Massachusetts Authorization to Use or Disclose Protected Health Information
Description
How to fill out Authorization To Use Or Disclose Protected Health Information?
Are you in a circumstance where you require paperwork for both corporate or particular aims nearly every day.
There are numerous sanctioned document templates available online, yet finding reliable versions isn't simple.
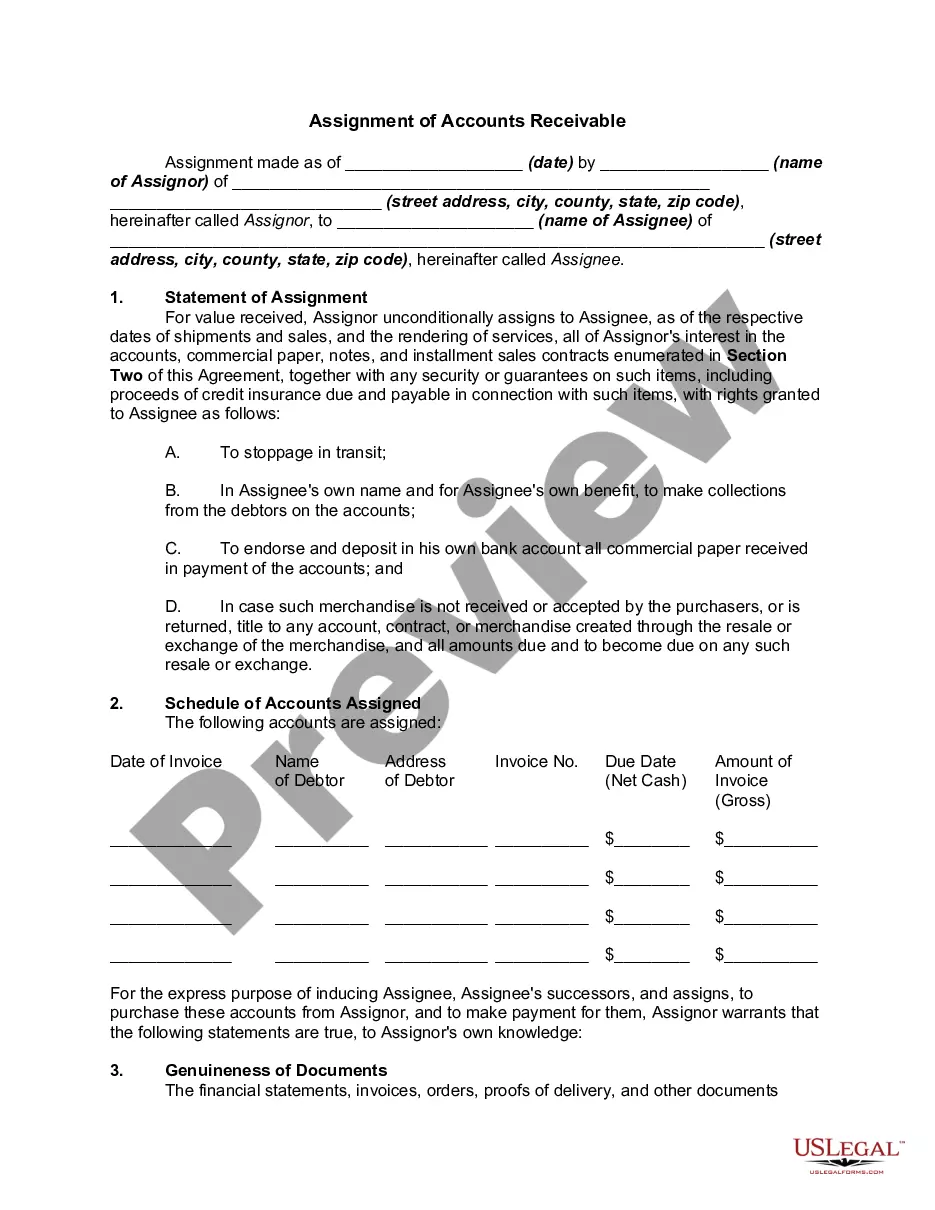
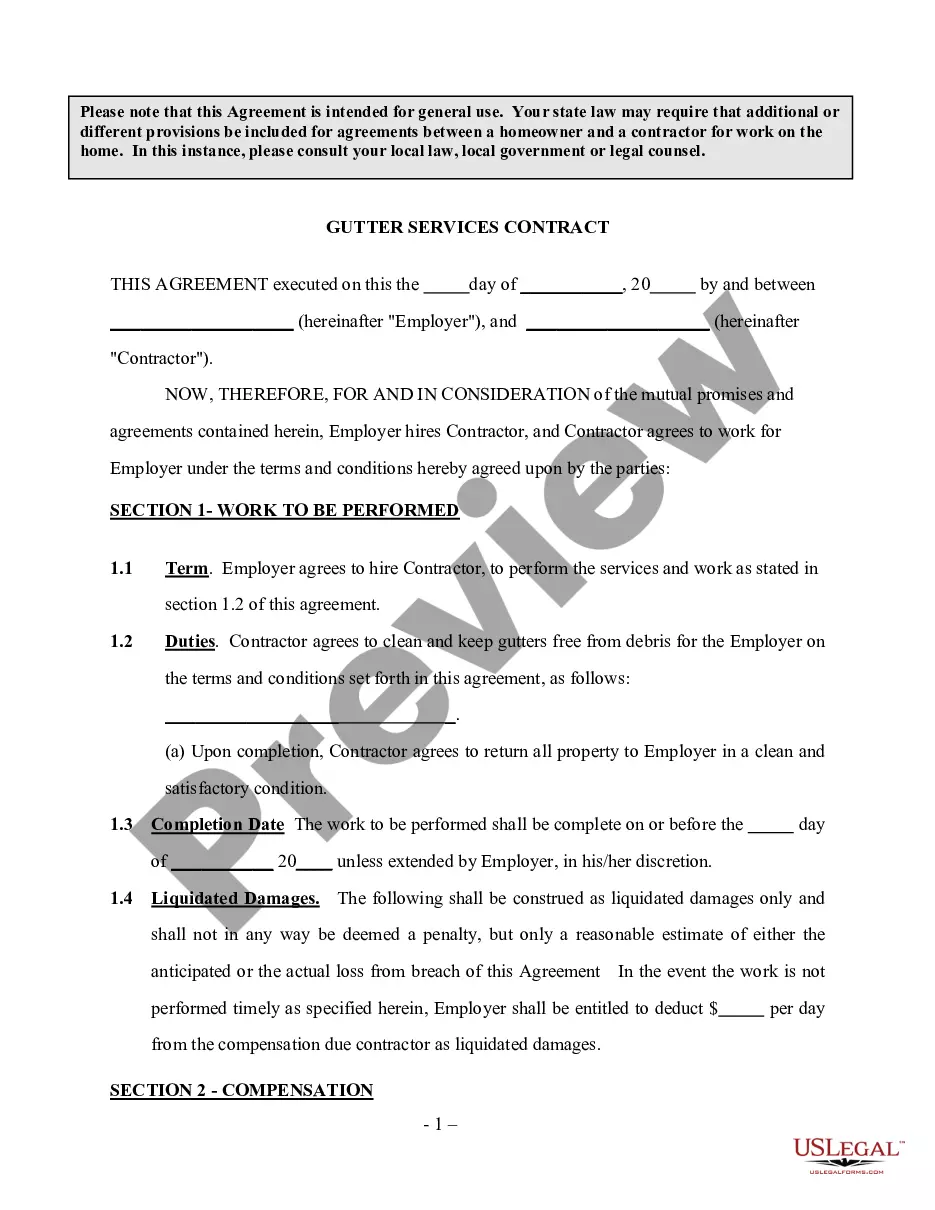
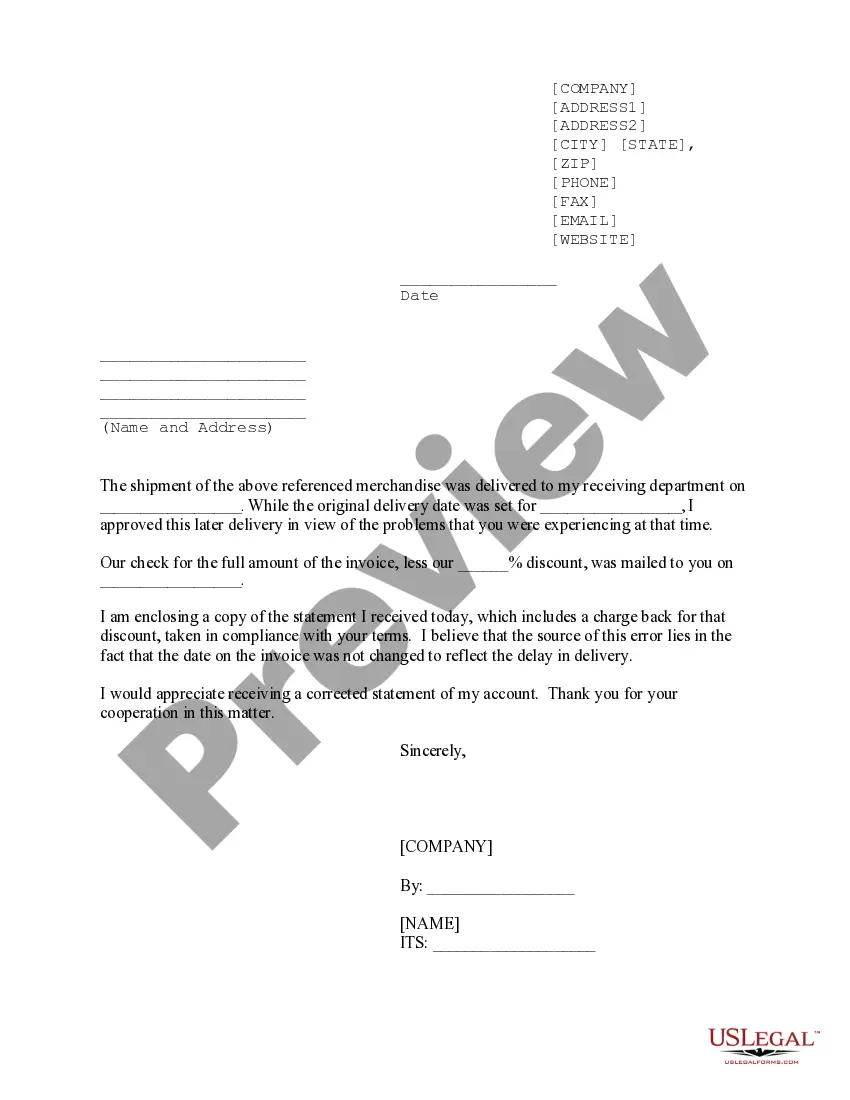
US Legal Forms offers thousands of form templates, such as the Massachusetts Authorization to Use or Disclose Protected Health Information, that are designed to comply with state and federal regulations.
