Louisiana COBRA Continuation Coverage Election Notice
Description
How to fill out COBRA Continuation Coverage Election Notice?
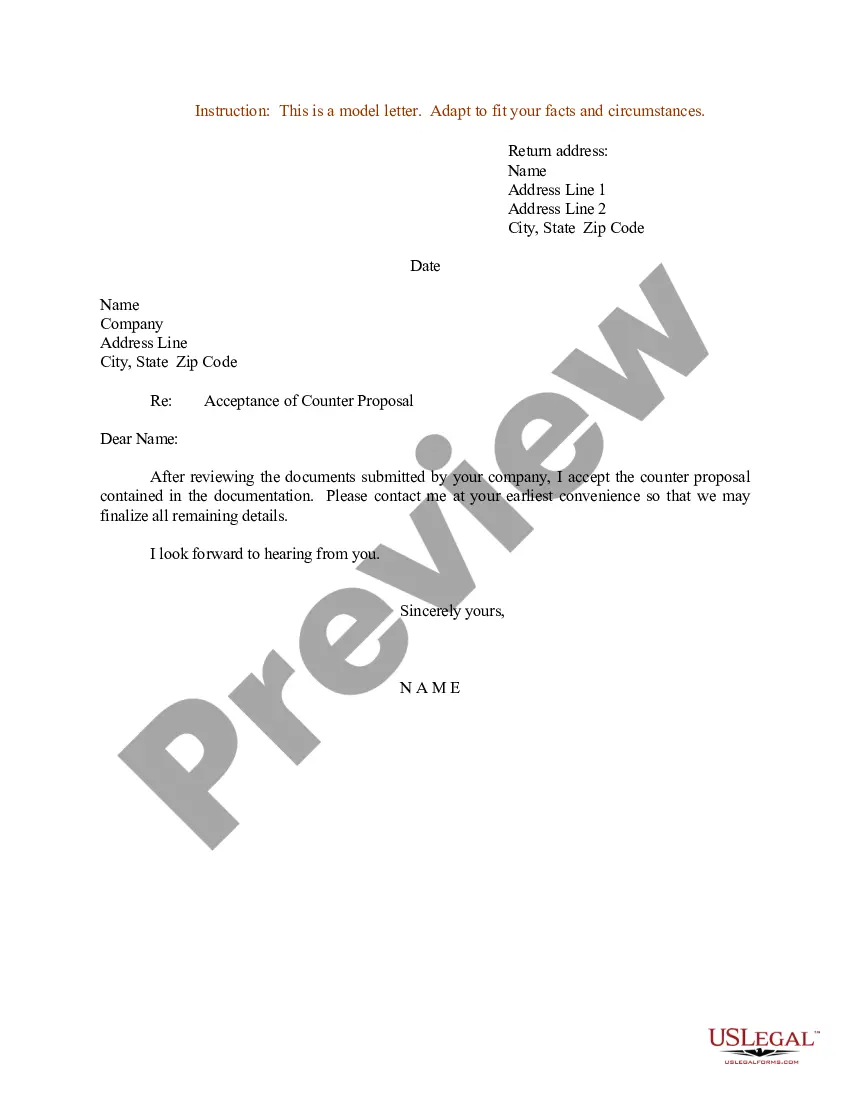
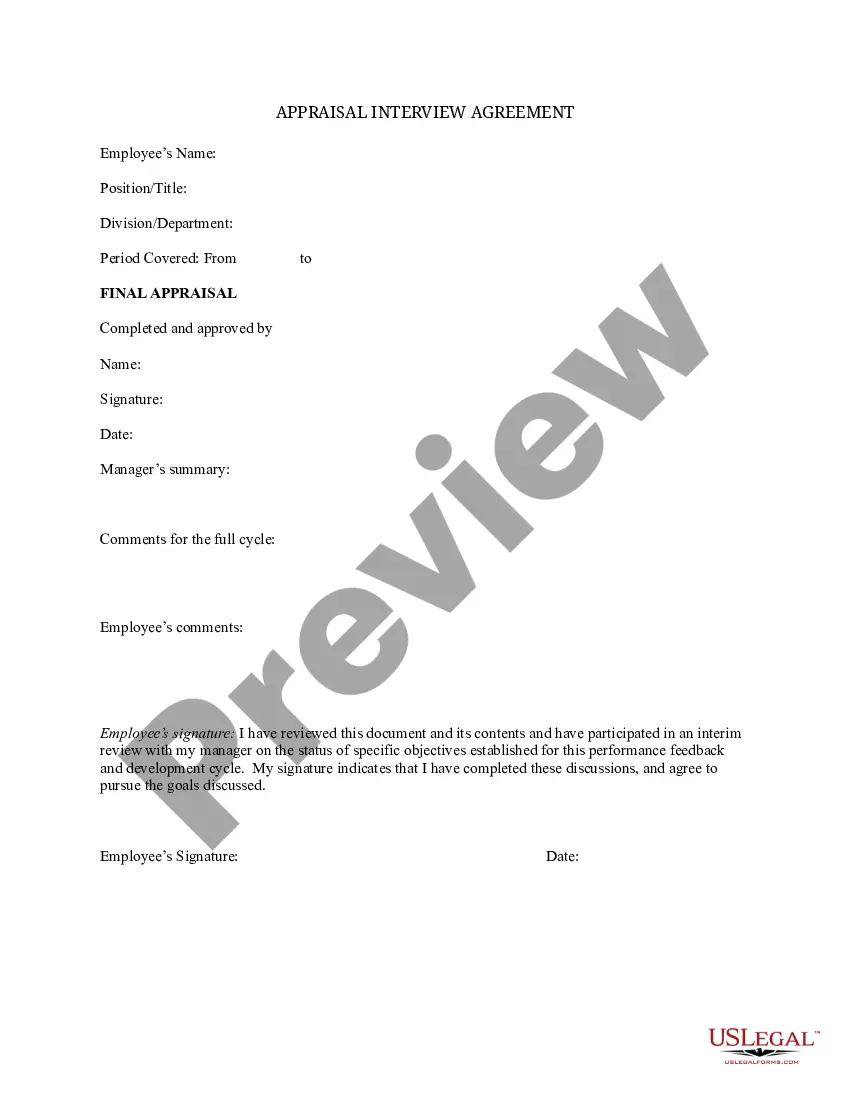
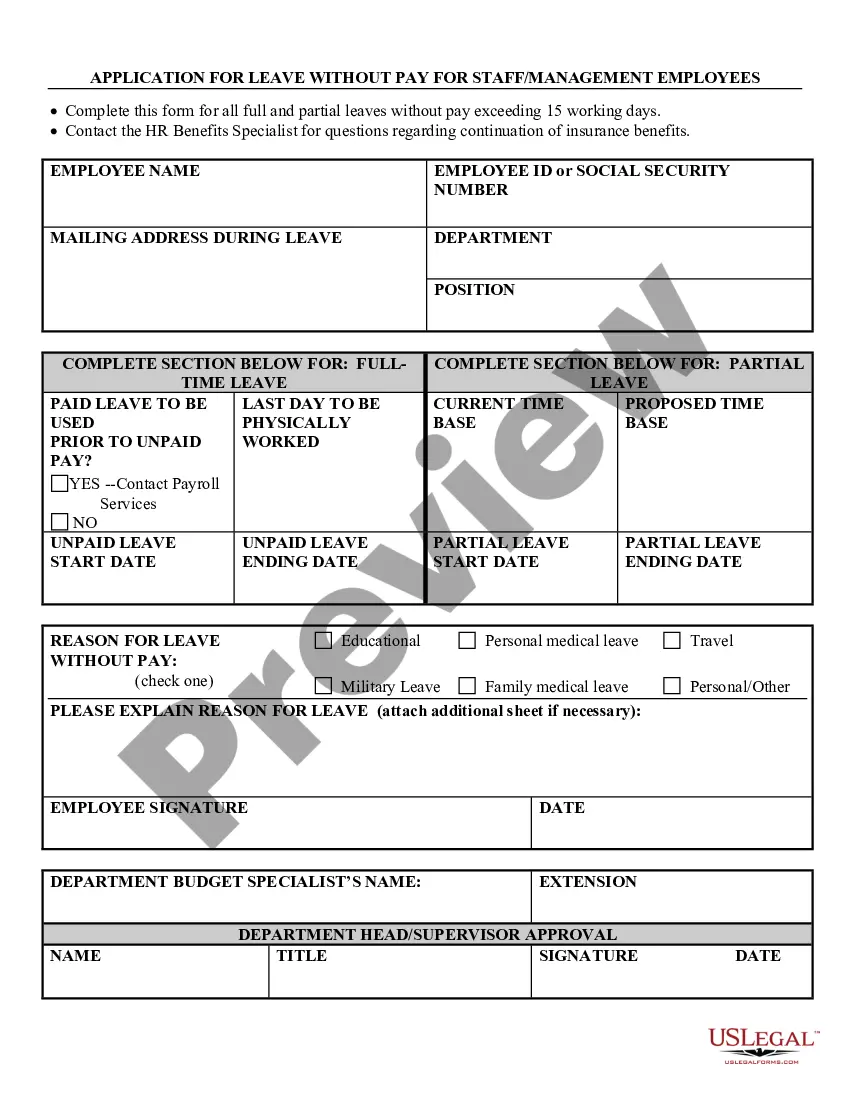
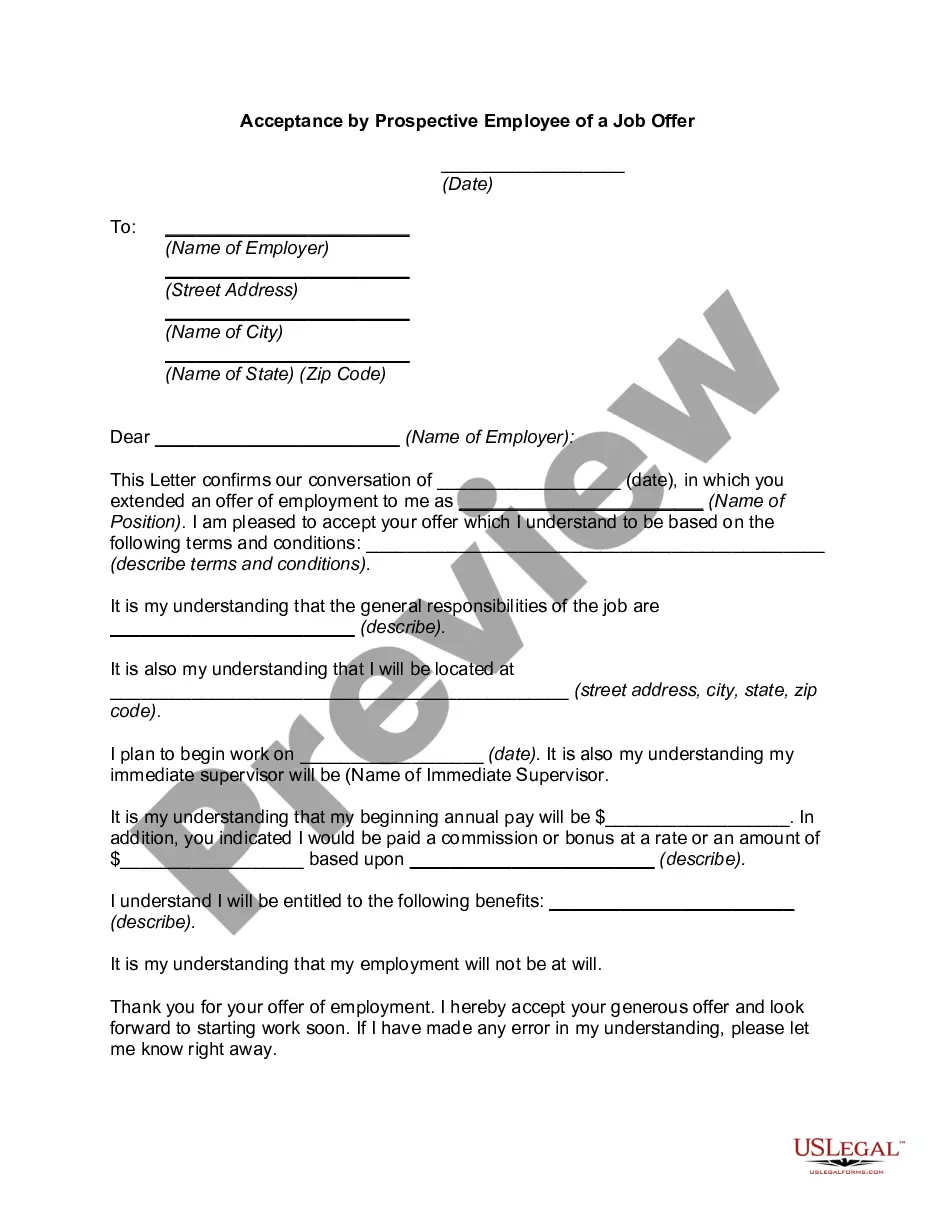
Have you ever found yourself in a situation where you need documents for either business or personal purposes almost every workday? There are many legal document templates accessible online, but finding forms you can trust is not easy.
US Legal Forms offers an extensive selection of form templates, such as the Louisiana COBRA Continuation Coverage Election Notice, designed to meet both state and federal requirements.
If you are already familiar with the US Legal Forms website and have an account, simply Log In. Then, you can download the Louisiana COBRA Continuation Coverage Election Notice template.
- Obtain the form you need, ensuring it is for the correct city/region.
- Use the Preview button to examine the form.
- Check the description to confirm you have chosen the correct form.
- If the form does not suit your needs, use the Search feature to find the form that meets your requirements.
- Once you find the appropriate form, click Get now.
- Choose the payment plan you want, fill in the necessary information to create your account, and pay for the order using your PayPal or credit card.
- Select a convenient file format and download your copy.
