Florida Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
Are you currently in a role where you often require documents for either business or personal reasons? There is a wide array of legal document templates accessible online, but finding reliable ones can be challenging.
US Legal Forms provides a vast collection of form templates, including the Florida Notice of Qualifying Event from Employer to Plan Administrator, which can be filled out to comply with state and federal regulations.
If you are already familiar with the US Legal Forms website and possess an account, simply Log In. After that, you can download the Florida Notice of Qualifying Event from Employer to Plan Administrator template.
Access all of the document templates you have purchased in the My documents section. You can obtain another copy of the Florida Notice of Qualifying Event from Employer to Plan Administrator at any time if needed. Simply select the desired form to download or print the document template.
Utilize US Legal Forms, the most extensive collection of legal documents, to save time and prevent errors. The service offers professionally crafted legal document templates that you can use for various purposes. Create an account on US Legal Forms and start making your life a bit more manageable.
- Obtain the form you require and ensure it is for the correct locale.
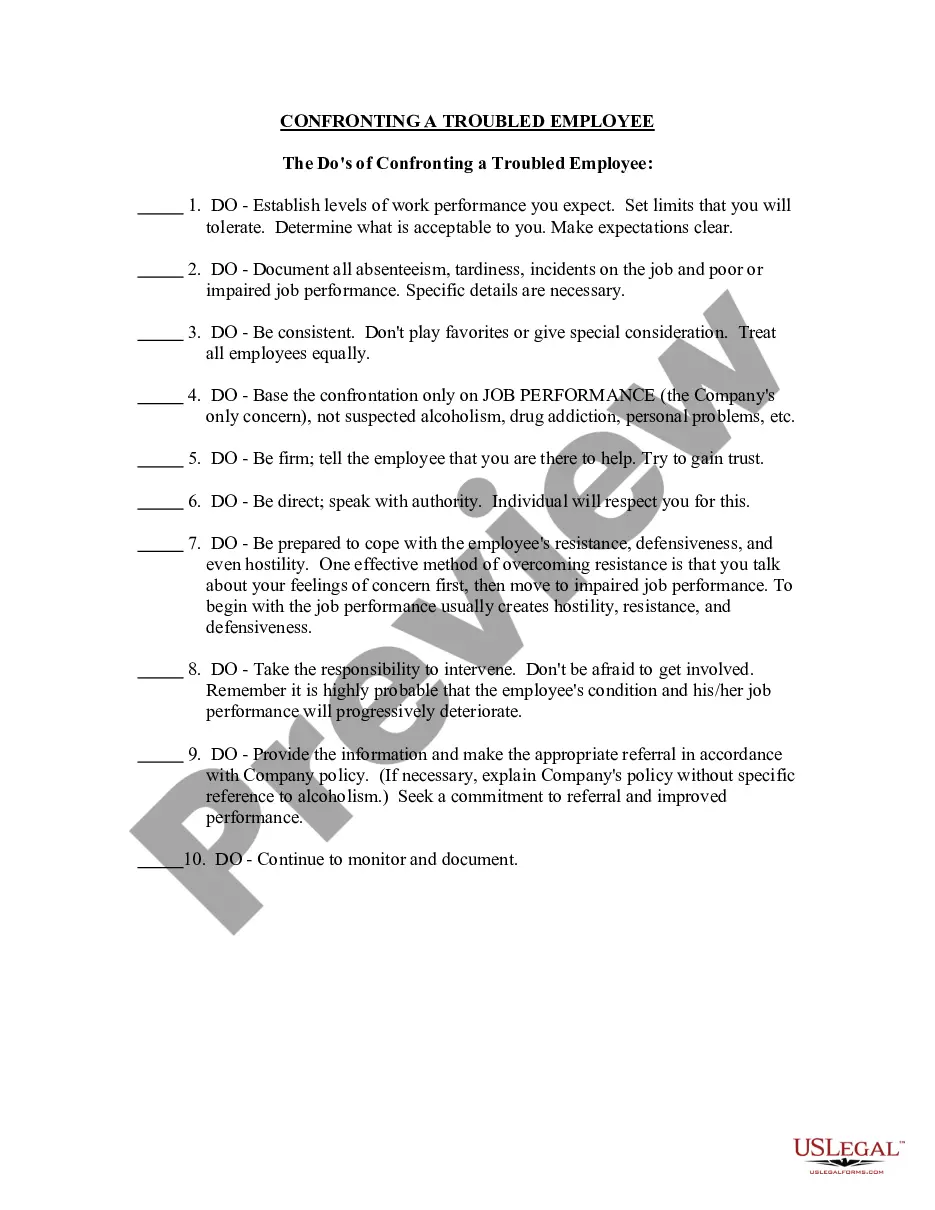
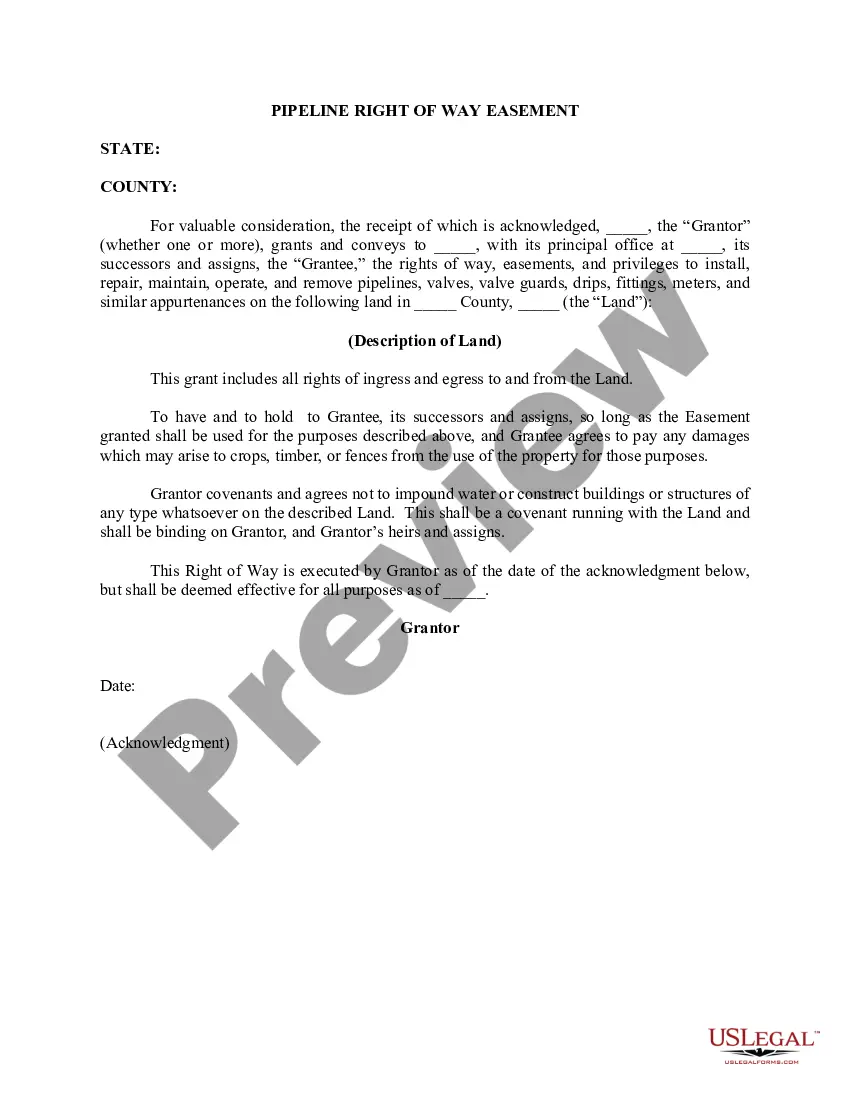
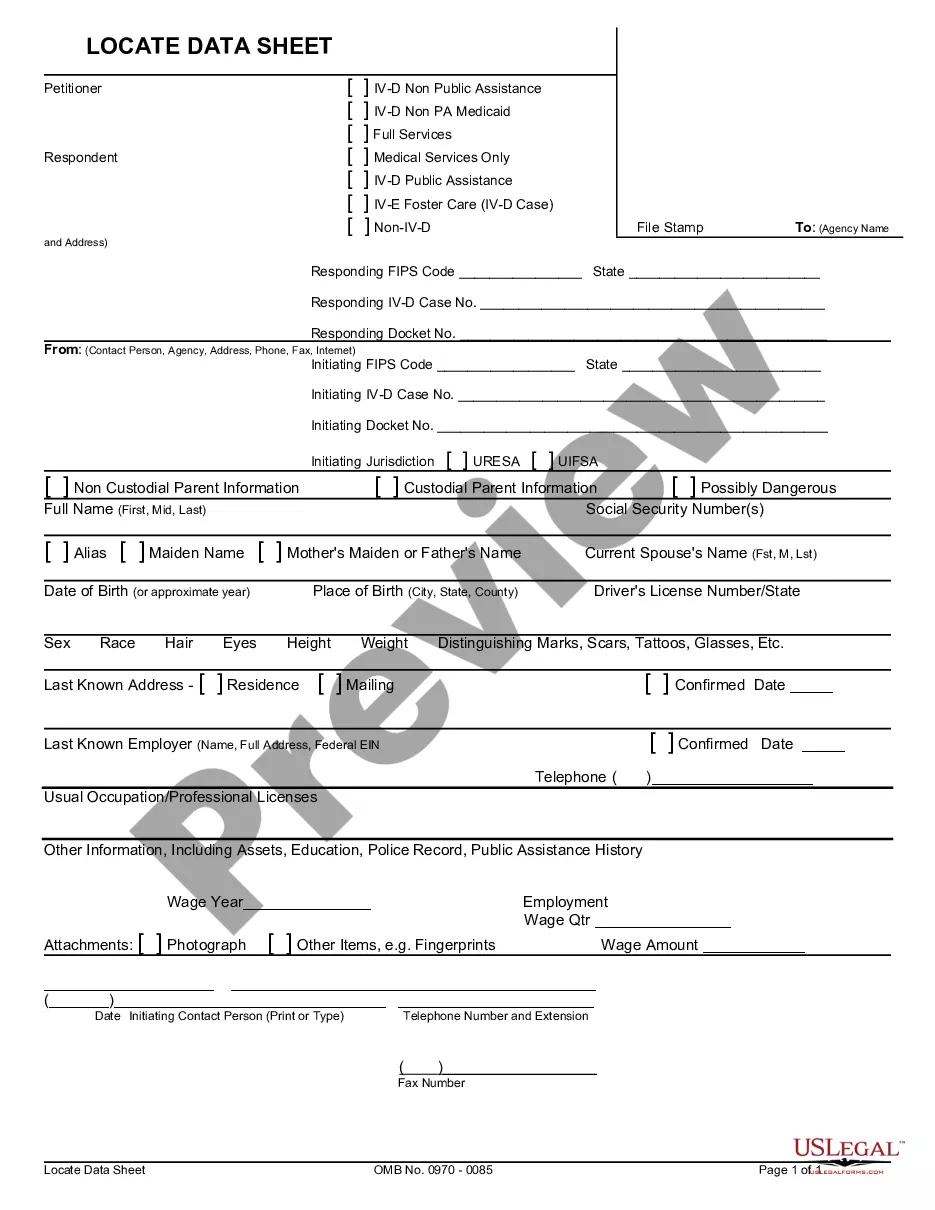
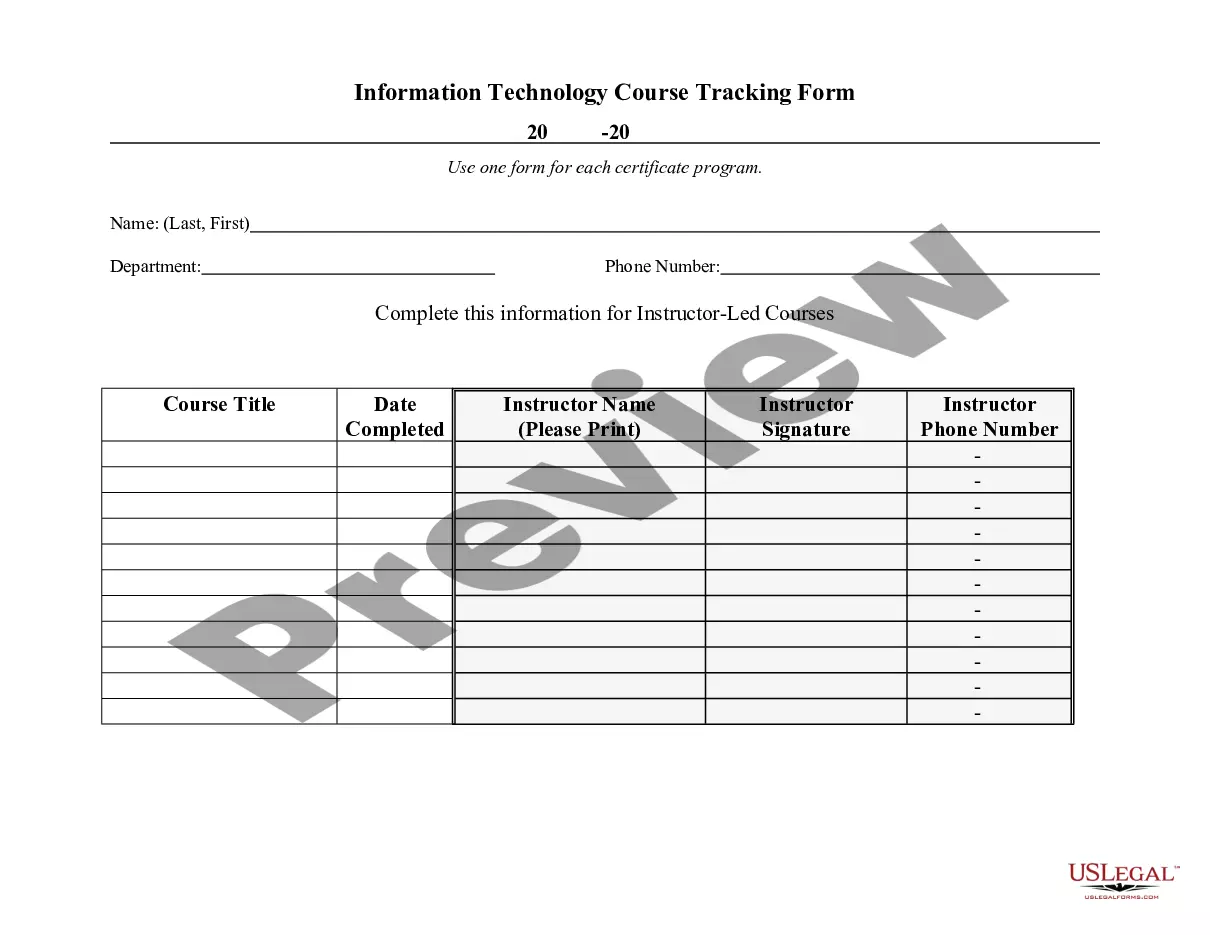
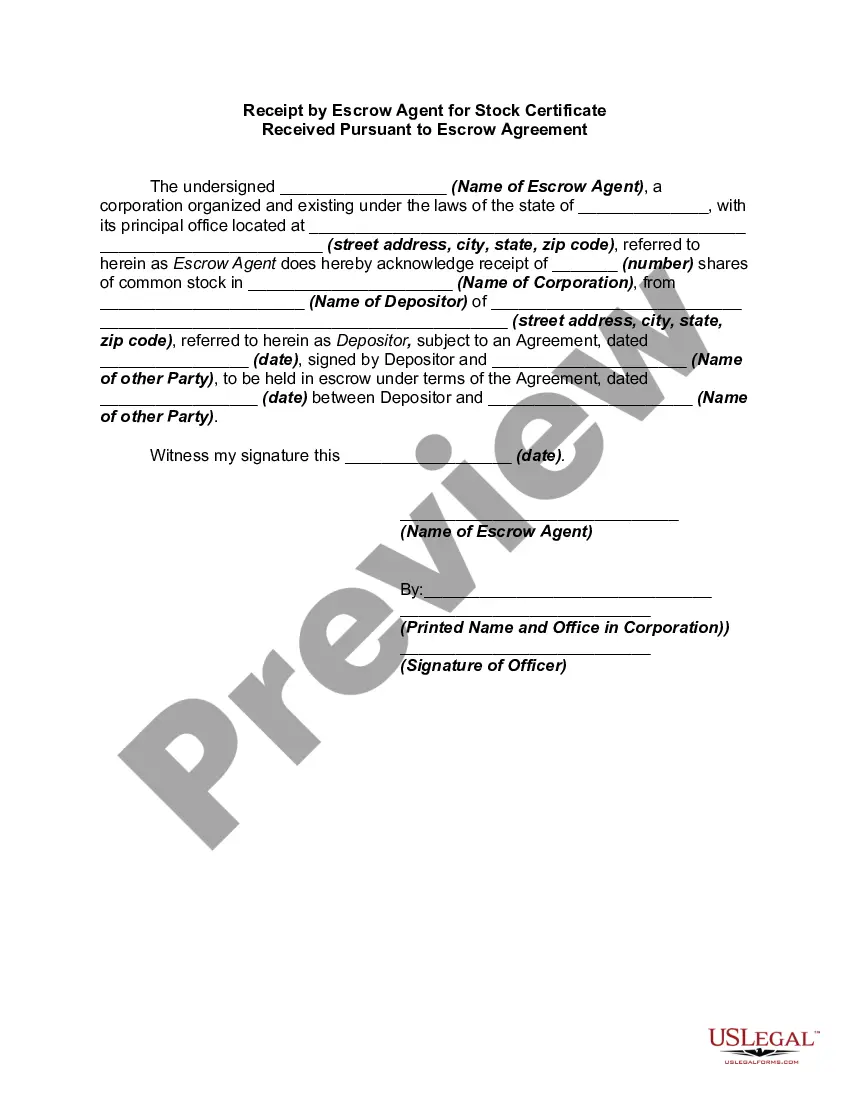
- Utilize the Preview feature to review the form.
- Examine the details to confirm you have selected the correct document.
- If the form isn’t what you’re looking for, use the Search field to find the form that meets your needs.
- Once you locate the appropriate form, click on Purchase now.
- Select the pricing plan you prefer, fill in the necessary information to create your account, and complete the purchase using PayPal or a credit card.
- Choose a convenient document format and download your copy.
Form popularity
FAQ
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
For example, the Florida Health Care Access Act requires that any employee signing up for insurance provide a full and accurate disclosure statement.
The exact number of hours can change from law-to-law. For example, to be covered by the Affordable Care Act (ACA or 'Obamacare'), an employee must work for 35 hours each week, but to be covered under relevant Florida health care statue, an employee only needs to work 20 hours a week.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Florida does not require employers to provide health care benefits to their employees. If an employer does provide health benefits, the state's insurance laws require plans to cover certain mandated benefits as defined by the federal Affordable Care Act (ACA).
Florida Healthcare Insurance: What you need to knowThere is no state law requiring employers to offer group healthcare insurance to their employees, but most employers do provide this benefit.
Florida's state continuation or mini-COBRA law provides similar continuation of coverage protection for employees who work for employers with two to 19 employees. Once you elect mini-COBRA coverage, you will pay 100% of the total insurance premium plus a 15% processing fee.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under