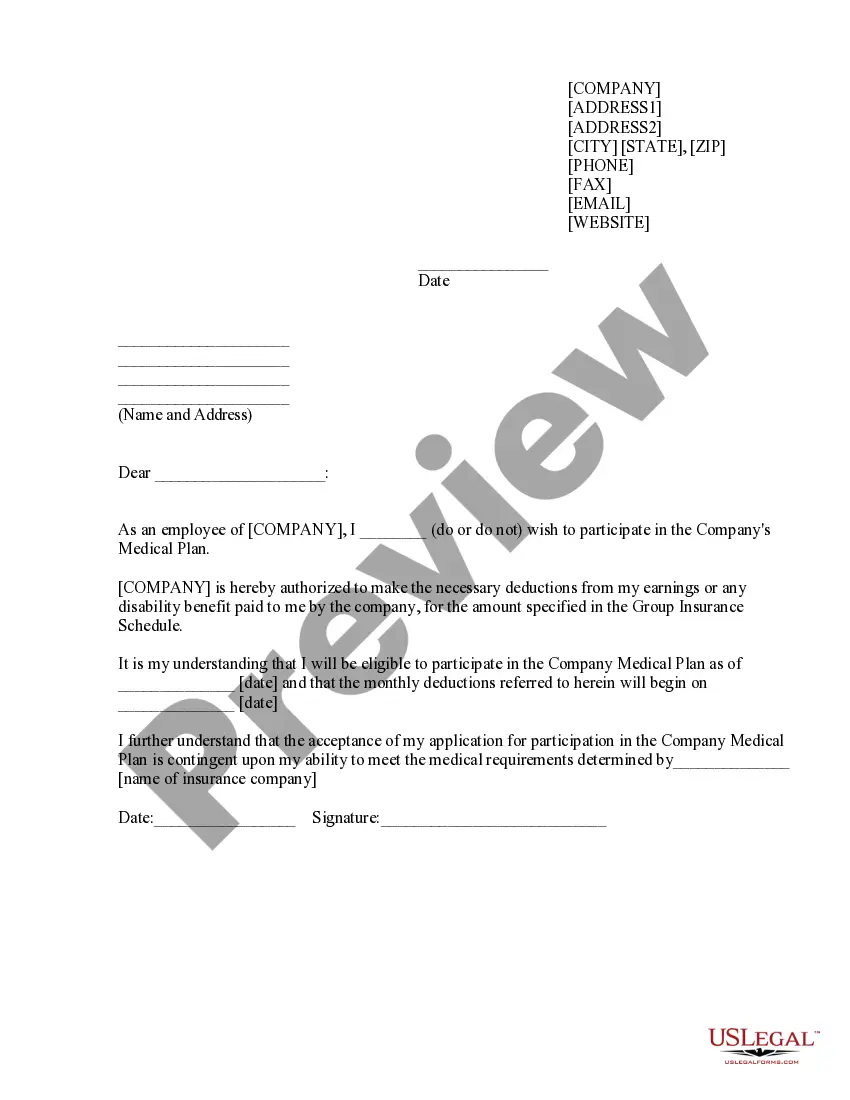
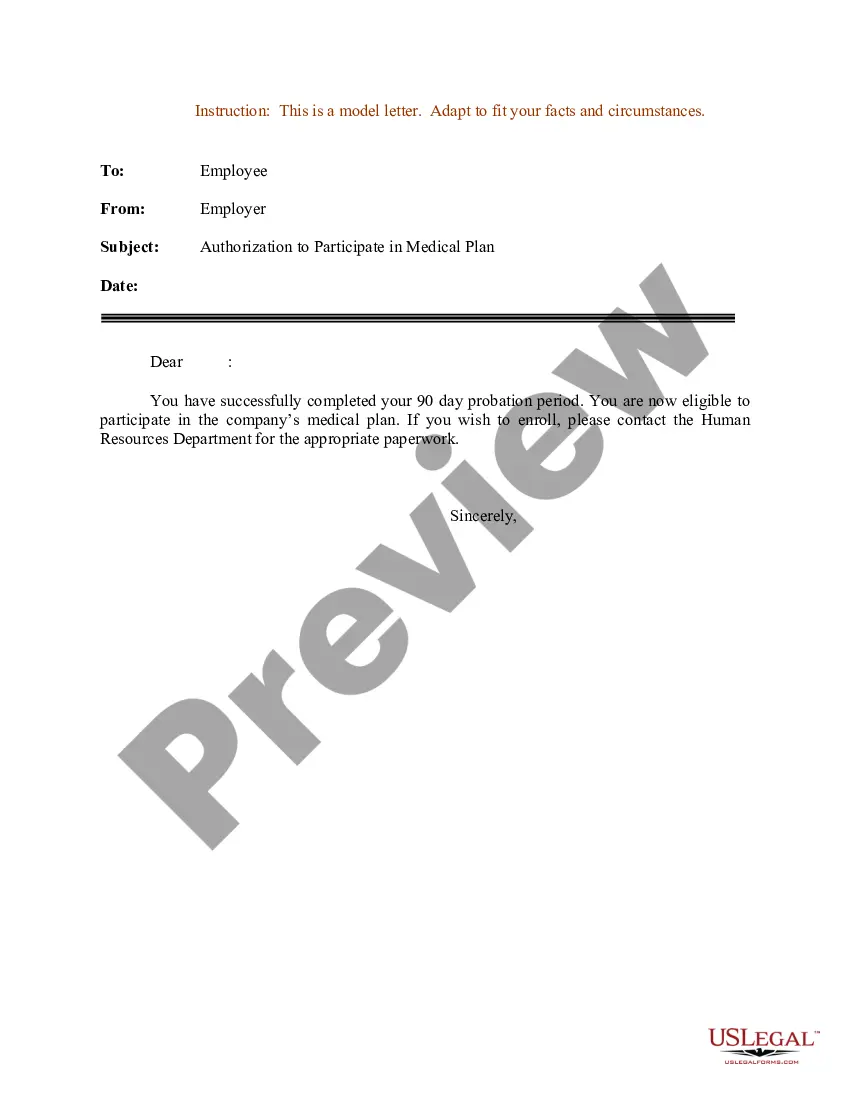
Indiana Sample Letter for Authorization to Participate in Medical Plan
Description
How to fill out Sample Letter For Authorization To Participate In Medical Plan?