Form popularity
FAQ
Qualified beneficiaries may remain on COBRA insurance for up to 18 months. In the case where there is a family event, such as a divorce, legal separation, annulment or a child loses dependent status, those beneficiaries may elect continuation insurance for up to 36 months.
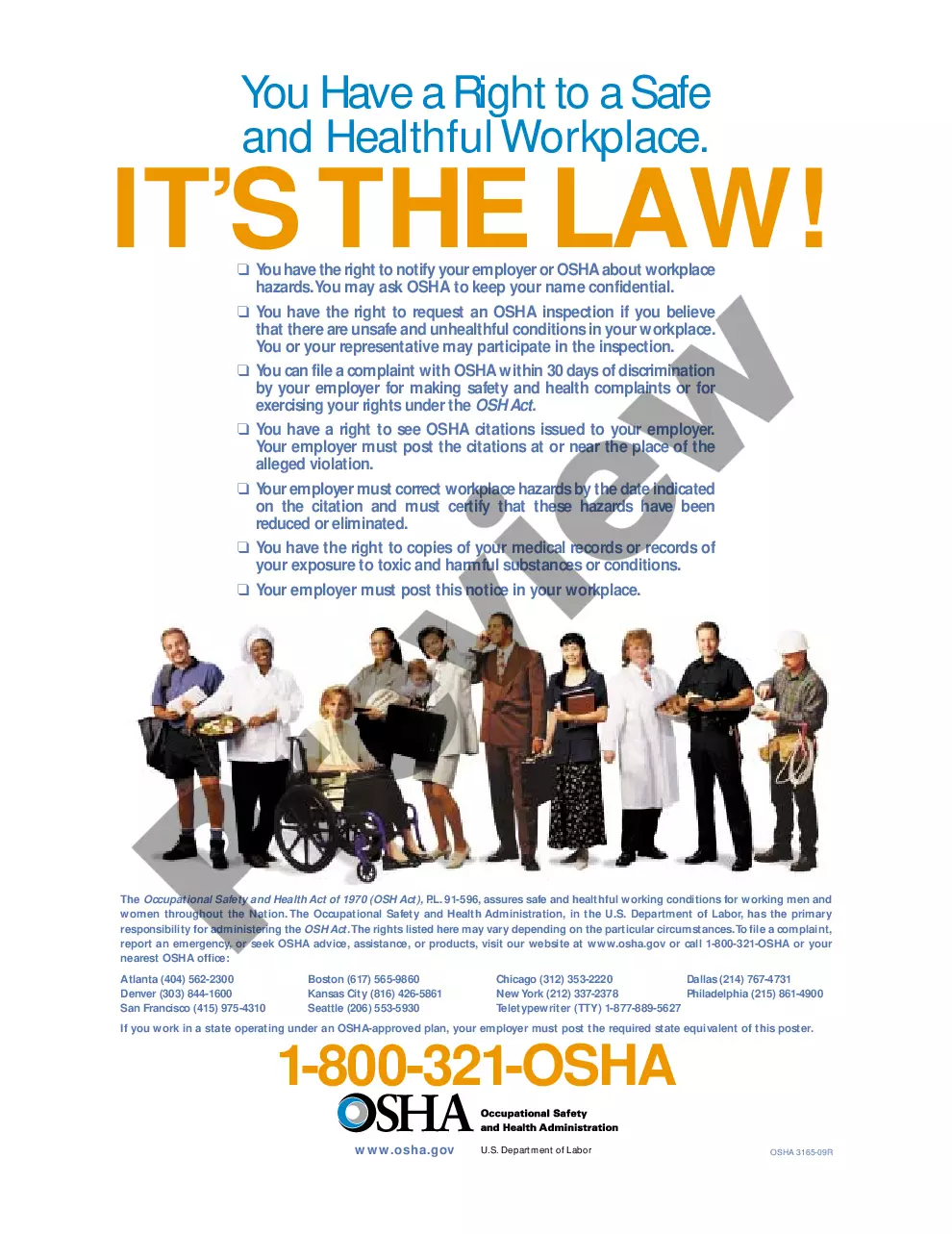
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Continuation of insurance under the group policy for any person shall terminate on the earliest of the following dates: (1) The date twelve months after the date the employee's or member's insurance under the policy would otherwise have terminated because of termination of employment or membership.
What is state continuation? State law allows employees of smaller employers (fewer than 20 employees) to keep the same group health insurance coverage for up to nine months after loss of a job or loss of coverage because of a reduction in work hours. This is called state continuation.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
The term continuation coverage refers to the extended coverage provided under the group benefit plan in which an eligible employee or eligible dependent is currently enrolled.
State continuation coverage refers to state laws that allow people to extend their employer-sponsored health insurance even if they're not eligible for extension via COBRA. As a federal law, COBRA applies nationwide, but only to employers with 20 or more employees.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.