California Individual Notice of Preexisting Condition Exclusion
Description
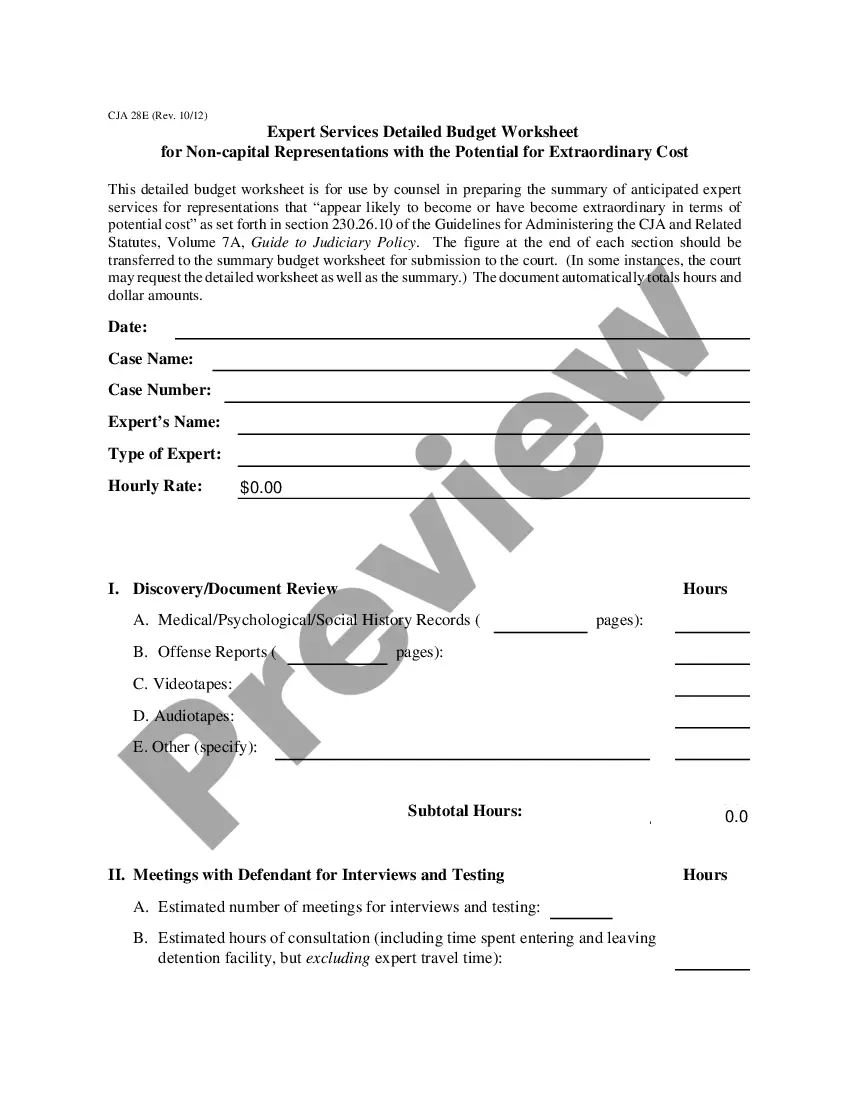
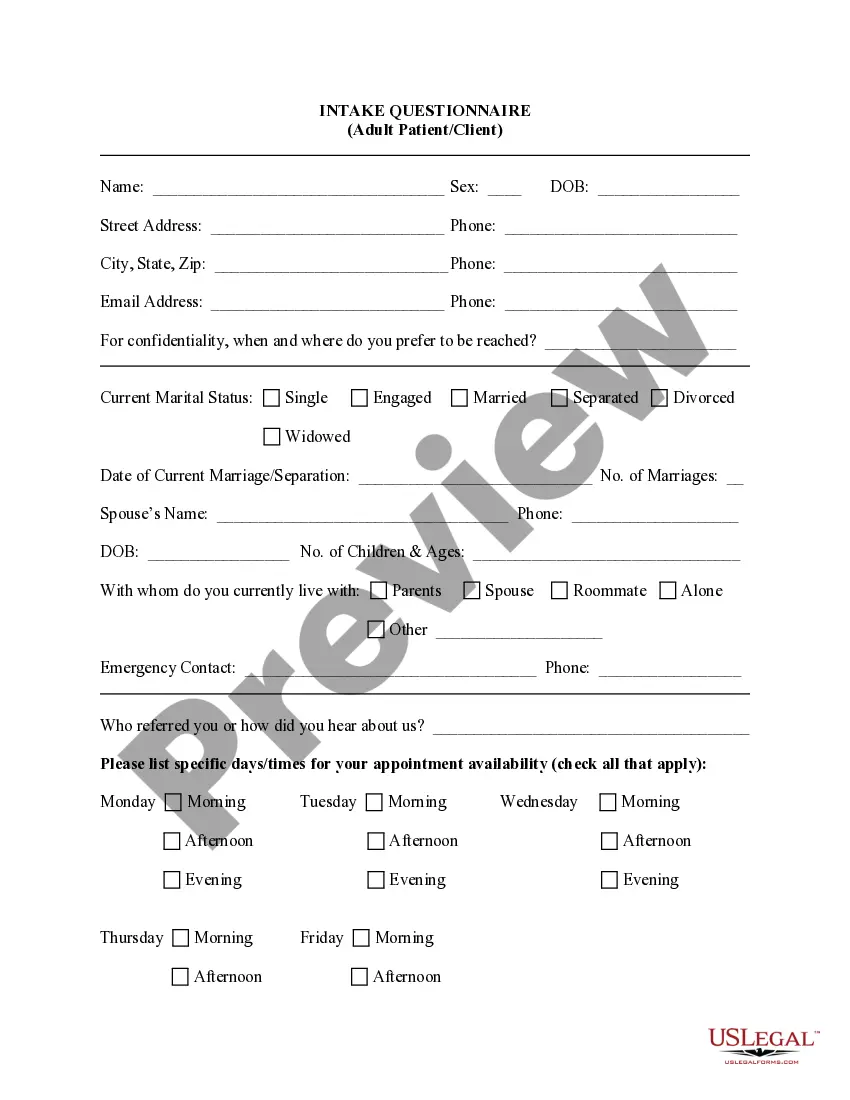