Once you find the right form, click Purchase now.
Choose the pricing plan you prefer, fill in the necessary information to create your account, and complete your purchase using PayPal or credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply sign in.
- Then, you can download the Massachusetts Authorization to Use or Disclose Protected Health Information template.
- If you do not have an account and wish to start using US Legal Forms, follow these instructions.
- Find the form you require and ensure it is for the correct area/region.
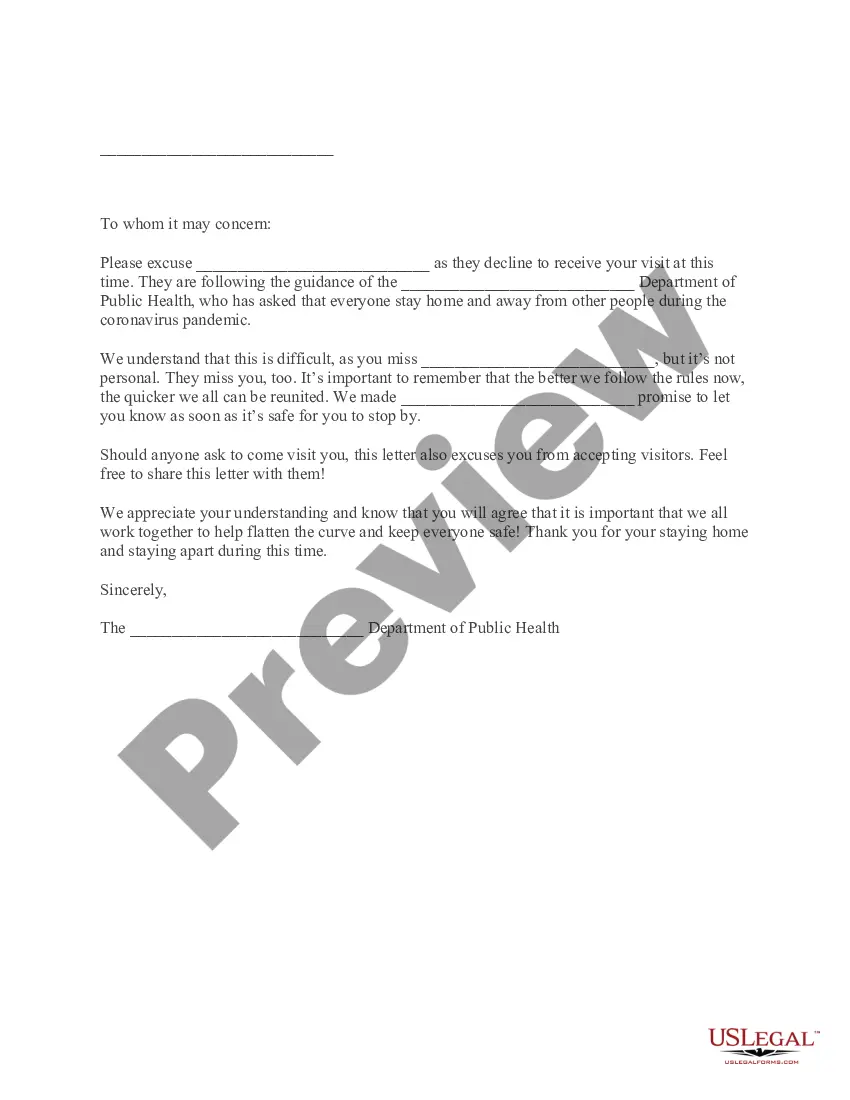
- Utilize the Preview button to review the form.
- Examine the details to confirm that you have selected the correct form.
