California Providers Request For Second Bill Review
Description
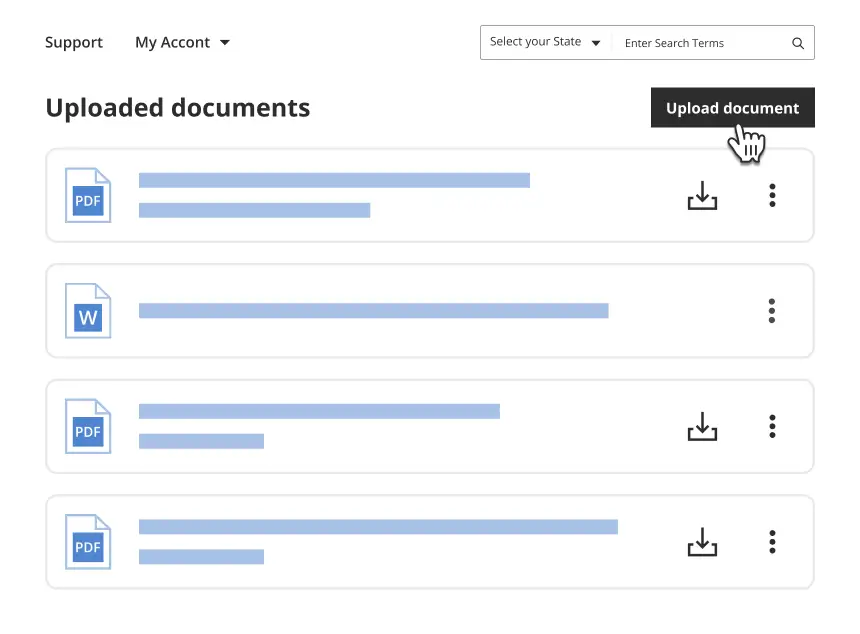
Get your form ready online
Our built-in tools help you complete, sign, share, and store your documents in one place.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Looking for another form?
How to fill out California Providers Request For Second Bill Review?
How much duration and resources do you frequently expend on creating formal documentation.
There’s a superior method to acquire such forms than employing legal professionals or investing hours navigating the web for an appropriate template. US Legal Forms is the premier online repository that provides expertly crafted and validated state-specific legal documents for any purpose, such as the California Providers Request For Second Bill Review.
Another advantage of our library is that you can access previously downloaded documents that you securely store in your profile in the My documents tab. Retrieve them anytime and re-complete your documentation as often as necessary.
Conserve time and energy completing legal documentation with US Legal Forms, one of the most reliable web solutions. Sign up with us now!
- Examine the form content to ensure it adheres to your state regulations. To do this, verify the form description or utilize the Preview option.
- If your legal template does not fulfill your requirements, search for another one using the search bar located at the top of the page.
- If you are already registered with our service, Log In and download the California Providers Request For Second Bill Review. Otherwise, continue to the next steps.
- Click Buy now once you locate the correct blank. Choose the subscription plan that best fits you to access the full benefits of our library.
- Register for an account and complete your subscription payment. You can settle the payment with your credit card or via PayPal - our service is entirely secure for that.
- Download your California Providers Request For Second Bill Review onto your device and fill it out on a printed hard copy or electronically.
