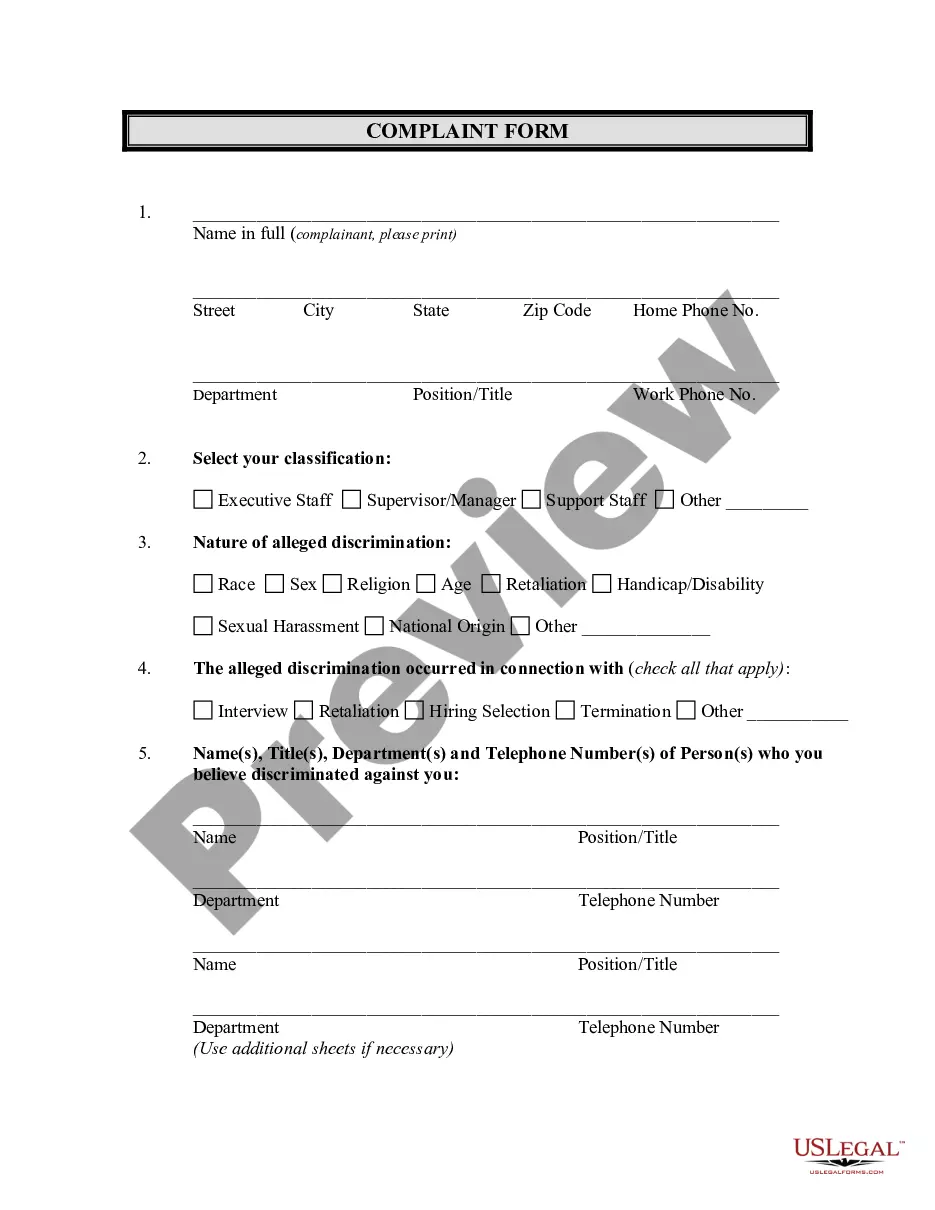
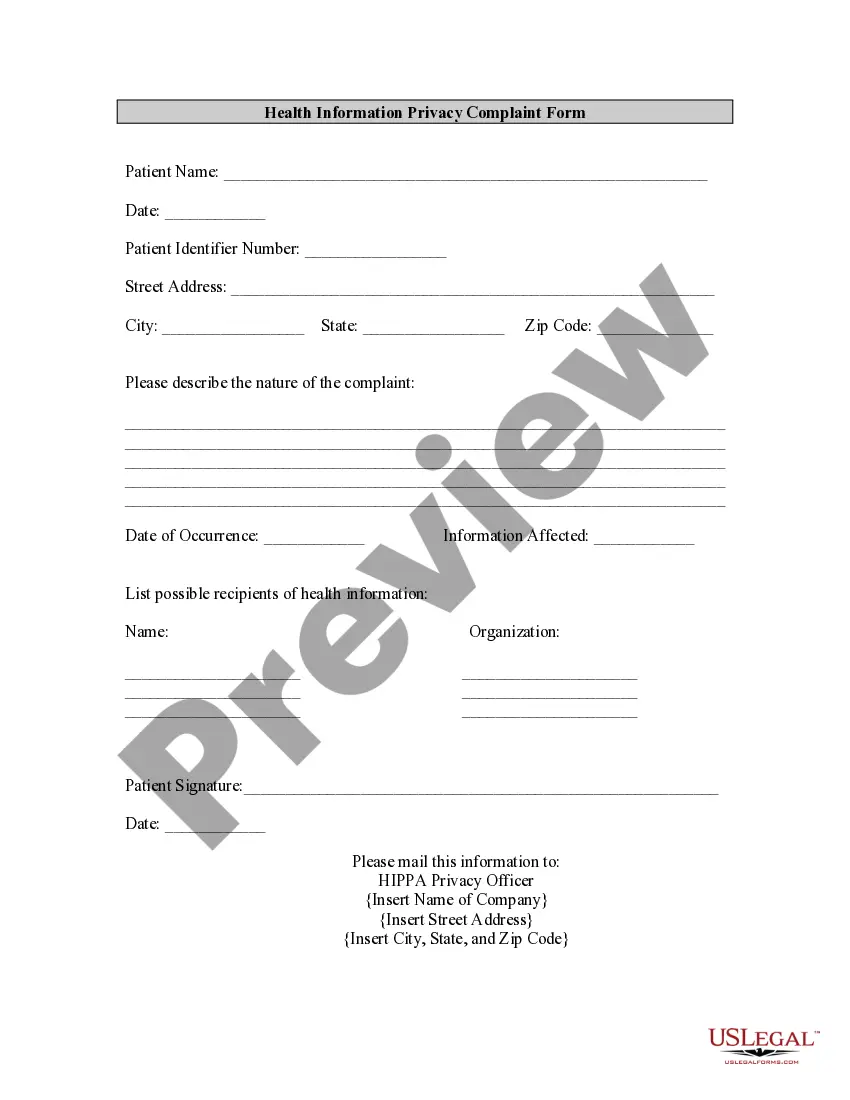
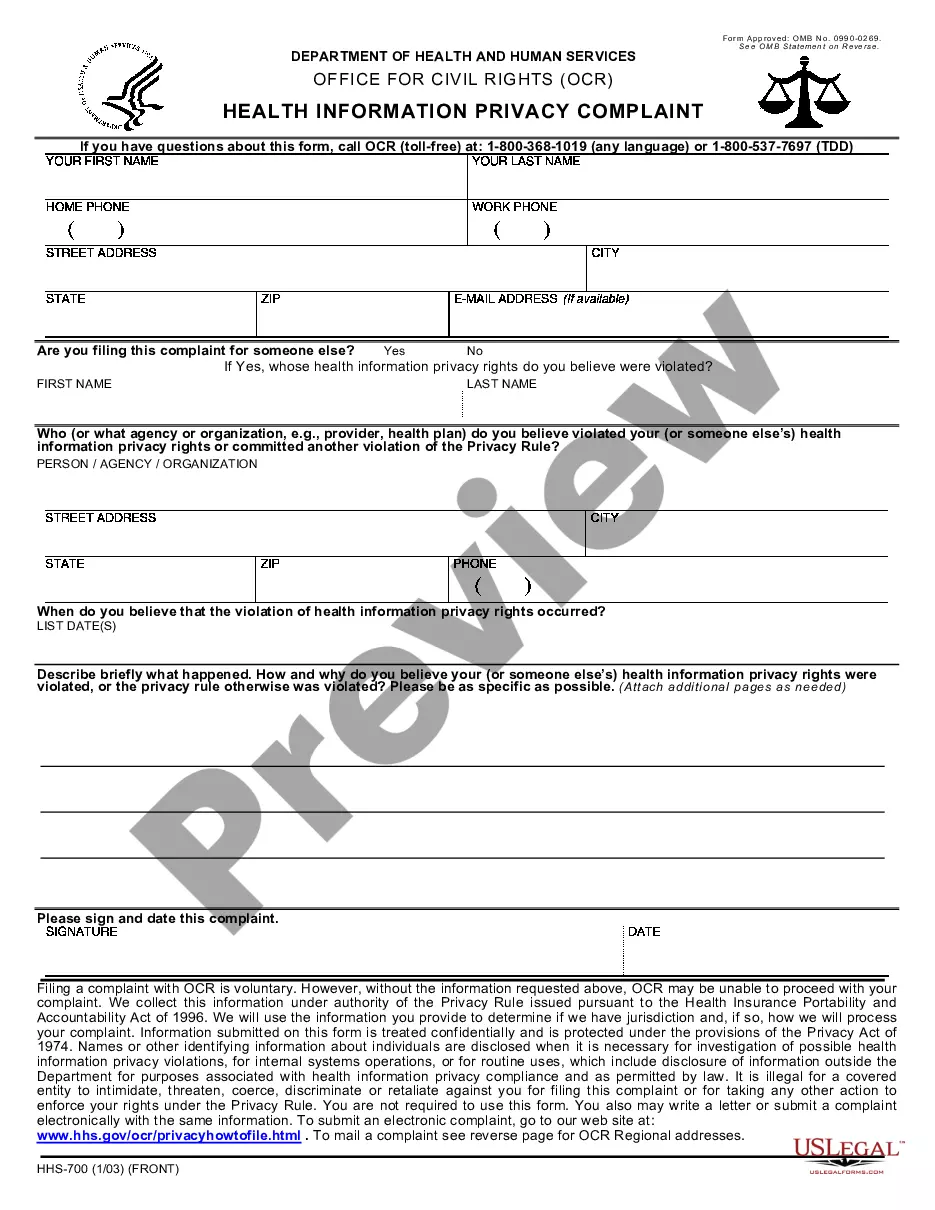
The California Utilization Review (UR) Complaint Form is a tool used by patients for filing grievances against UR decisions. The form seeks to provide a way for consumers to voice their grievances against a UR decision, which is a review of the medical necessity of a health care service or procedure. The form contains the date, patient information, provider information, UR decision being disputed, reason for disagreement, and any additional information that the patient may wish to add. There are two types of California Utilization Review (UR) Complaint Forms: a standard one-page complaint form and a more detailed two-page complaint form. Additionally, the California Department of Industrial Relations provides a list of frequently asked questions to help guide consumers through the complaint process.
California Utilization Review (UR) Complaint Form
Description
How to fill out California Utilization Review (UR) Complaint Form?
Completing formal documentation can be quite a hassle unless you have pre-prepared fillable templates at your disposal.
With the US Legal Forms online database of official documents, you can trust in the forms you acquire, as all of them adhere to federal and state laws and are verified by our specialists.
Here’s a brief guideline for you: Verification of document compliance. You should thoroughly review the form you wish to ensure it fits your needs and satisfies your state’s legal requirements. Reviewing your document and checking its general overview will assist you in this regard.