- If the form isn't what you need, use the Search field to locate the form that fulfills your needs and requirements.
Form popularity
FAQ
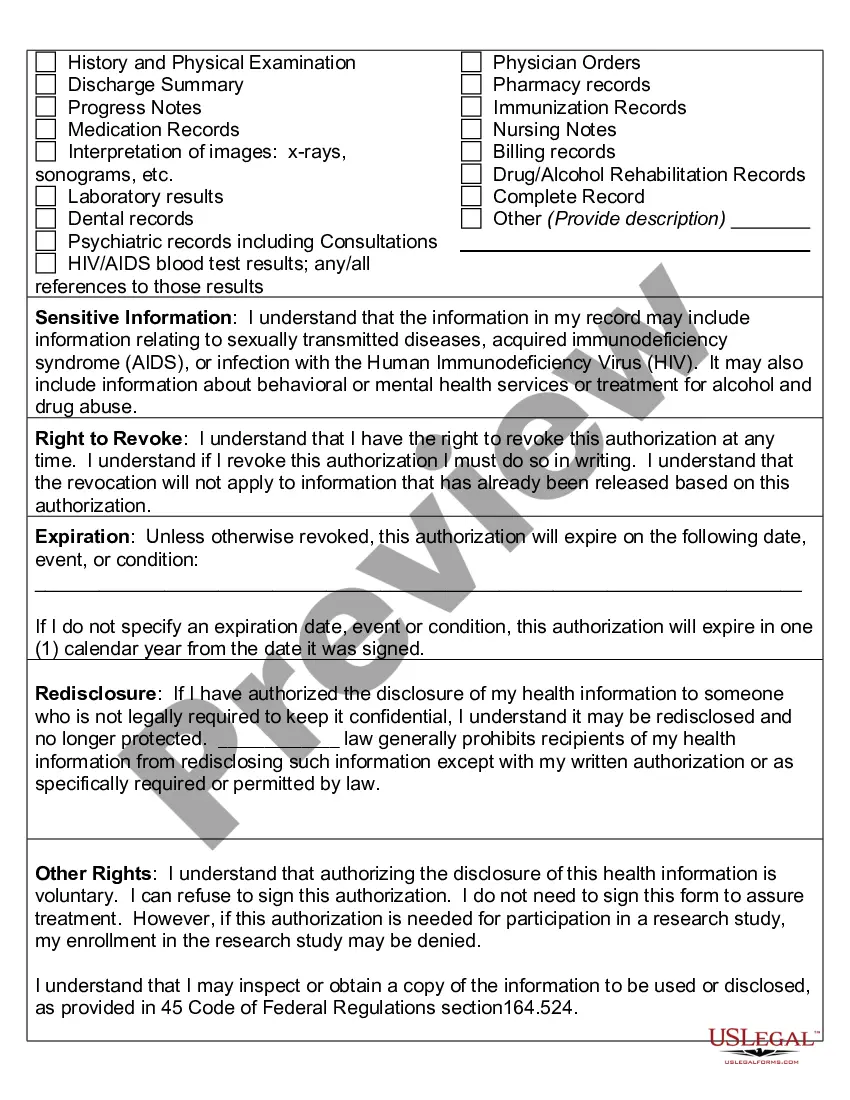
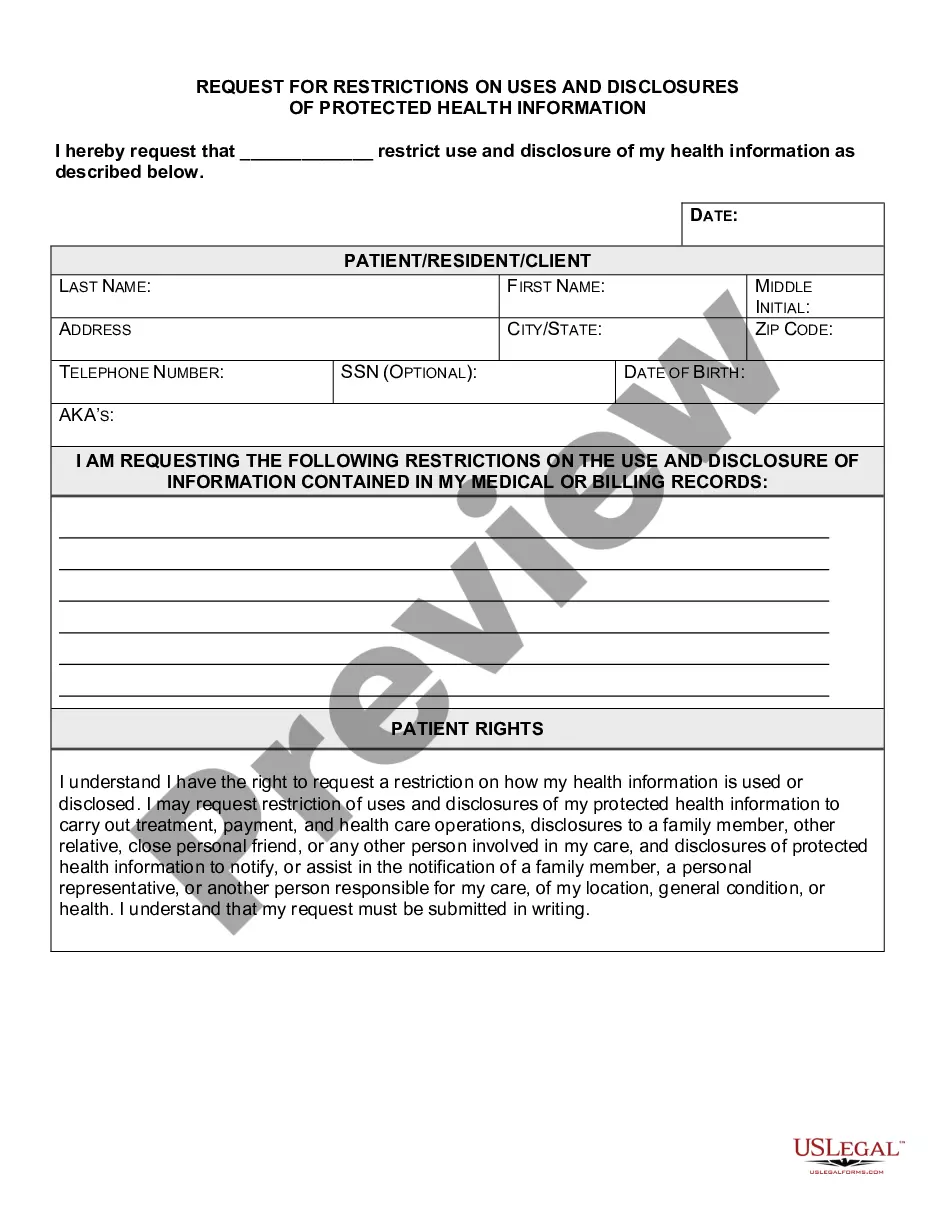
Unauthorized access, use, and disclosure of protected health information occur when personal medical data is shared or used without proper consent or outside the legal framework. This can lead to serious privacy breaches and legal consequences. By using the Massachusetts Authorization to Use or Disclose Protected Health Information, you can prevent unauthorized activities and protect both the patient's rights and your organization from potential liabilities.