Form popularity
FAQ
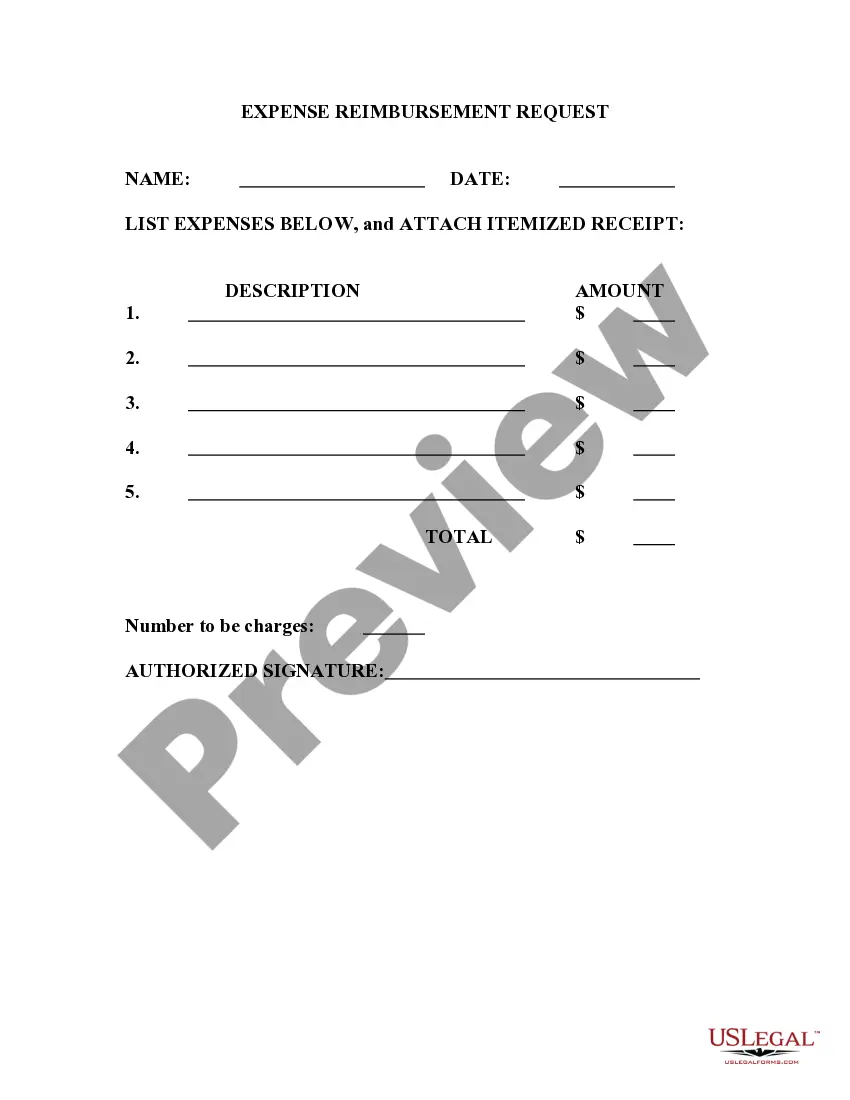
Challenging balance billing involves gathering all relevant documentation, including your bill and insurance statements. Communicate directly with the provider to address any inaccuracies. If your efforts do not yield results, you can escalate your case by contacting a consumer protection agency. Remember, California Providers Request For Second Bill Review can help streamline this process and provide essential support.
To fight balance billing in California, examine your bill carefully and verify your insurance coverage. Engage with your insurance provider to understand their payment terms and negotiate discrepancies with the hospital or provider. You can also file a complaint with the California Department of Managed Health Care if necessary. Using California Providers Request For Second Bill Review can strengthen your position in resolving these issues effectively.