Finding the appropriate legal document template can be challenging. Clearly, there are numerous templates accessible online, but how can you secure the legal document you need.
Utilize the US Legal Forms website. This service offers thousands of templates, such as the Indiana Sample Letter for Authorization to Participate in Medical Plan, which can be utilized for both business and personal purposes. All templates are reviewed by professionals and comply with federal and state requirements.
If you are already registered, Log In to your account and click the Obtain button to acquire the Indiana Sample Letter for Authorization to Participate in Medical Plan. Use your account to access the legal documents you have purchased previously. Visit the My documents tab in your account to retrieve another copy of the document you need.
Complete, modify, print, and sign the downloaded Indiana Sample Letter for Authorization to Participate in Medical Plan. US Legal Forms is the largest repository of legal templates where you can find various document templates. Take advantage of the service to obtain properly crafted documents that adhere to state regulations.
- Firstly, ensure you have selected the correct form for your city/region.
- You can preview the form using the Review button and read the form description to confirm it is the right one for you.
- If the form does not meet your requirements, use the Search field to find the appropriate form.
- Once you are confident that the form is suitable, click the Acquire now button to obtain the form.
- Choose the pricing plan you prefer and enter the necessary details. Create your account and complete your purchase using your PayPal account or credit card.
- Select the file format and download the legal document template to your device.
Form popularity
FAQ
To apply for Medicaid and food stamps in Indiana, visit the Indiana Family and Social Services Administration's online portal or a local office. Completing a single application will allow you to apply for both programs. Remember that the Indiana Sample Letter for Authorization to Participate in Medical Plan can help present your case clearly when seeking assistance.
Applying for health coverage in Indiana involves completing an online application through the Indiana Family and Social Services Administration's website or via healthcare. You will need to provide personal information, income details, and possibly documentation to support your application. Incorporating the Indiana Sample Letter for Authorization to Participate in Medical Plan can help clarify your needs during this process.
The income limit for Medicaid in Indiana varies depending on family size and the specific program you are applying for, such as Traditional Medicaid or the Healthy Indiana Plan. It's essential to check the latest guidelines on the Indiana state website or consult a local representative for accurate information. The Indiana Sample Letter for Authorization to Participate in Medical Plan can also provide helpful context for your income determination.
For Medicaid provider enrollment in Indiana, you can contact the Indiana Family and Social Services Administration at 1-800-457-4584. This number connects you to assistance regarding enrollment and eligibility questions. Having documents ready, including the Indiana Sample Letter for Authorization to Participate in Medical Plan, can streamline your interaction.
To obtain government health insurance, start by exploring programs like Medicaid and the Children’s Health Insurance Program (CHIP). You can visit the official state website or healthcare for detailed information on eligibility and application procedures. Additionally, using resources like the Indiana Sample Letter for Authorization to Participate in Medical Plan can help support your application process.
Medicaid does require prior authorization for many services in Indiana, designed to ensure that all care aligns with established guidelines and is medically necessary. This process helps to manage costs and ensures quality of care. Utilizing the Indiana Sample Letter for Authorization to Participate in Medical Plan can enhance your application, ensuring all necessary details are conveyed clearly and effectively.
Yes, traditional Indiana Medicaid typically requires prior authorization for various procedures and services. This step ensures that the proposed services align with medical necessity and Medicaid standards. Providing a comprehensive Indiana Sample Letter for Authorization to Participate in Medical Plan can greatly assist in navigating the prior authorization process smoothly.
To apply for state insurance in Indiana, individuals should complete an online application through the Indiana Family and Social Services Administration website. It's crucial to provide accurate information and gather necessary documentation ahead of time. Additionally, having the Indiana Sample Letter for Authorization to Participate in Medical Plan can help clarify intentions and support the application process effectively.
Certain services, such as routine check-ups and preventive care, often do not require prior authorization under Indiana Medicaid. However, this can vary by plan, so it's essential to verify specific requirements. Familiarizing yourself with the Indiana Sample Letter for Authorization to Participate in Medical Plan can clarify which services require authorization and assist in the overall understanding of the process.
A prior authorization request form is a document that healthcare providers submit to insurance companies or Medicaid to obtain approval for specific services or medications before they are rendered. This form typically requires detailed information regarding the patient's medical history and the necessity of the requested service. Utilizing the Indiana Sample Letter for Authorization to Participate in Medical Plan can help streamline this process by ensuring all pertinent information is included.