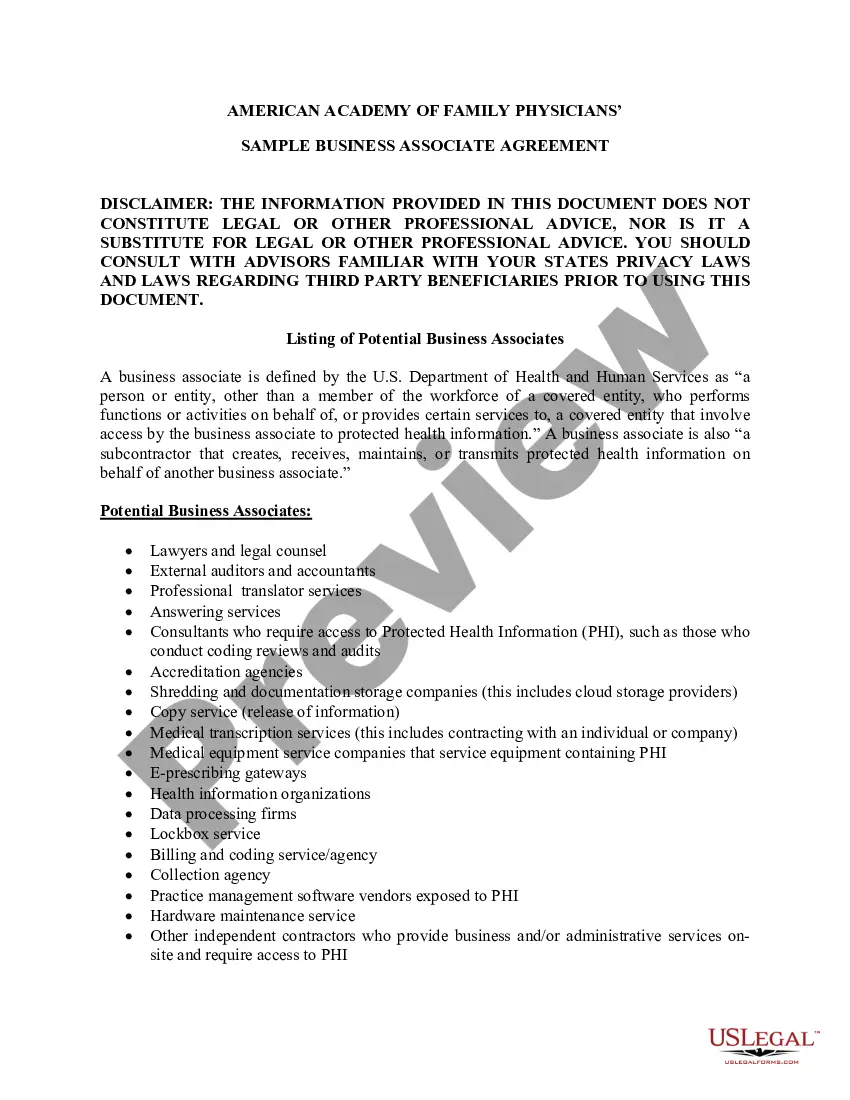
In limited circumstances, the HIPAA Privacy Rule permits covered entities to use and disclose health information without individual authorization. Covered entities may use and disclose protected health information without authorization for their own treatment, payment, and healthcare operations.
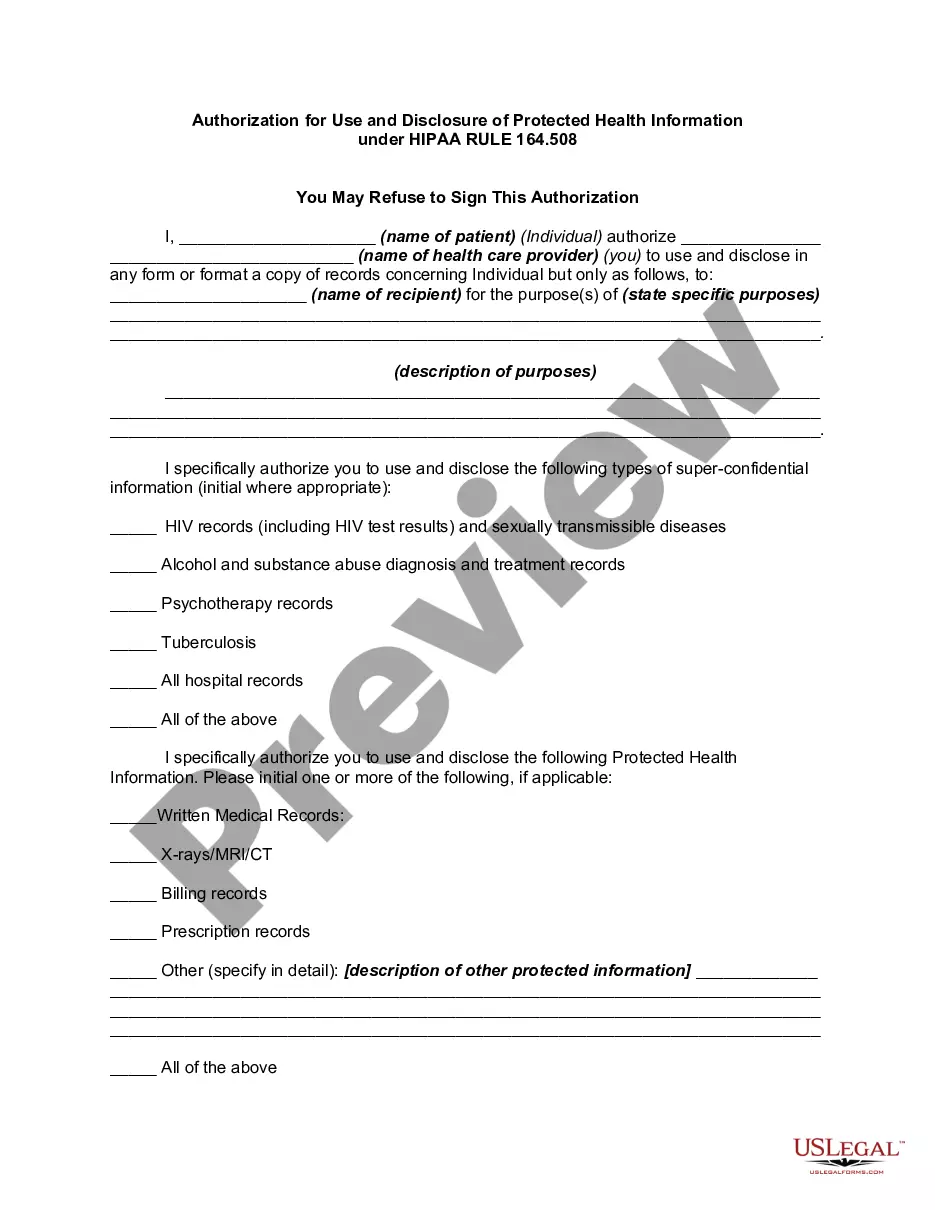