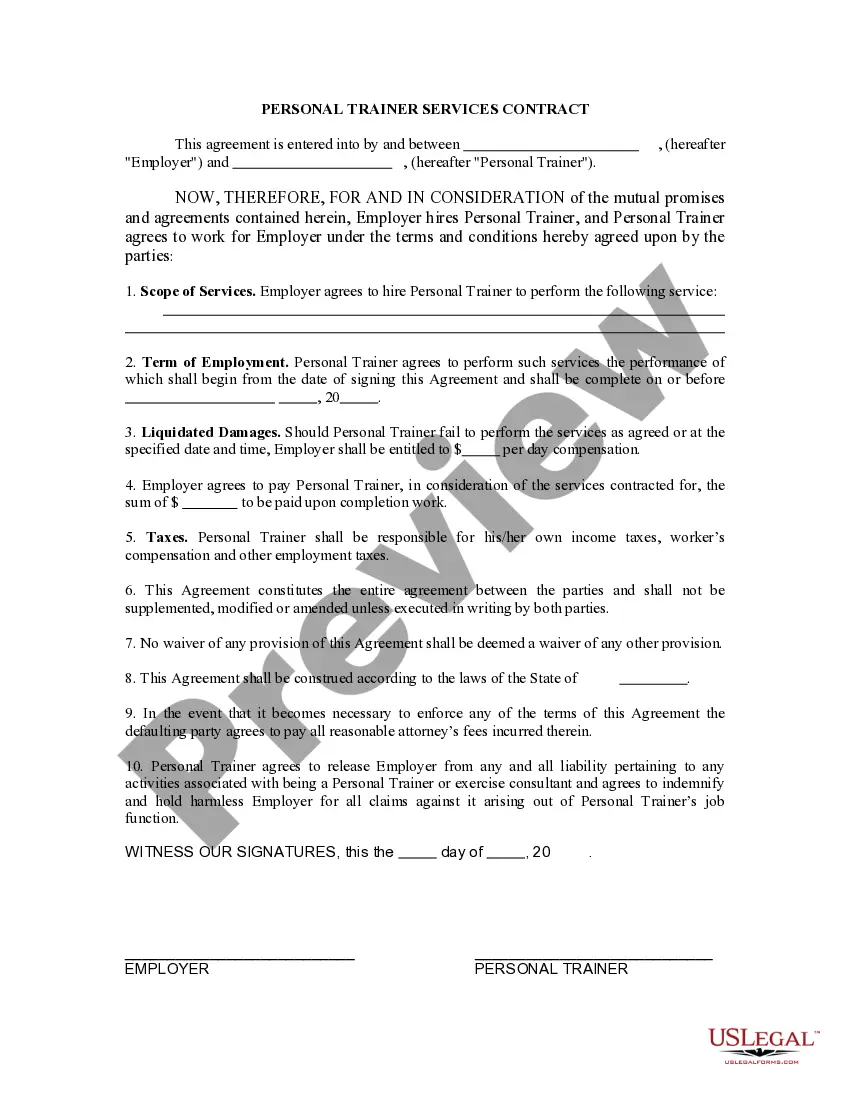
The prohibition on balance billing refers to laws that prevent healthcare providers from billing patients for the difference between their billed charges and what insurance covers. In California, this applies primarily to emergency care and certain in-network situations. This regulation protects patients from unforeseen high costs. If you need assistance with understanding this process, California Providers Request For Second Bill Review can offer valuable insights.
Yes, California prohibits balance billing under specific circumstances, especially for emergency services. This applies to patients who receive care from out-of-network providers without consent. It ensures that patients are not responsible for the difference between what their insurance pays and the total bill. For more information, consider resources related to California Providers Request For Second Bill Review for navigating these complex situations.
Fighting unfair medical bills starts with a thorough review of your charges and insurance coverage. Compare your bill with the Explanation of Benefits from your insurance company. If discrepancies arise, you can contact the billing department to discuss corrections. Additionally, utilizing California Providers Request For Second Bill Review may help in advocating for more accurate assessments.
In California, a hospital cannot bill you two years after the service date due to the statute of limitations. This law limits the time during which a provider can pursue payment for services rendered. However, it's essential to review your specific situation carefully. To protect yourself, consider using California Providers Request For Second Bill Review to ensure accuracy in your billing.