- Obtaining your California Utilization Review (UR) Complaint Form from our collection is straightforward.
- Existing users with an active subscription simply need to Log In and click the Download button once they locate the correct template.
- If needed, users can access the same form from the My documents section of their account.
- However, if you are a newcomer to our service, creating an account with a valid subscription takes just a few moments.
Form popularity
FAQ
To become a utilization review specialist, you typically need a background in healthcare, often including degrees in nursing or healthcare administration. Additionally, gaining experience in clinical settings and understanding health insurance policies is crucial. As you progress, consider exploring resources like the California Utilization Review (UR) Complaint Form to familiarize yourself with the documentation aspect of the field, enhancing your knowledge and skills.
To obtain a utilization certificate, you usually need to go through a specific process defined by your health insurance provider or the relevant regulatory authority. This often involves submitting a request along with necessary documentation to prove the medical necessity of prior treatments. If you have faced difficulties, the California Utilization Review (UR) Complaint Form can guide you in formally requesting the certificate.
A utilization review letter is a formal document that notifies a patient or healthcare provider about the outcome of a utilization review. It typically outlines whether the requested treatment is approved or denied, along with the reasons for the decision. If you receive a rejection, using the California Utilization Review (UR) Complaint Form can help you formally address and appeal the decision.
The basic three components of utilization review are the evaluation of the necessity of care, the appropriateness of the care provided, and the efficiency of the care delivery. Each component helps ensure that patients receive the right treatments at the right time, aligning care with medical standards. The California Utilization Review (UR) Complaint Form can be essential for documenting any concerns regarding these components in your healthcare experience.
Utilization review is indeed a required process for most workers' compensation claims in California. This mandatory review helps verify that proposed treatments are justified, helping to control expenses and providing guidance on the appropriate care for injured workers. By enforcing these reviews, the system aims to balance the needs of patients with the financial concerns of insurers. If you believe an unfair decision was made during this review, the California Utilization Review (UR) Complaint Form can assist you in voicing your complaint effectively.
Labor Code 4610 in California outlines the requirements for the utilization review process in workers' compensation claims. It establishes the criteria that insurers must follow when conducting these reviews and ensures that injured workers can access necessary medical treatments efficiently. This regulation aims to protect both the rights of patients and the integrity of the review process. For issues related to this code, the California Utilization Review (UR) Complaint Form can help clarify your requirements.
Yes, professionals conducting utilization reviews in California must be licensed and meet specific qualifications. These licenses require a background in healthcare or relevant experience, ensuring that only qualified individuals perform these critical evaluations. Proper licensing helps maintain a high standard of care for injured workers. Should you encounter a licensing issue, the California Utilization Review (UR) Complaint Form may provide a pathway to address it formally.
In California, insurers have 90 days to make a decision regarding a workers' compensation claim. This timeframe allows for a thorough review of the claim and any necessary evaluations of medical evidence. Responding promptly within this period is crucial to ensuring that injured workers receive timely benefits. If you feel the waiting period is taking too long, consider utilizing the California Utilization Review (UR) Complaint Form to address these concerns.
The utilization review process serves to assess the medical necessity and appropriateness of treatments requested in workers' compensation cases. Its primary aim is to ensure that care provided aligns with established guidelines, thereby guaranteeing the best outcomes for injured workers. This scrutiny helps manage costs effectively for insurance companies while also safeguarding patients. If you encounter challenges during this review, the California Utilization Review (UR) Complaint Form can be a valuable tool to raise your concerns.
The 90 day rule in California mandates that workers' compensation claims must be resolved within 90 days. This rule applies to the time from when the claim is filed until a determination is made about the injured worker's benefits. If the decision isn't reached within this timeframe, the claim may be considered accepted. If you have concerns about a delayed decision, the California Utilization Review (UR) Complaint Form provides a structured way to communicate those issues.