In general, a covered entity may only use or disclose PHI if either: (1) the HIPAA Privacy Rule specifically permits or requires it; or (2) the individual who is the subject of the information gives authorization in writing.
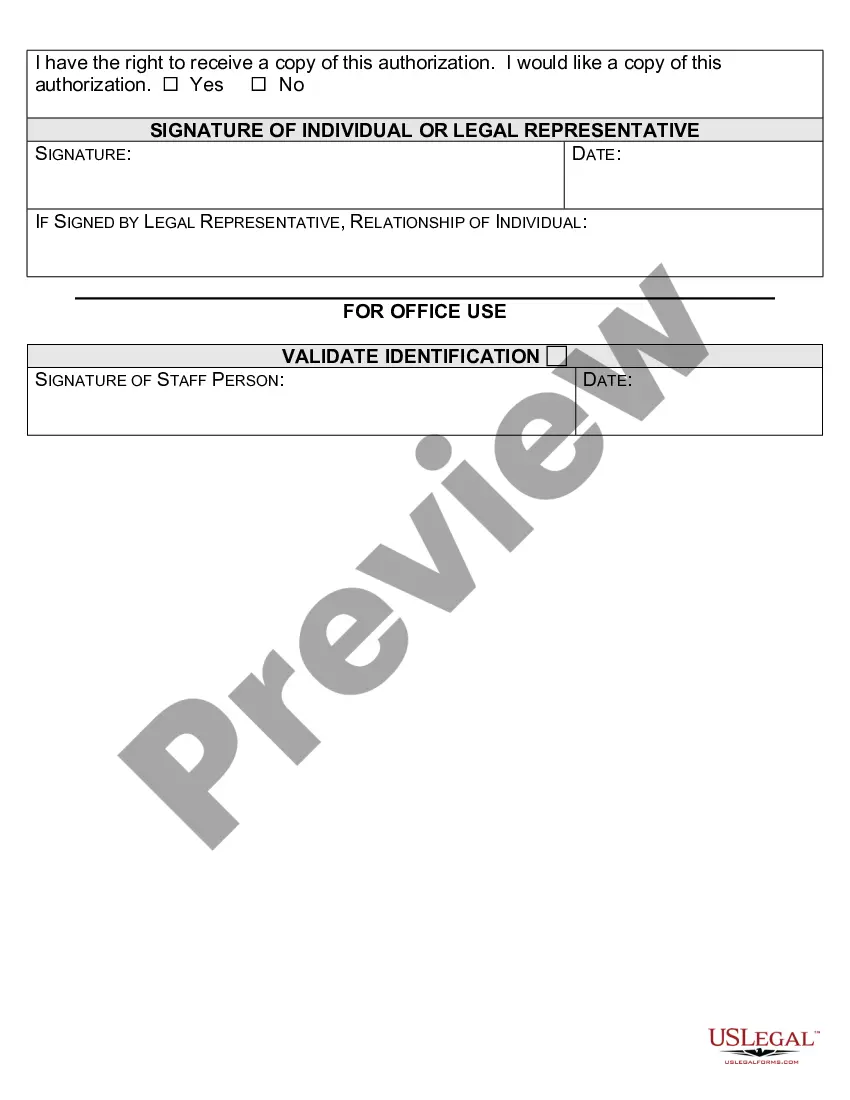
The HIPAA Privacy Rule requires that an individual provide signed authorization to a covered entity, before the entity may use or disclose certain protected health information (PHI).