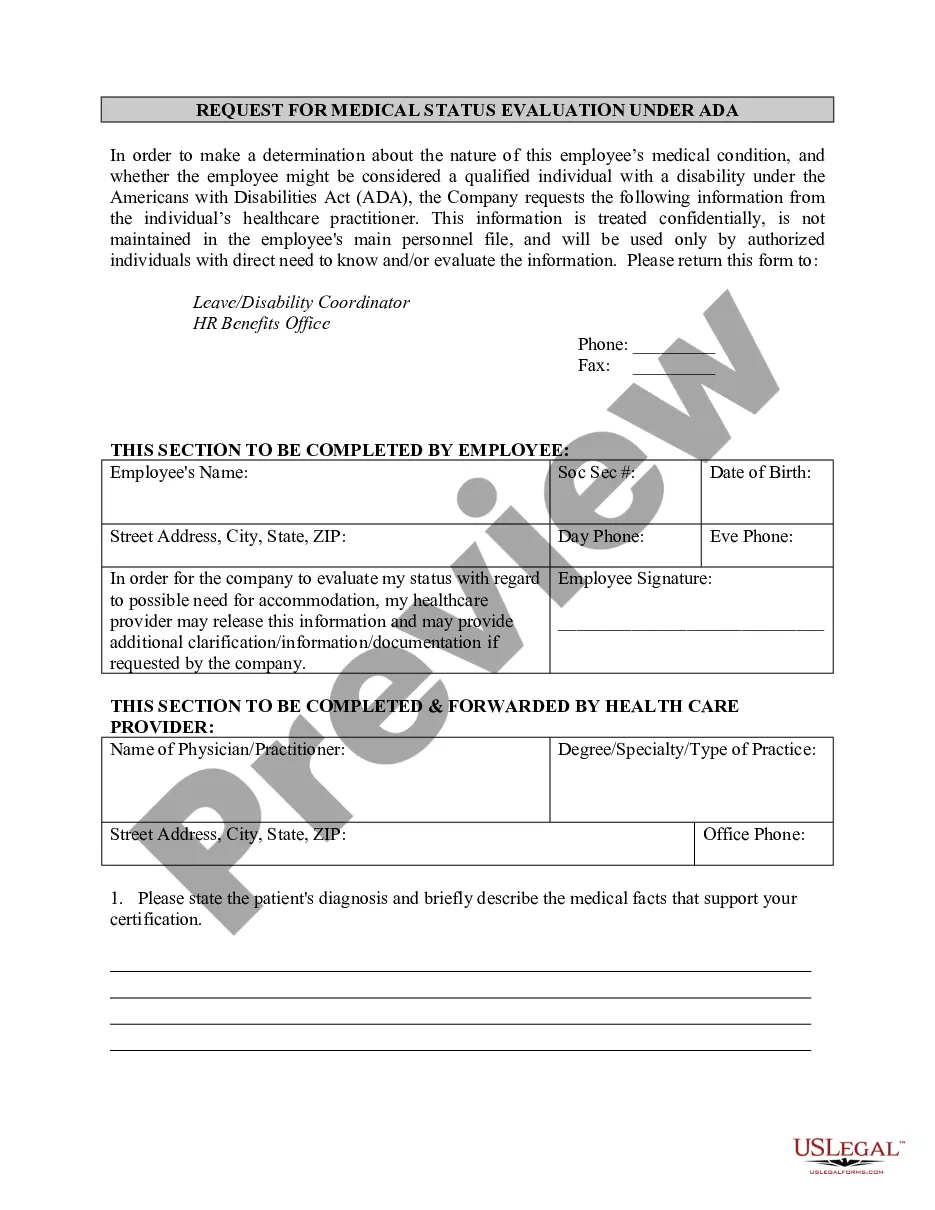
In California, those conducting utilization reviews must have specific licenses or certifications as defined by state regulations. The licensing ensures that reviewers have the necessary expertise to perform fair evaluations of treatment requests. Providers seeking clarity on denied treatments can find support through the California Providers Request For Second Bill Review process.
Rule 9785 sets forth specific requirements related to the review of medical treatment requests in California's workers' compensation system. This rule specifies how the review process should be conducted, ensuring fairness and transparency. Awareness of this rule is beneficial for providers who might need to engage in the California Providers Request For Second Bill Review to address discrepancies in treatment approvals.
Labor Code 4610 in California outlines the regulations surrounding utilization review for workers' compensation claims. It establishes the framework for medical treatment guidelines, including timelines for reviews and required documentation. Being familiar with this code can assist providers in navigating disputes and utilizing the California Providers Request For Second Bill Review effectively.
