California Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
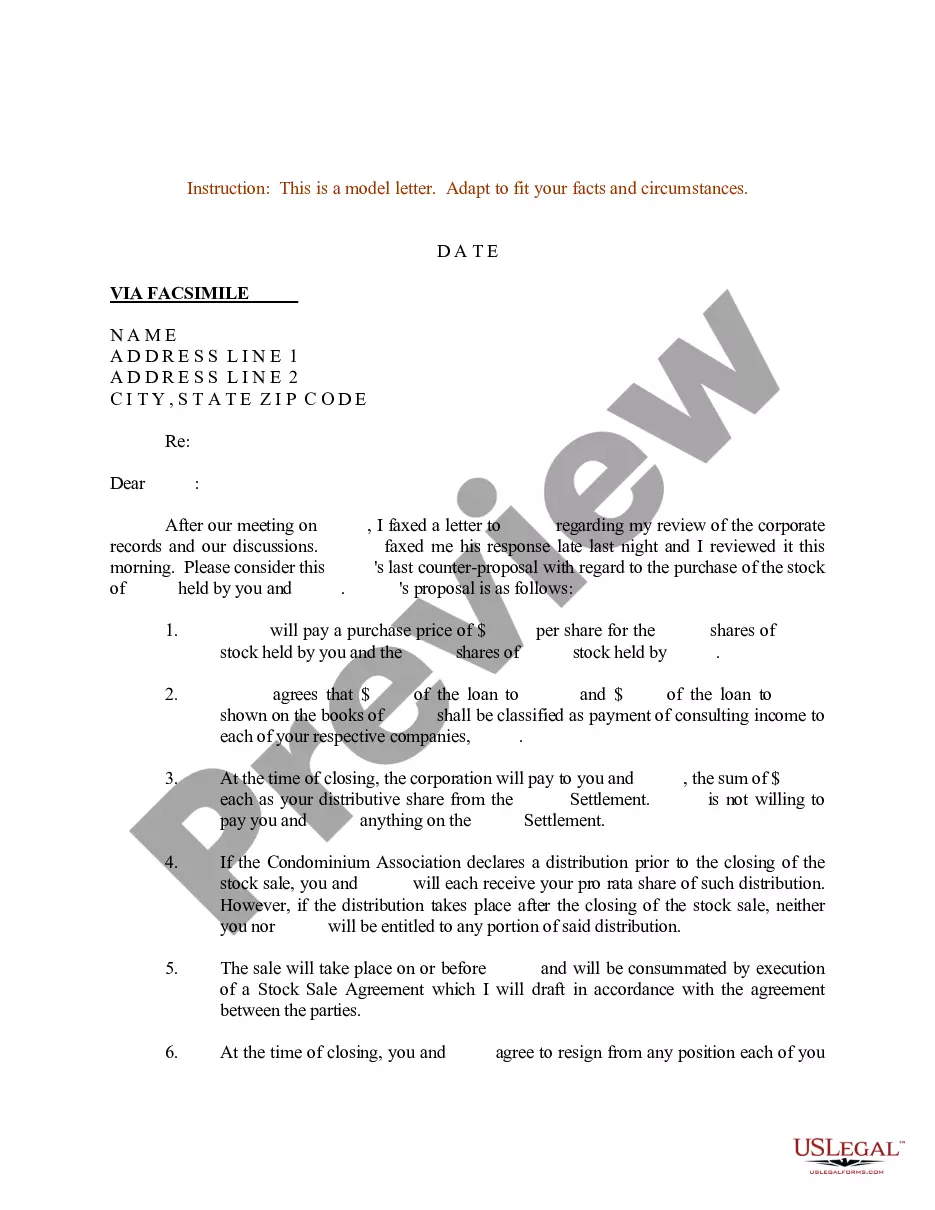
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
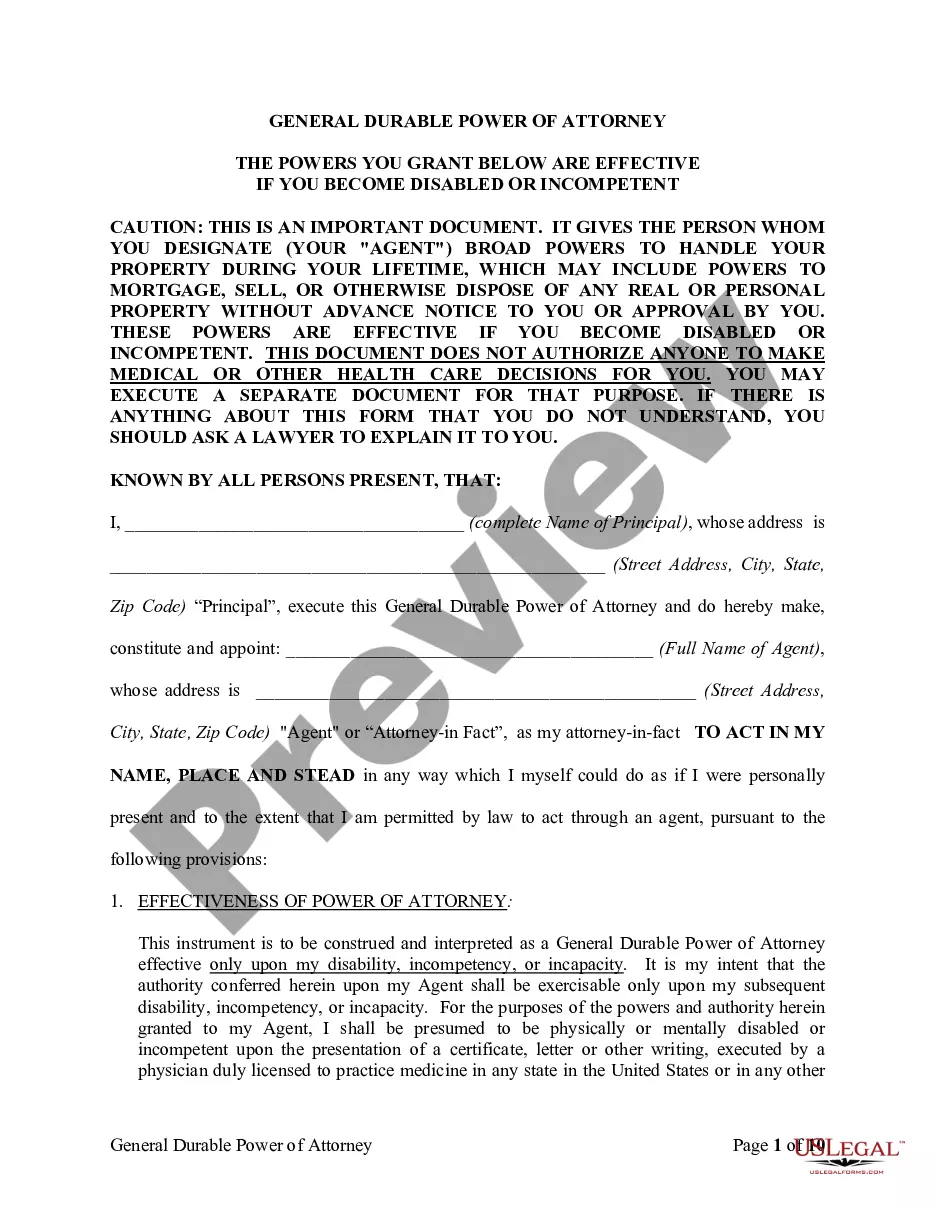
It is feasible to spend hours online searching for the official document template that fulfills the state and federal requirements you need.
US Legal Forms offers countless legal forms that are reviewed by experts.
You can easily download or print the California Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from your service.
If available, use the Preview button to browse through the document template as well.
- If you already have a US Legal Forms account, you can Log In and then click the Acquire button.
- After that, you can complete, modify, print, or sign the California Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
- Every legal document template you acquire is yours forever.
- To get another copy of the purchased template, go to the My documents tab and click the corresponding button.
- If you are using the US Legal Forms site for the first time, follow the basic instructions below.
- First, make sure you have chosen the correct document template for the state/area of your choice.