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
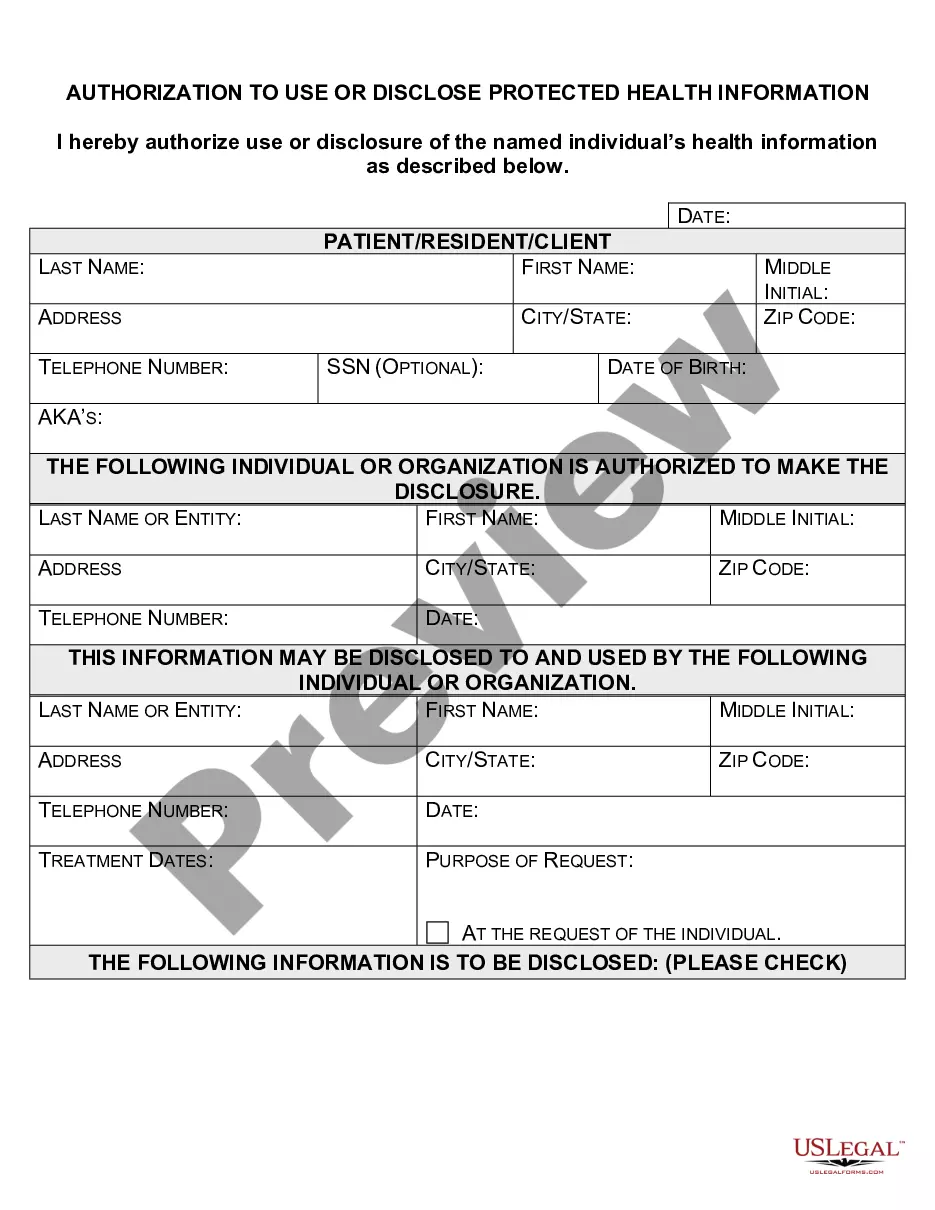
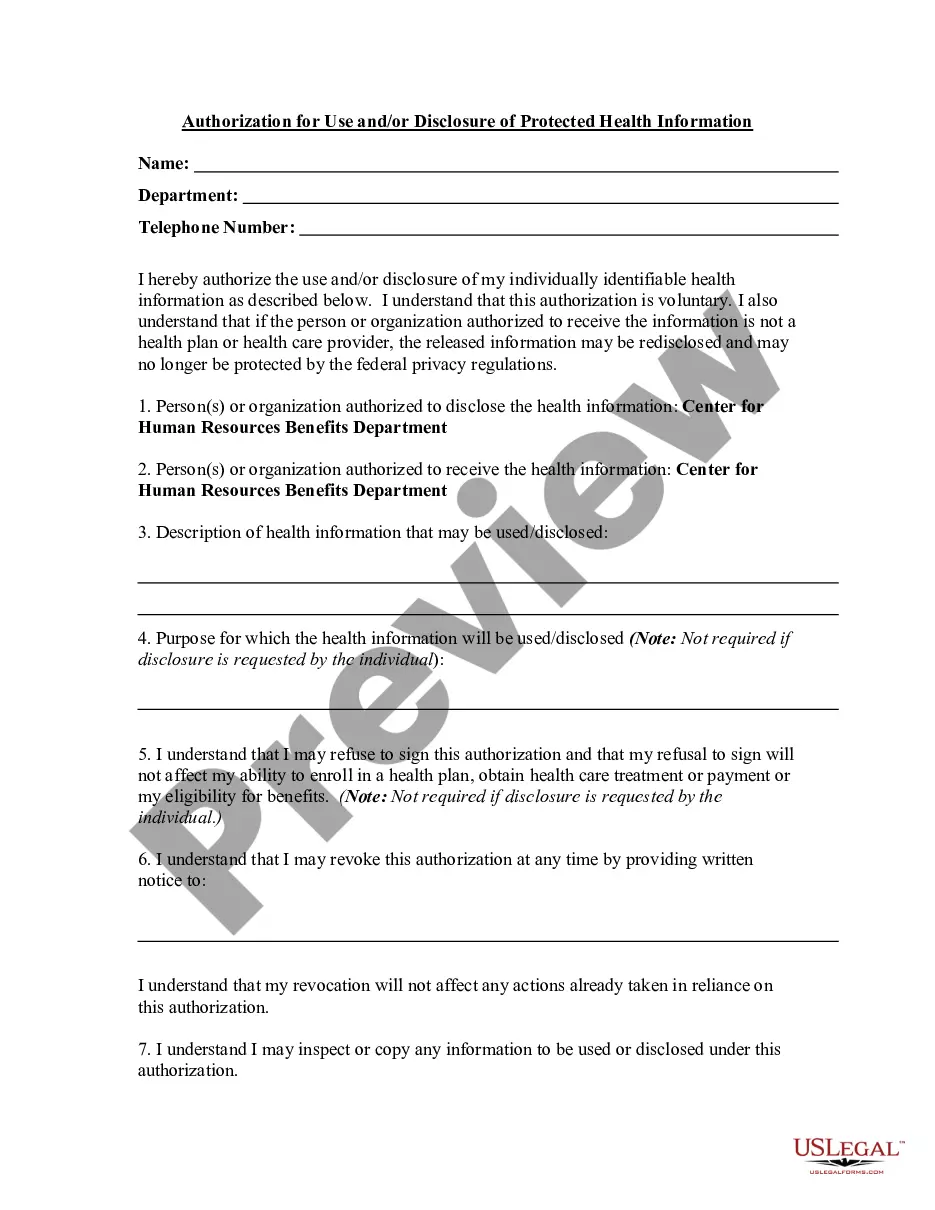
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
A patient authorization is not required for disclosure of PHI between Covered Entities if the disclosure is needed for purposes of treatment or payment or for healthcare operations. You may disclose the PHI as long as you receive a request in writing.
However, PHI can be used and disclosed without a signed or verbal authorization from the patient when it is a necessary part of treatment, payment, or healthcare operations. The Minimum Necessary Standard Rule states that only the information needed to get the job done should be provided.
