California General Notice of Preexisting Condition Exclusion
Description
How to fill out General Notice Of Preexisting Condition Exclusion?
It is feasible to spend hours online trying to locate the valid document template that meets the state and federal standards you need.
US Legal Forms offers thousands of valid forms that are reviewed by professionals.
You can download or print the California General Notice of Preexisting Condition Exclusion from our platform.
If you are using the US Legal Forms website for the first time, follow the simple instructions below: First, ensure you have selected the correct document template for your location/city.
Review the form description to ensure you have selected the suitable form.
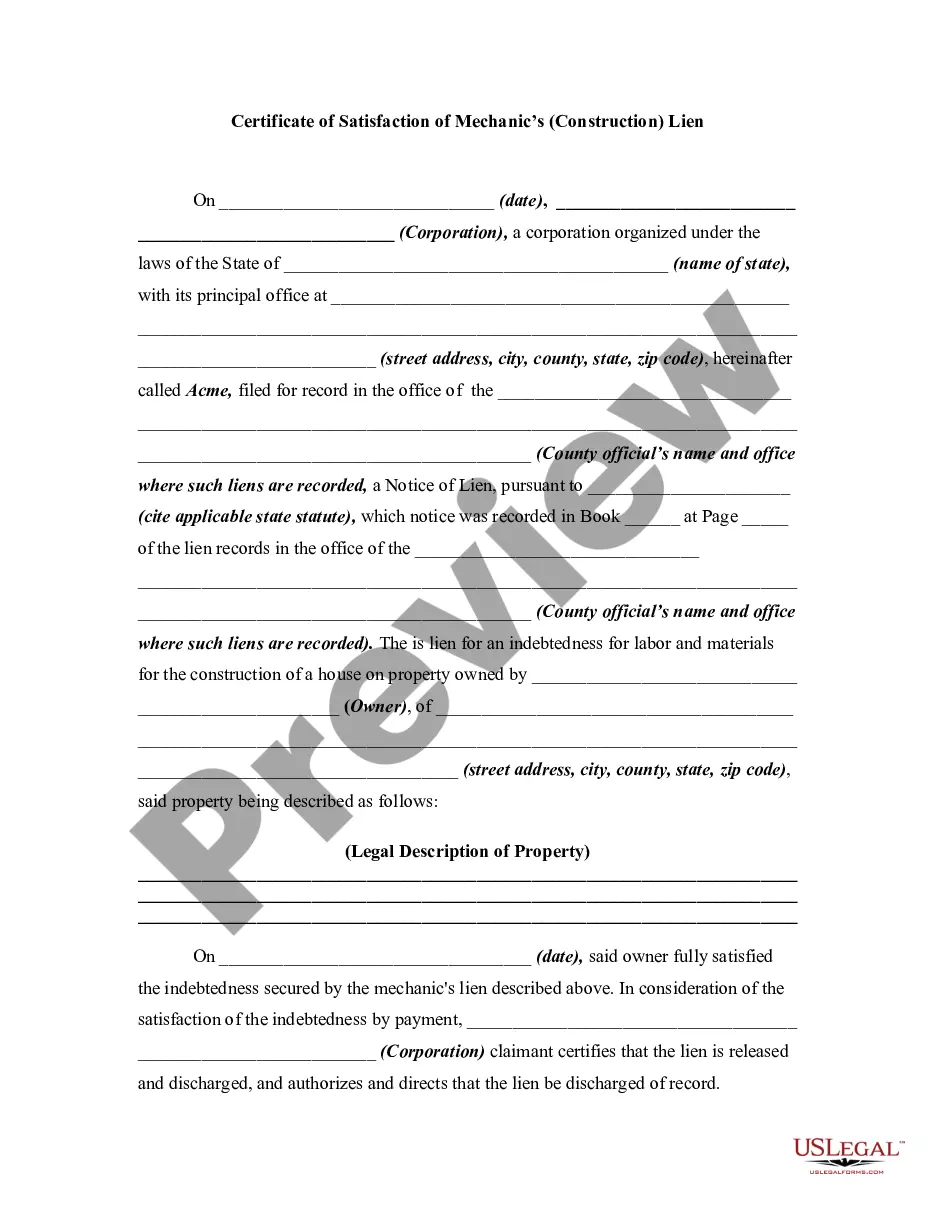
