarding Bill at any time if needed.
- Click on the desired document to download or print the template.
Form popularity
FAQ
Billing Time Statute You must submit a clean claim to the Maryland Medical Assistance Program within 12 months of the date of service (for acute hospitals?date of discharge). A clean claim is an original, correctly completed claim that is ready to process. Submit claims immediately after providing services.
State and federal law protects you from surprise or balance billing if you receive emergency care, including emergency behavioral health services at a medical facility or when you're treated at an in-network hospital or outpatient surgical facility by an out-of-network provider.
A hospital facility may not "balance bill" a Medicaid recipient for services for which the recipient did not knowingly agree to be responsible. Please refer any questions regarding this transmittal to the staff specialist for hospital services at (410) 767-1478.
Balance billing can happen when a patient receives covered health care services from an out-of- network provider or an out-of-network facility (a hospital, for example). In-network providers agree with an insurance company to accept the insurance payment in full, and don't balance bill.
Maryland-specific balance billing protections If you are in a PPO or EPO governed by Maryland law, hospital-based or on-call physicians paid directly by your PPO or EPO (assignment of benefits) may not balance bill you for services covered under your plan and can't ask you to waive your balance billing protections.
A balance bill is issued when a provider charges a patient with the amount the insurance company doesn't pay. For example, the dermatologist charges the insurance company $300. The insurance company agreed to pay $150. If the doctor then charges the patient the remaining $150, the patient will receive a balance bill.