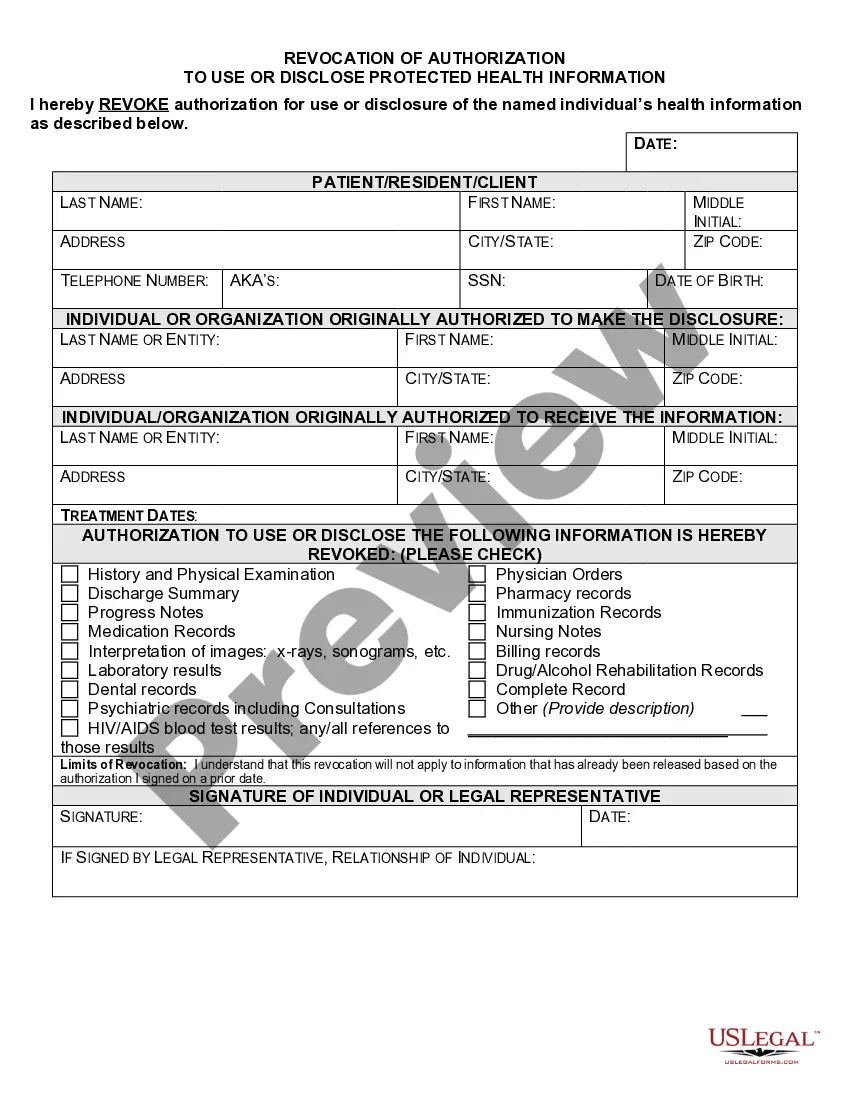
What are two required elements of an authorization needed to disclose PHI? Response Feedback: All authorizations to disclose PHI must have an expiration date and provide an avenue for the patient to revoke his or her authorization. What does the term "Disclosure" mean?
A HIPAA authorization is a detailed document in which specific uses and disclosures of protected health are explained in full. By signing the authorization, an individual is giving consent to have their health information used or disclosed for the reasons stated on the authorization.