How to fill out Individual Notice Of Preexisting Condition Exclusion?
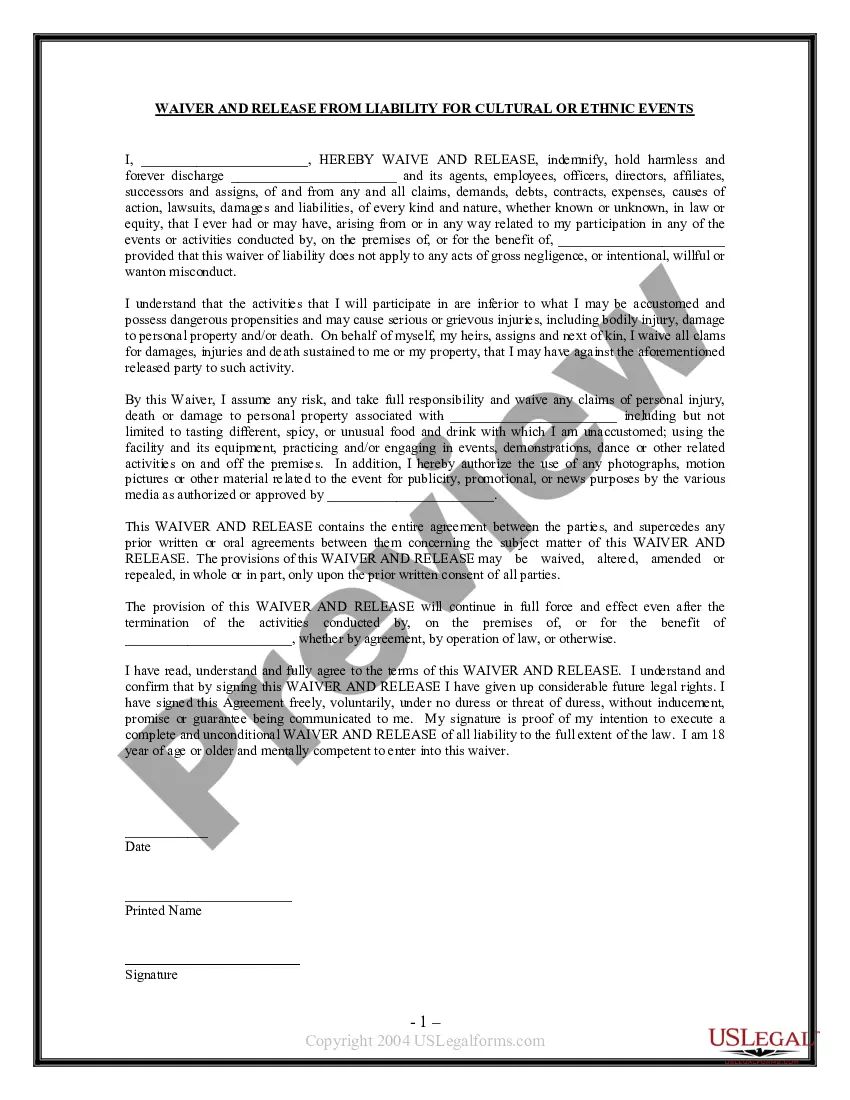
Selecting the appropriate legal document design can be challenging.