- Check the template details to ensure you have selected the right form.
Form popularity
FAQ
If you're losing health coverage. You must send documents showing the lost coverage and the date it ends. Acceptable documents include notices from your previous insurance company or your employer.
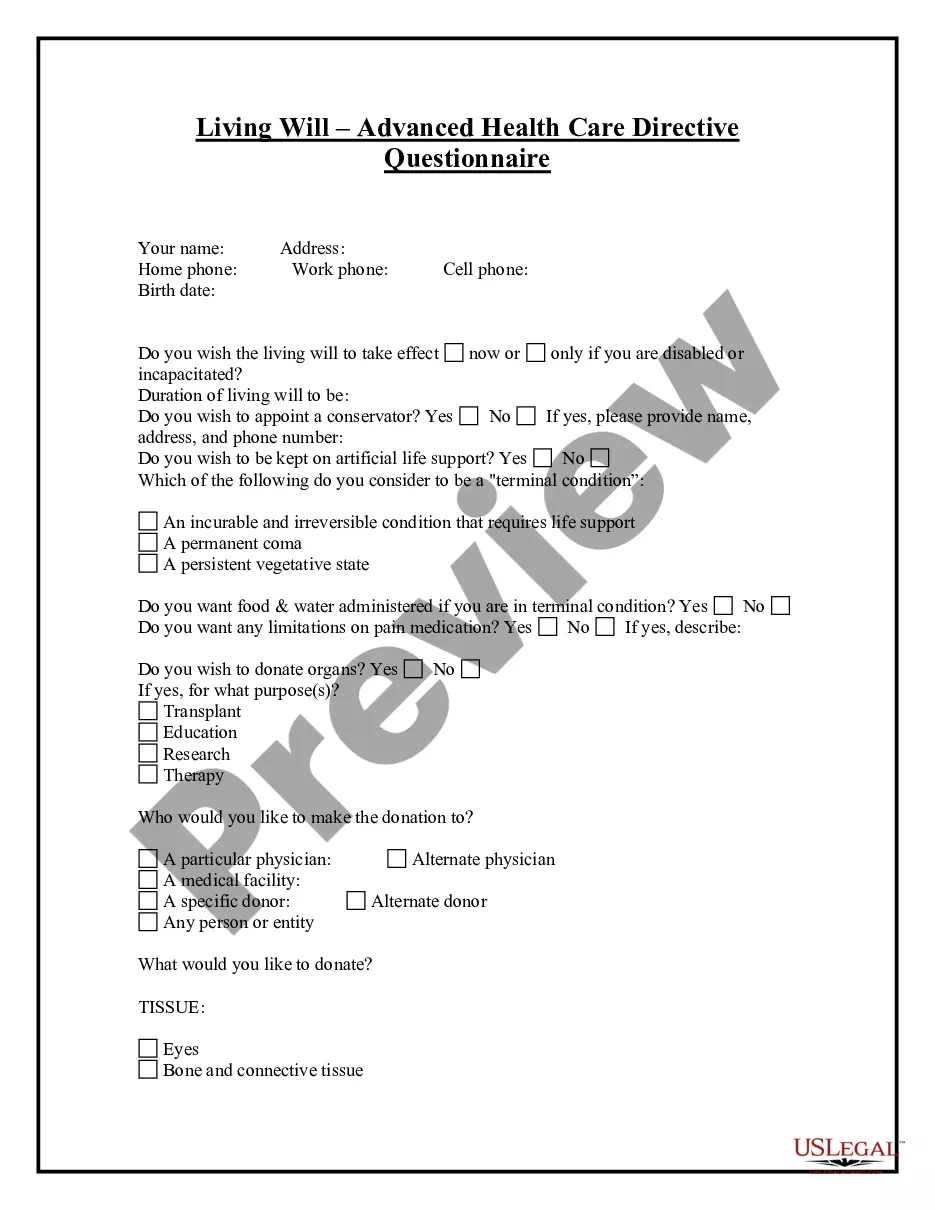
A coverage position letter is a letter communicating a coverage position to the insured. There are three basic types: Those letters that inform the insured there is a question of coverage. Those letters that inform the insured there is no coverage. Those letters that inform the insured there is no question of coverage.