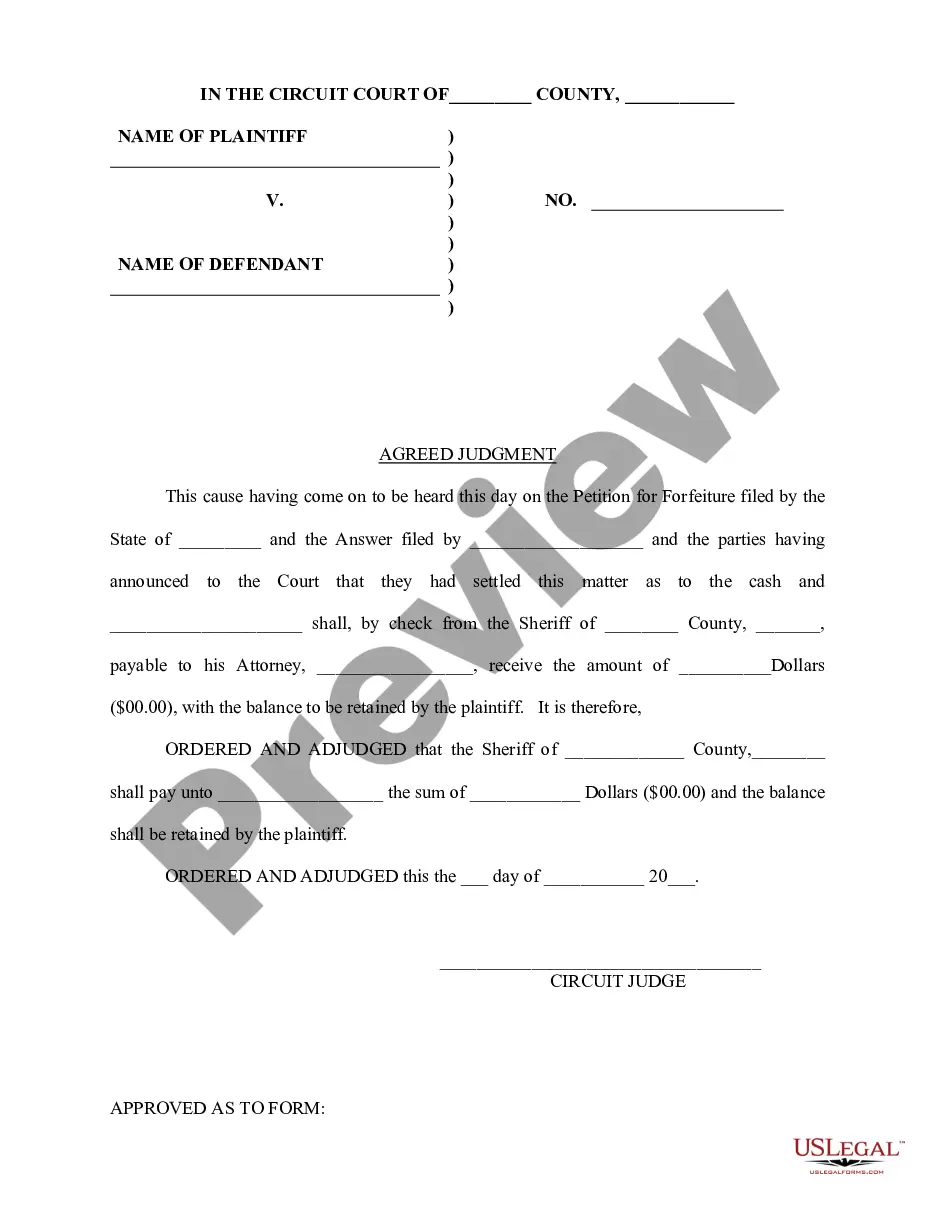
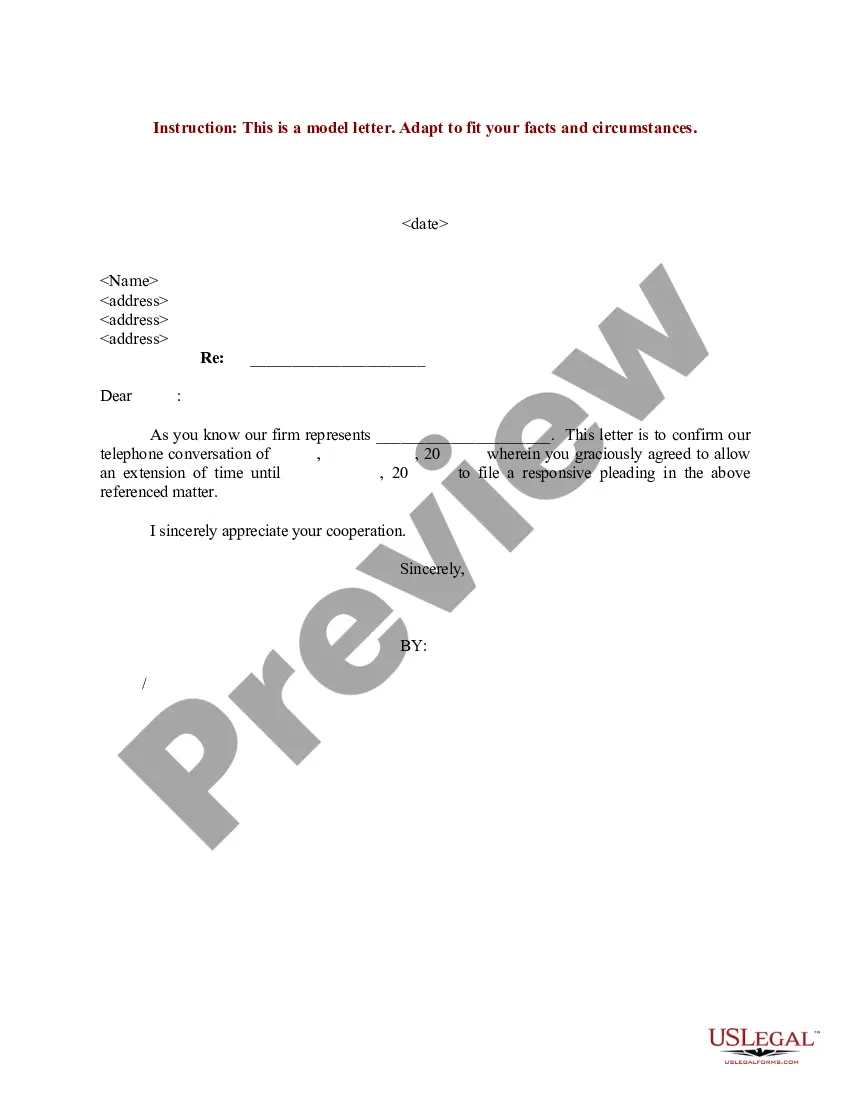
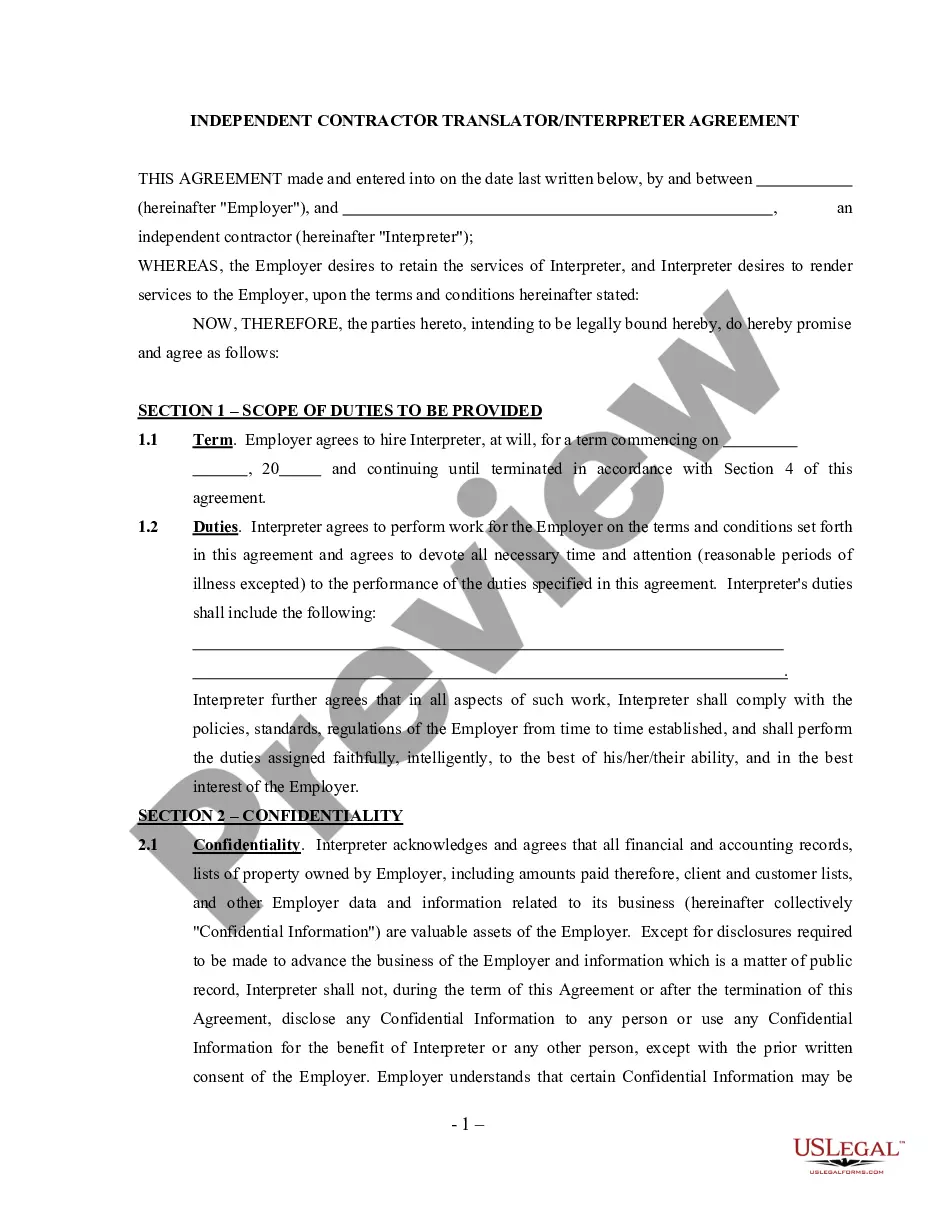
If available, utilize the Review button to view the document template as well.
To find another version of the form, take advantage of the Search field to locate the template that fits your needs and requirements.
Once you have found the template you want, click Acquire now to proceed.
Select the pricing plan you prefer, enter your credentials, and register for a free account on US Legal Forms.
Complete the purchase. You can use your credit card or PayPal account to pay for the valid form.
Choose the format of the document and download it to your device.
Make changes to the document if necessary. You can complete, edit, and sign and print the California General Notice of Preexisting Condition Exclusion.
Obtain and print thousands of document templates using the US Legal Forms website, which offers the largest variety of valid forms.
Utilize professional and state-specific templates to manage your business or personal needs.
- If you already have a US Legal Forms account, you can Log In and then click the Obtain button.
- After that, you can complete, modify, print, or sign the California General Notice of Preexisting Condition Exclusion.
- Each valid document template you acquire is yours permanently.
- To obtain another copy of any purchased form, go to the My documents section and click the corresponding button.
Form popularity
FAQ
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
The Patient Protection and Affordable Care Act changed that. If you have a pre-existing medical condition, you can't be denied health insurance coverage and you won't have to pay more because of it.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
In California, group health plans can limit or exclude coverage for pre-existing conditions for adults (age 19 and older) for up to six months from the date coverage begins.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
If you had a pre-existing condition exclusion period, you didn't have coverage for any care or services related to your pre-existing condition for a predetermined amount of time, despite paying your monthly premiums.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.