Clearly, there are numerous templates accessible online, but how can you secure the legal form you desire? Utilize the US Legal Forms website.
The platform offers thousands of templates, including the California Individual Notice of Preexisting Condition Exclusion, which can be used for business and personal needs. All the forms are reviewed by professionals and comply with federal and state regulations.
Once you are confident that the form is appropriate, click the Get now button to acquire the form. Choose the pricing plan you want and provide the necessary information. Create your account and place your order using your PayPal account or Visa or Mastercard. Select the document format and download the legal document template to your system. Finally, complete, modify, print, and sign the obtained California Individual Notice of Preexisting Condition Exclusion. US Legal Forms is the largest collection of legal documents where you can find various paper templates. Use the service to download professionally crafted documents that adhere to state requirements.
- If you are already registered, Log In to your account and click the Download button to access the California Individual Notice of Preexisting Condition Exclusion.
- Use your account to search through the legal forms you have previously purchased.
- Go to the My documents tab in your account and retrieve another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple guidelines you can follow.
- First, make sure you have selected the correct form for your area/state. You can view the form using the Preview button and read the form description to ensure it is suitable for you.
- If the form does not fulfill your requirements, use the Search section to find the right form.
Form popularity
FAQ
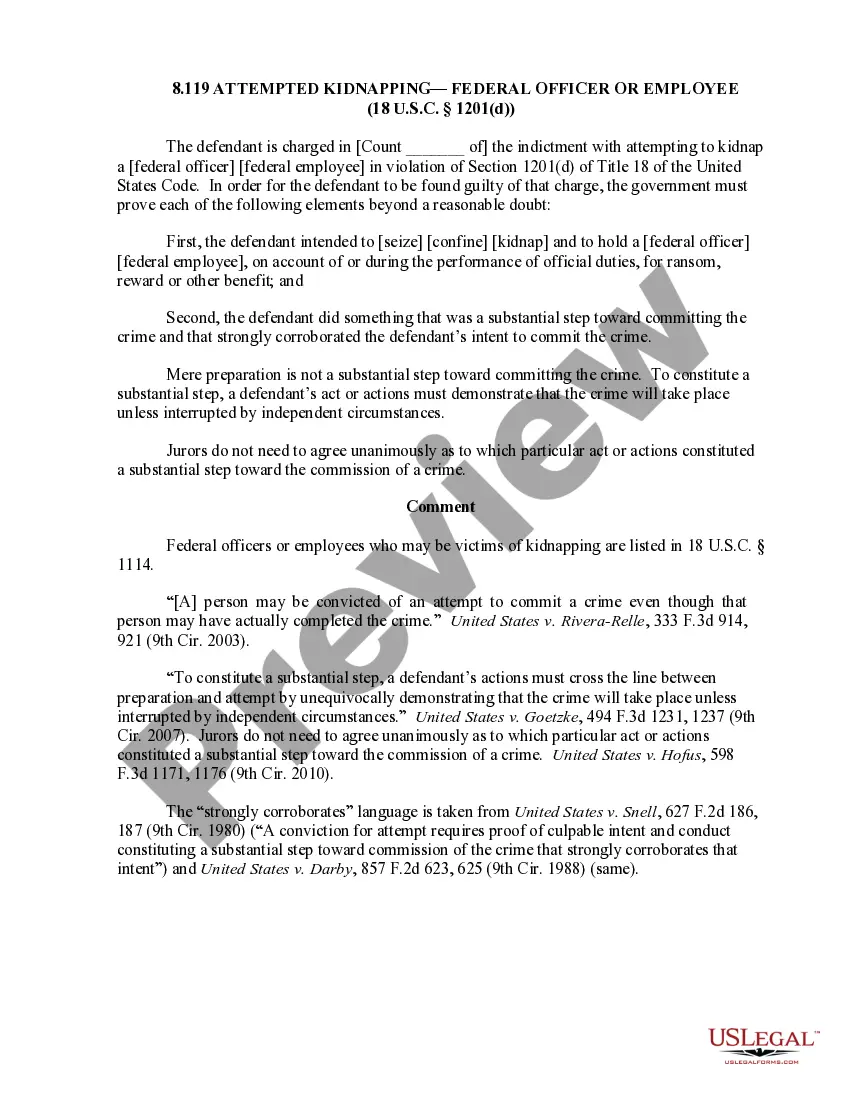
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
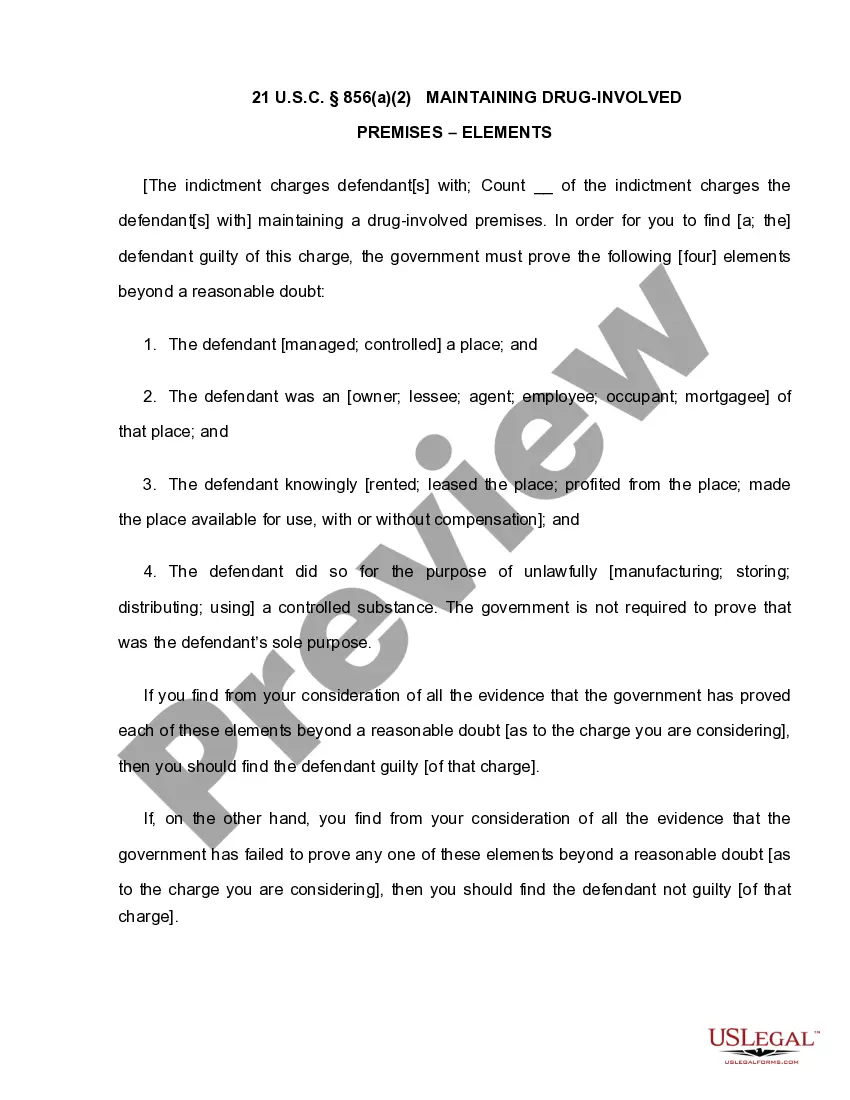
There might be a scenario's where system determines records for more than one condition type in the pricing procedure. In order to avoid this we can set up conditions or a group of conditions to be mutually exclusive. This is called condition exclusion.
Examples of pre-existing conditions include cancer, asthma, diabetes, and even pregnancy. Under the Affordable Care Act (Obamacare), health insurance companies cannot refuse to cover you because of any pre-existing conditions nor can they charge you more money for coverage or subject you to a waiting period.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions. They tend to be chronic or long-term.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
In California, group health plans can limit or exclude coverage for pre-existing conditions for adults (age 19 and older) for up to six months from the date coverage begins.