Loss of Coverage means a complete loss of coverage under, or elimination of, a Component Plan or a Medical or Dental Plan, including the elimination of a Component Plan.
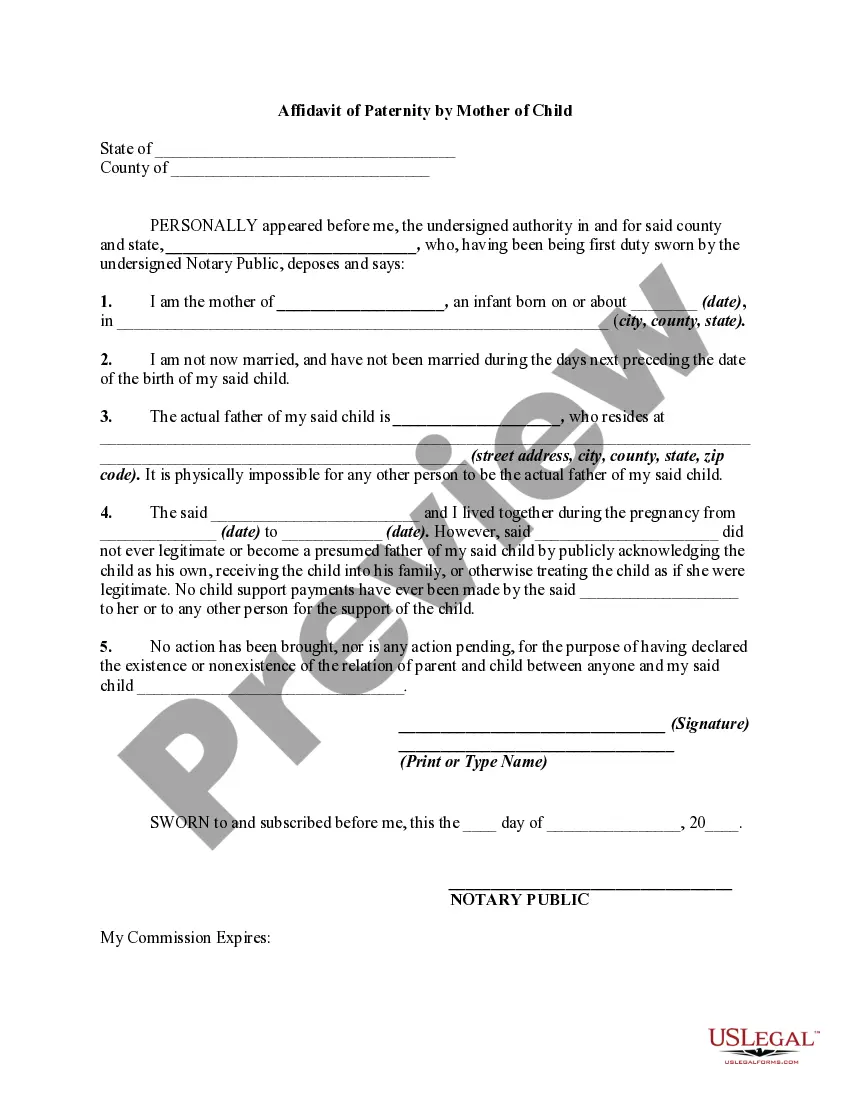
Time employee has to apply: 31 days after termination of existing coverage. Employers affected: Employers who offer group health insurance and have 2 to 19 (Does not affect employee's right to conventional continuation coverage pay insurance premiums for 3 months or for as long as employer continues to pay (3)2026
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
Loss of Coverage Letter Letter from your previous health carrier indicating an involuntary loss of coverage. The supporting document must indicate your name, the names of any dependents that were covered under the prior plan and the date the previous health coverage ended.
A letter from an employer, on official letterhead or stationery, that confirms one of these about you or your spouse or dependent family member:That your employer dropped or will drop your coverage or benefits. That your employer stopped or will stop contributing to your cost of coverage.