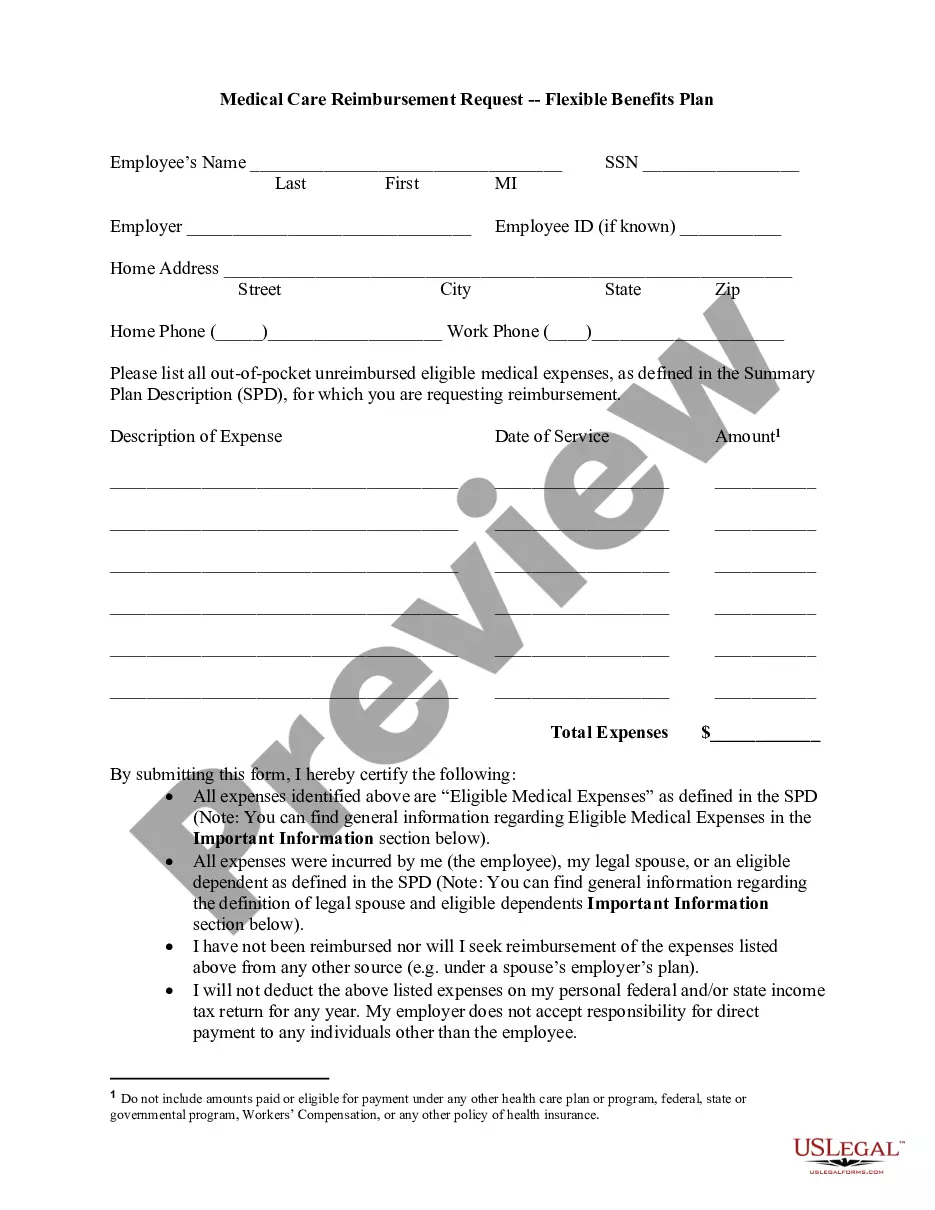
The medical bill review process involves a thorough examination of medical bills submitted by healthcare providers to determine their accuracy and necessity. Various steps include verifying patient eligibility, assessing medical services rendered, and ensuring compliance with applicable laws. Understanding this process is crucial for providers having issues with bill payments and looking to utilize the California Providers Request For Second Bill Review.